1 5
t h
I n t e r n a t i o n a l C o n f e r e n c e o n
Immunology
Journal of Clinical Immunology and Allergy
ISSN 2471-304X
J u l y 0 5 - 0 7 , 2 0 1 8
V i e n n a , A u s t r i a
Immunology 2018
Page 28
T
wo patients presented with a history of anaphylaxis (one with loss of
consciousness, the other with laryngeal edema, urticaria, angioedema, and
near syncope) immediately after eating chapuline from Oaxaca, Mexico. Prick
puncture testing to grasshopper antigen was 4+ in both patients and negative
in five non-allergic controls. Both patients gave a prior history of urticaria/
angioedema/laryngeal edema following ingestion of crustaceans.
In vitro
IgE
specific antibodies to crustaceans, dust mites, and cockroach were positive in
both patients. Total IgE was greater than 2000 IU/mL in one patient, and 92.6 IU/
mL in the other (nl<87 IU/mL). Tryptase levels in both patients were not elevated.
Specific IgE inhibition studies reveal that grasshopper extract contains antigens
capable of binding to patient's specific IgE to crustaceans, cockroach, and mites,
indicating the presence of a cross reacting pan-allergen in grasshopper extract.
Immunoblot analysis of the grasshopper extract revealed the presence of a 30
kD molecular weight protein in grasshopper and chapuline and a 38 kD molecular
weight protein in shrimp, which bound patient-specific IgE antibody. Western Blot
analysis of the extract probed with anti-tropomyosin antibody revealed those
antigens to be tropomyosin. Although previous reports in the literature of allergic
rhinoconjunctivitis, contact urticaria, and asthma after inhalation of grasshopper
are well known, this is the first well-documented report of anaphylaxis following
ingestion of grasshoppers. Ingestion of insects is very popular in Asia, the Middle
East, South and Central America, and particularly in Mexico and in Southern
California. The purpose of this report is to alert the medical community and
the public to the fact that there is an increased risk of allergic reactions to the
ingestion of grasshoppers in patients with a prior history of crustacean, house
dust mite, and/or cockroach allergy.
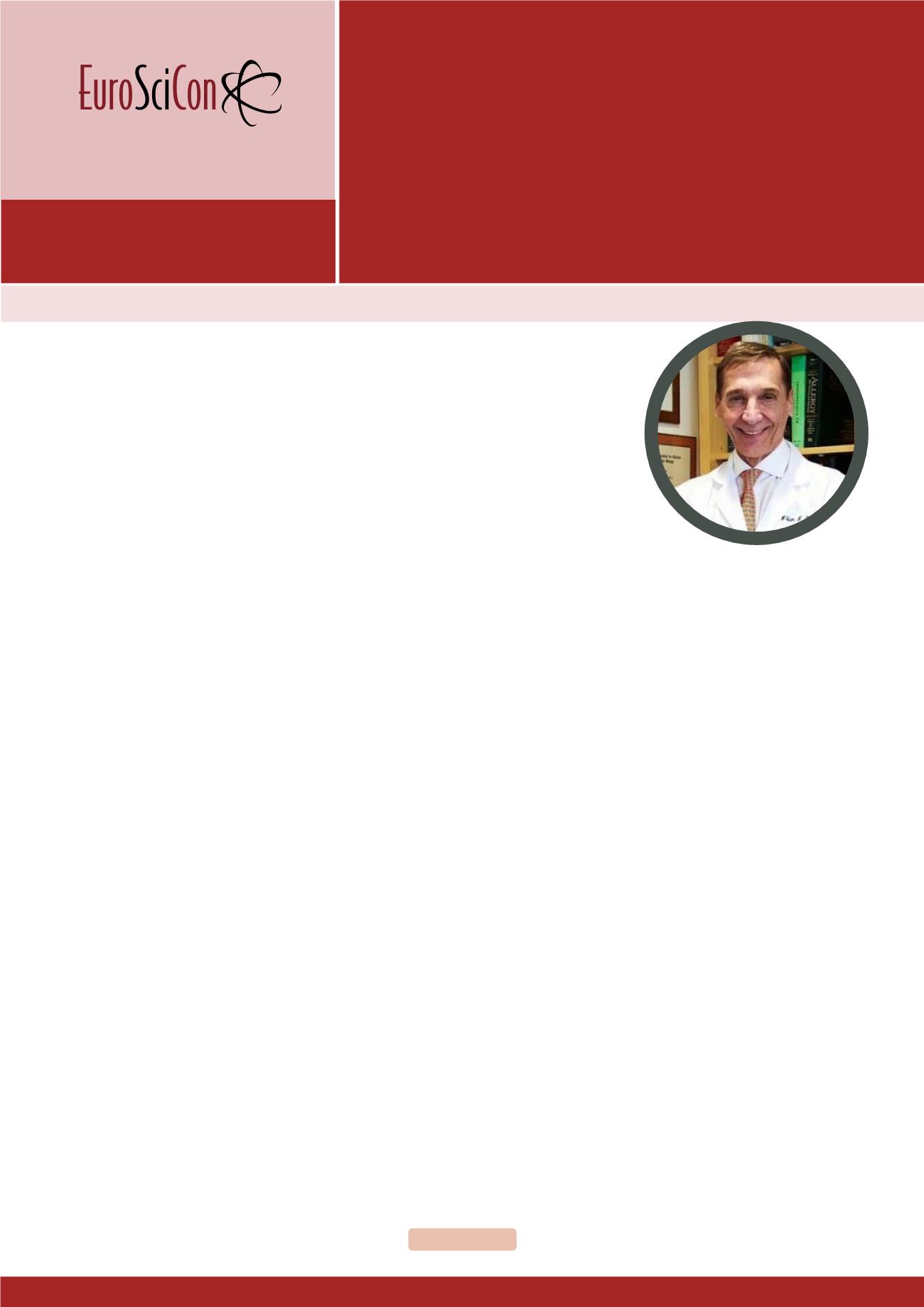
Biography
William N Sokol was a board certified Internist (Northwestern)
and Allergist (UCLA). He completed Undergraduation (BA) from
Ohio State University (AED pre-Med honorary). Ohio State Col-
lege of Medicine (Landacre research society award). He joined
the clinical faculty of the division of Allergy at the University of
California at Irvine immediately after his fellowship and current-
ly a Clinical Professor of Immunology and Allergy at U C I where
he give the basic immunology lectures to Medical Students
and supervise training of Allergy fellows, including guiding their
research efforts. His fields of interest have included basic re-
search on β-adrenergic cell membrane receptors which result-
ed in several papers which contributed in part to the refutation
of the β-blockade theory of the origin of asthma. Subsequent
interests involved the descriptions of a several new causes of
occupational asthma and clinical research on bacterial sinus-
itis, asthma, rhinitis and several new causes of anaphylaxis. He
has published over 50 articles in the peer reviewed medical lit-
erature. His most recent work is on the description of a 30 kD
tropomyosin found in a type of grasshopper called chapulines
which are commonly ingested in Mexico and the USA. This di-
etary peculiarity is causing allergic reactions including anaphy-
laxis in unsuspected patients with underlying crustacean HDM
and cockroach allergy.
wsokolallergy@aol.comAnaphylaxis after first ingestion of
chapulines (grasshopper) in patients
allergic to house dust mite, cockroach, and
crustaceans, is tropomyosin the cause?
William N Sokol
University of California, California, USA
William N Sokol, Insights Allergy Asthma Bronchitis 2018, Volume: 4
DOI: 10.21767/2471-304X-C1-001