Volume 4
Journal of Pediatric Care
ISSN: 2471-805X
Page 49
JOINT EVENT
May 07-08, 2018 Frankfurt, Germany
&
3
rd
International Conference on
Pediatrics and Pediatric Surgery
22
nd
Edition of International Conference on
Neonatology and Perinatology
Successfully treated
Candida
infection of ventriculo-peritoneal shunt in an extremely low birth weight
infant
Vittoria Rizzo
Maurizio Bufalini Hospital- Cesena, Italy
I
nfection is a common complication of ventriculo-peritoneal (VP) shunt placement. Candida is a rarely implicated.
Most authors consider device removal necessary to clear infection. Jans reported high caspofungin levels in cerebro-
spinal fluid (CSF) and successful treatment of a neonatal VP shunt-associated Candida meningitis adding caspofungin to
standard antifungal treatment. A preterm female (GA24 weeks, BW 708 gr) developed, on day 14, late onset GBS sepsis with
ultrasonographic evidence of ventriculitis. Lumbar puncture was not performed because of clinical instability. She received a
16 days course of antibiotics plus fluconazole prophylaxis. Despite clinical improvement, progressive hydrocephalus occurred.
On day 46, antibiotic-impregnated VP shunt with Ommaya was inserted, with 3 days prophylactic linezolid and cefotaxime.
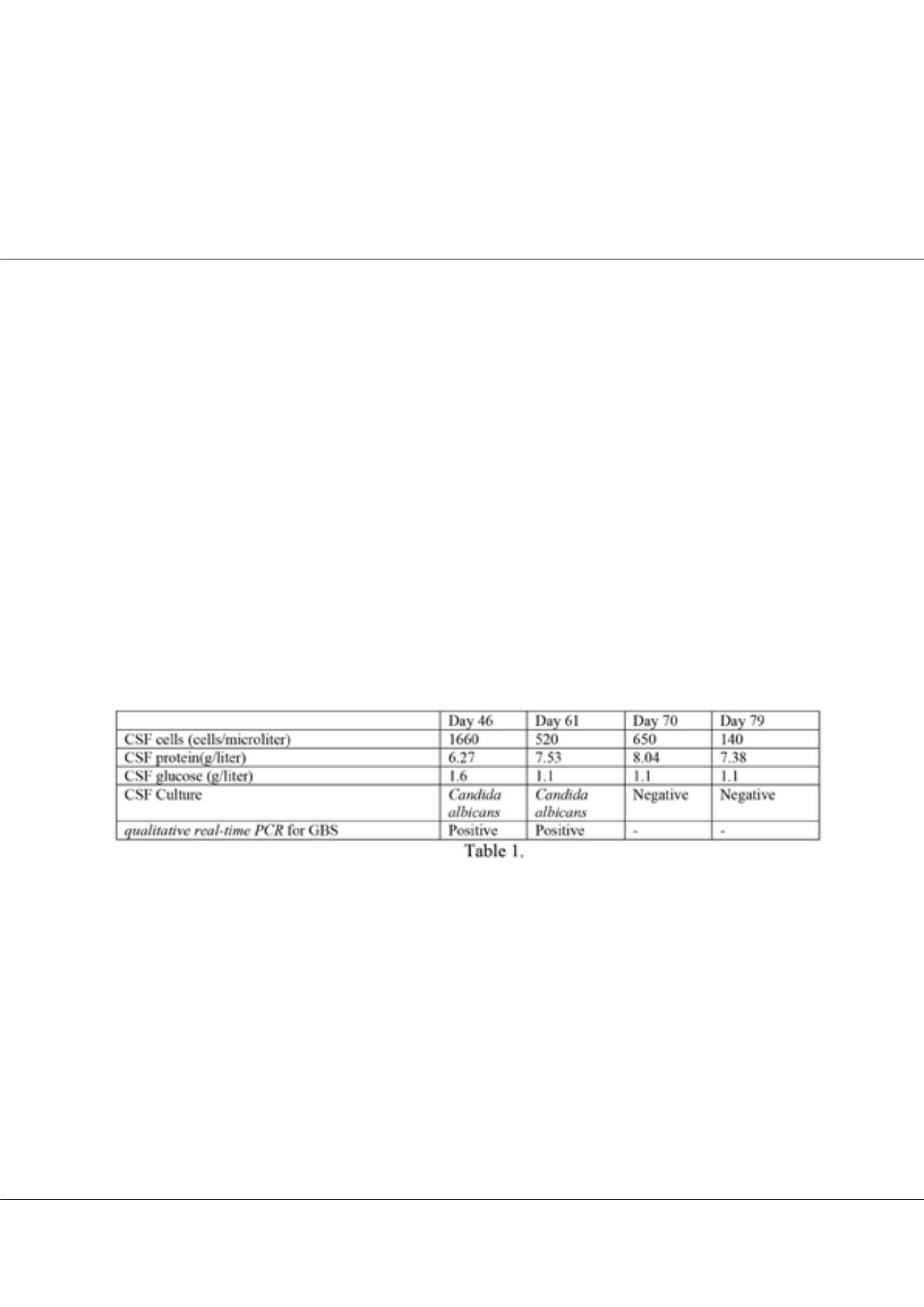
CSF taken during surgical procedure (see table 1) grew Candida albicans susceptible to fluconazole, voriconazol, amphotericin
B; qualitative real-time PCR for GBS was positive. Ampicillin (300 mg/kg/day) and fluconazole (6 mg/kg/day) were started.
Fifteen days later, CSF showed moderate response to treatment but colture was sill positive for Candida albicans. After 3
weeks, the baby had poor weight gain, unchanged ventricular size despite VP shunt, worsening of pleiocitosis and raised CSF
proteins, with negative colture. Intravenous caspofungin (25 mg/m2/day) was added and ampicillin stopped (we assumed PCR
detection of GBS not indicative of active infection). After a 9 days on caspofungin, there were clinical improvement, reduction
of ventricles size, sterile CSF, reduced pleiocitosis and CSF proteins. Fluconazole and caspofungin were discontinued. The
baby recovered, without the need for shunt replacement, and was discharged home on day 90. VP shunt was replaced only 18
months later because of malfunctioning.
Caspofungin, probably due to its specific action on fungal biofilm, can achieve resolution of VP shunt-associated Candida
albicans infections, avoiding shunt and reservoir substitution.
Bibliography
1. Baradkar V P, Mathur M, Sonavane A, and Kumar S. Candidal infections of ventriculoperitoneal shunts J Pediatr
Neurosci. 2009 Jul-Dec; 4(2): 73–75. doi: 10.4103/1817-1745.57325
2. Kojic EM, Darouiche RO. Candida infection of medical devices. Clin Microbiol Rev. 2004;17:255–67. [PMCID:
PMC387407] [PubMed: 15084500]
3. Jans J, Brüggemann RJM, Christmann V, Verweij PE,WarrisaA. Favorable Outcome of Neonatal Cerebrospinal Fluid
Shunt-Associated Candida Meningitis with Caspofungin May 2013 Volume 57 Number 5 Antimicrobial Agents and
Chemotherapy p. 2391–2393.
Biography
Vittoria Rizzo works at PICU-NICU in “Maurizio Bufalini” Hospital Cesena-Italy. She has a special interest in Neonatal Infections. She has published more than 20
papers in reputed journals, of which 8 in international Journals.
vittoria.rizzo@auslromagna.itVittoria Rizzo, J Pediatr Care, Volume 4
DOI: 10.21767/2471-805X-C2-009
















