Zinner Syndrome-Developmental Anomaly of Mesonephric Duct (Case Report)
Papava V1, Didbaridze T2*, Tsirekidze M3, Kvakhajelidze V1, Mamasakhlisi T4, Sinauridze G5, Shanidze L6 and Zaalishvili Z7
1 Department of Urology, Tbilisi State Medical University, Tbilisi, Georgia
2 Department of Microbiology, Tbilisi State Medical University, Tbilisi, Georgia
3 Department of Radiologist, Tbilisi State Medical University, Tbilisi, Georgia
4 Department of Internal Medicine, Tbilisi State Medical University, Tbilisi, Georgia
5 Department of Caraps Medline, Tbilisi State Medical University, Tbilisi, Georgia
6 Manager of the Georgian-Austrian Medical Centre, Tbilisi State Medical University, Tbilisi, Georgia
7 American program of Tbilisi State Medical University, Tbilisi, Georgia
- *Corresponding Author:
- Didbaridze T
Department of Microbiology,
Tbilisi State Medical University,
Tbilisi,
Georgia;
E-mail: t.didbaridze@tsmu.edu
Received Date: September 23, 2021; Accepted Date: September 30, 2021; Published Date: October 14, 2021
Citation: Papava V, Didbaridze T, Tsirekidze M, Kvakhajelidze V, Mamasakhlisi T, et al. (2021) Zinner Syndrome-Developmental Anomaly of Mesonephric Duct (Case Report). J Nephrol Urol. Vol.5 No.4:16.
Abstract
Zinner syndrome is developmental anomalies of the urogenital tract are rare but often encountered. This condition is caused by disrupted embryonic development of the genitourinary system. Only approximately a 100 cases have been reported so far. Most patients with this anomaly are asymptomatic. Radiologic modalities such as intravenous pyelography, ultrasonography, vasovesiculography, contrast enhanced computed tomography, and magnetic resonance imaging are all helpful in diagnosis of this unusual entity. We reported a case of Zinner syndrome, one of the rarest genitourinary system anomalies. Ultrasound as well as CT and MRI can easily detect the abnormalities specific for Zinner syndrome. Asymptomatic patients require active follow-up while symptomatic patients with enlarging seminal vesicle cyst require surgical intervention such as perineal cyst aspiration, subcutaneous cyst drainage, laparoscopic, and open surgery. Male patients need to be followed up for infertility. Our patient is asymptomatic. Therefore, he requires an active follow-up.
Keywords
Magnetic Resonance Imaging (MRI); Computed Tomography (CT); Asymptomatic man; Genitourinary system
Introduction
Zinner syndrome is a rare congenital anomaly characterized by renal agenesis, the ipsilateral seminal vesicle cyst, and the obstruction or dilation of vas deferens. This condition is caused by disrupted embryonic development of the genitourinary system. Zinner syndrome was first described by Zinner in 1914 which is why the syndrome is named after him [1]. Only a few hundred Zinner syndrome cases are reported in the medical literature [2]. This condition belongs to the rarest anomalies of the genitourinary tract and is diagnosed in the second to fourth decade of life [3]. Most patients with this anomaly are asymptomatic. The patients with Zinner syndrome, are usually diagnosed in the 2nd-3rd decade of life They are developmentally normal, may report decreased urine output, increased urinary frequency, perineal pain, and ejaculatory dysfunction. Diagnostic evaluation includes CT, ultrasound, MRI, urogenital X-ray, urodynamic studies, and laboratory tests. It is considered to be the male counterpart of Mayer-Rokitansky-Kuster-Hauses syndrome seen in females [4]. An insult occurring before the 7th gestation week causes maldevelopment of the distal part of the mesonephric duct producing atresia of both ejaculatory duct and the ureteric bud [5].
The close embryologic relationship between the genital and urinary tracts explains the developmental aberrations leading to this anomaly. The Mesonephric or Wolffian duct, which forms the male reproductive system as well as the ureteric bud, is a paired structure. The orifice of the distal mesonephric duct and the ureteric bud separates between 6th-8th gestational week, and the ureteric orifice migrates toward the metanephric blastema, whereas the distal part of mesonephric duct under the influence of testosterone and anti-Mullerian hormone, forms the hemitrigone, the bladder neck, the urethra up to the external sphincter, the seminal vesicle, vas deferens, ejaculatory ducts, epididymis, paradidymis, and appendix of the epididymis [6,7]. During the 4th to 6th week of gestation, the metanephric blastema secretes growth factors, which induce the growth of the ureteric bud toward it. The ureteric bud too secretes growth factors and proliferates, fusing with the metanephric blastema, and in turn inducing the blastema to become the primitive kidney on undergoing mesenchymal to epithelial transition [8].
Imaging enables accurate diagnosis of this rare anomaly of the genitourinary tract. On sonography, ipsilateral kidney is absent, and the obstructed ejaculatory ducts are seen as anechoic structures in the pelvis, though hemorrhage or infection can produce internal low level echoes [9]. CT is better than sonography, and CT findings are of a retrovesicular periprostatic cystic mass along with ipsilateral renal agenesis [10]. Aspiration of cyst fluid transperineally and identification of spermatozoa in it is also confirmatory for Zinner's syndrome.
Surgical aspiration of the seminal vesicle cysts through perineal or laparoscopic approach or percutaneous cyst drainage or a transurethral cyst deroofing is considered therapeutic and by relieving the ejaculatory duct obstruction provides excellent cure and symptomatic relief (100% and 75%, respectively) [11]. Infertility results from ejaculatory duct obstruction and when obstruction is released, fertility is restored.
We present an uncommon case of a 17-year-old asymptomatic patient which the initial presentation of bilateral pneumonia.
Case Presentation
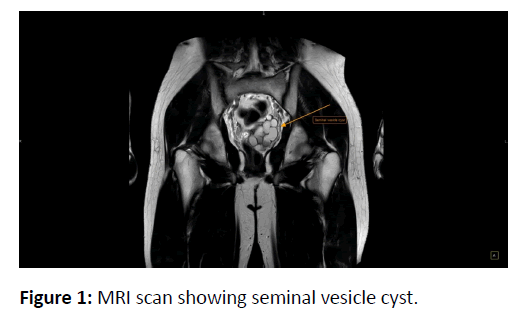
A 17-year-old man was admitted to the clinic in October 2017 and was diagnosed with bilateral pneumonia. Several days after admission, dysuria and urinary dribbling were noted prompting the patient's referral to the urologist. The patient did not report any other urinary symptoms in the past. The physical exam revealed the non-palpable kidneys along with negative costovertebral angle tenderness. Both testes were palpable in the scrotum. However, the palpation of the left-sided spermatic cord revealed the wider, dense vas deferens. Serum creatinine and the urinalysis of the patient were non-significant (Figure 1.).
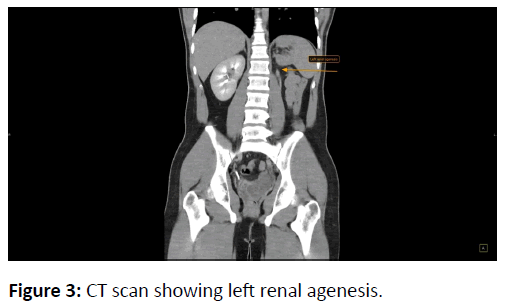
The testicular ultrasound showed homogenous testes with normal echogenicity and a testicular volume of 12 cm3. The leftsided vas deferens kinked without dilation of pampiniform plexus. The pelvic ultrasound revealed a severely kinked, nonhomogenous, fluid-containing structure with a maximal diameter of 30 mm on the left posterior side of the bladder. The seminal vesicles were not visualized. The ultrasound and the CT showed a mildly enlarged right-sided kidney with normal parenchyma and a non-dilated collecting system. The left-sided kidney was hypoplastic and was associated with a long, tubular structure with an uneven diameter and a thickness of 1 cm. This structure is proximally connected to the left kidney suggesting that it is the left-sided ureter. The contrast was not excreted in the left-sided ureter.
MRI of the genitourinary system revealed the asymmetric seminal vesicles. While the right seminar vesicle had normal size and structure, the left seminal vesicle contained the multiloculated cyst with non-homogenous, proteinaceous, and hemorrhagic fluid inside.
The patient was counseled on the ambulatory follow-up in 2017 but he has not attended the follow-up visits until 2021. In 2021, he reported urinary dribbling at least twice a day. The urinary and scrotal ultrasound was performed again which showed a kinked structure with non-homogeneous fluid and a maximal diameter of 34 mm on the left posterior side of the bladder. Seminal vesicles were not visualized.
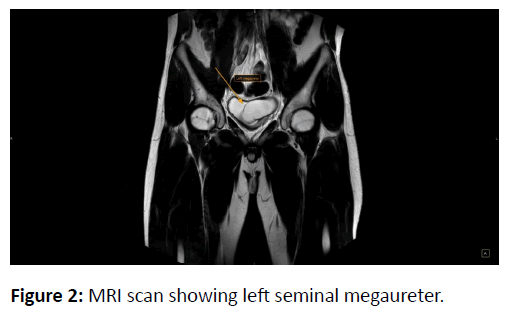
Repeat serum creatinine and urinalysis were still nonsignificant. Spermogram revealed normospermia. Sperm culture did not yield any growth. PSA was 0.50 ng/dL. Repeat MRI revealed the asymmetric seminal vesicles, S>D. While the right seminar vesicle had normal size and structure, the left seminal vesicle was enlarged (70/53/65 mm from previous 65/44/63 mm) and contained the multi-loculated cyst. The distal part of the left ureter is deformed and unevenly dilated with a maximal diameter of 33 mm (previous 23 mm). The left ureter impinges on the posterior wall of the bladder and the bladder neck. The multi-loculated cyst in the left seminal vesicle is attached to the rectum causing a rectal deviation to the right (Figures 2 and 3).
CT revealed a normal right-sided kidney with a non-dilated collecting system and the normal excretion of contrast. The hypoplastic left-kidney, previously 10 mm in size, is now 16 mm thick with event echogenicity. The left-ureter is represented as the tubular structure with uneven diameter. The size of the left ureter is increased compared to the previous findings. The contrast is not excreted in the left ureter. The bladder is not fully filled with urine and is deformed.
Conclusion
We reported a case of Zinner syndrome, one of the rarest genitourinary system anomalies. Ultrasound as well as CT and MRI can easily detect the abnormalities specific for Zinner syndrome. Asymptomatic patients require active follow-up while symptomatic patients with enlarging seminal vesicle cyst require surgical intervention such as perineal cyst aspiration, subcutaneous cyst drainage, laparoscopic, and open surgery. Male patients need to be followed up for infertility. Our patient is asymptomatic. Therefore, he requires an active follow-up.
References
- Zinner. (1914) An instance of intravesical seminal vesicle cyst. Wien Med Wochenschr Suppl. 64: 605.
- Khanduri S, Katyal G, Sharma H, Goyal A, Singh N, et al. (2017) Unique Association of Multiple Seminal Vesicle Cysts with Contralateral Renal Agenesis: A Rare Variant of Zinner Syndrome. Cureus. 9: 1415.
- Mehra S, Ranjan R, Garga UC. (2016) Zinner syndrome-a rare developmental anomaly of the mesonephric duct diagnosed on magnetic resonance imaging. Radiol Case Rep. 11: 313-317.
- Farooqui A, AlDhahir L, Mahfooz AB. (2018) Massive seminal vesicle cyst with ipsilateral renal agenesis-Zinner syndrome in a Saudi patient. Urol Ann. 10: 333-335.
- Slaoui A, Regragui S, Lasri A, Karmouni T, El Khader K, et al. (2016) Zinner's syndrome: Report of two cases and review of the literature. Basic Clin Androl. 26: 10.
- Trigaux JP, van Beers B, Delchambre F (1991) Male genital tract malformations associated with ipsilateral renal agenesis: sonographic findings. J Clin Ultrasound. 19: 3-10.
- Kenney PJ, Leeson MD (1983) Congenital anomalies of the seminal vesicles: spectrum of computed tomographic findings. Radiology. 149: 247-251.
- Kord E, Zisman A, Darawsha AE, Dally N, et al. (2017) Minimally invasive approach for treatment of seminal vesicle cyst associated with ipsilateral renal agenesis. Urol Int. 99: 338-342.
- van den Ouden D, Blom JH, Bangma C, de Spiegeleer AH. (1998) Diagnosis and management of seminal vesicle cysts associated with ipsilateral renal agenesis: A pooled analysis of 52 cases. Eur Urol. 33: 433-440.
- Politano VA, Lankford RW, Susaeta R (1975) A transvesical approach to total seminal vesiculectomy: A case report. J Urol. 113: 385-388.
- Okoye BO, Jones DJ, Lancashire MJ, Brown EF, Ritchie AW, et al. (1995) Transvesical endoscopic drainage of a seminal vesicle cyst. Br J Urol. 76: 810.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences