Whole-Body-CT First, FAST second
Pothmann Carina Eva Maria, Simmen Hans-Peter* and Pape Hans-Christoph
Division of Trauma, University Hospital Zurich, Zurich, Switzerland
- *Corresponding Author:
- Simmen Hans-Peter
Division of Trauma
University Hospital Zurich
Zurich, Switzerland
Tel: +41442551111
E-mail: HansPeter.Simmen@usz.ch
Received date: February 15th,2017; Accepted date: February 27th,2017; Published date: March 05th,2017
Citation: Carina Eva Maria P, Hans-Peter S, Hans-Christoph P. Whole-Body-CT First, FAST second. J Emerg Trauma Care 2017. 2:1.
Commentary
The adequate initial diagnostic in the resuscitation room lately became a big topic of discussion.
The American standard of trauma diagnostic includes a focused assessment with sonography for trauma (FAST) within the primary survey as proclaimed by the American College of Surgeons` Committee on Trauma and taught in the advanced trauma live support (ATLS®) [1].
Zanobetti et al. [2] proved their CA-FAST protocol to be a rapid bedside method, with good accuracy in detection of ultrasonographical patterns suggestive of serious injury in trauma patients. Ultrasonography should be used as initial investigation during the primary survey, sending to further diagnostic studies (CT scan) only those patients not clearly classified.
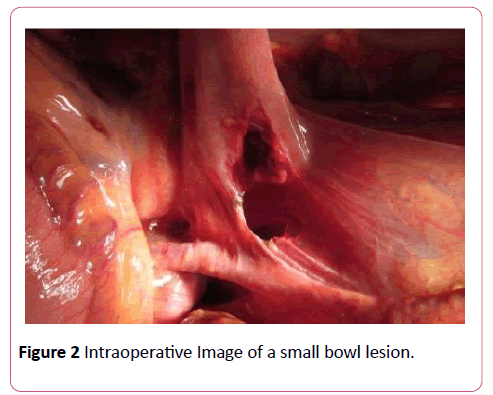
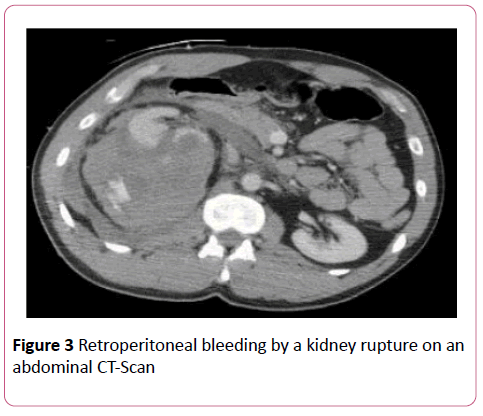
Sonography in trauma patients can be associated with obstacles as within obese patients or patients with intestinal gas. A retroperitoneal bleeding might be difficult to realize as there is no free fluid seen in the abdomen. Also, small hollow viscus organ lesions can easily be missed. A delay of the diagnose of a hollow viscus organ injury, such as a small bowl injury, has a major impact on the morbidity and mortality of trauma patients.
A study of Niederee et al. [3] indicate that the prolonged time to repair of a perforated small bowel injury increased both morbidity and mortality. When operative control of enteric contamination was delayed (>24 hours), there was a significant increase in the rates of intra-abdominal abscess, sepsis, and wound dehiscence compared with perforations repaired early (<8 hours). In the patients who had isolated perforation of the small bowel (no other injury with an Abbreviated Injury Scale score >1), differences were also dramatic. Patients with perforated small bowl injuries who had their repair performed within 8 hours had a significantly lower overall complication rate and lower rates of acute renal failure and sepsis. Time to operative intervention was a major factor in mortality.
In the isolated small bowl injury group, mortality nearly quadrupled by delaying operative repair past 24 hours. Patients who had their repair performed within 24 hours had 4% mortality, whereas patients who had their repair performed after 24 hours had 15% mortality (p 0.029).
Whilst treating polytraumatized patients we examined an advantage in preferring a primary Whole-Body-CT scan to a FAST.
In a survey of members of the American Association for the Surgery of Trauma, CT scan emerged as the most common diagnostic tool in the stable blunt trauma patient [4].
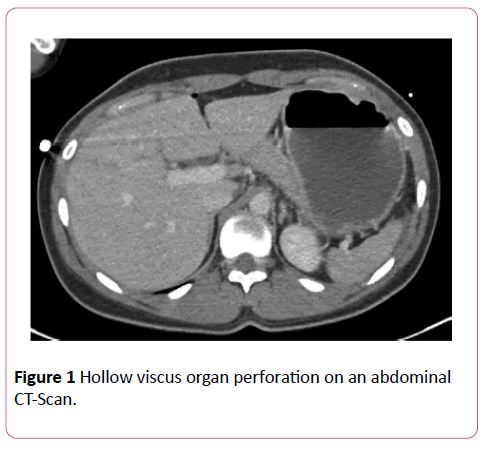
Huber-Wagner et al. [5] have shown that Whole-Body-CT significantly increases the survival rate in hemodynamically stable as well as unstable patients. This statement is underlined by an USZ Online survey of the year 2015 showing the abdominal CT with intravenous contrast agent had top priority in 51% of the 175 participating departments. Even small hollow viscus lesions can be detected with a high sensitivity (Figure 1).
Although some authors have proposed abdominal CT scan as an accurate method for diagnosing small bowl injuries, false negative rates of approximately 6% to 15% have made it difficult to endorse CT scan as a reliable test for excluding small bowl injuries [6].
A Whole-Body-CT scan can be performed within a few minutes after the patients’ admission and detect abdominal injuries, as well as other trauma related injuries with high significance and reduce the mortality and morbidity.
If there is a high grade of suspicion of a blunt hollow viscus organ injury in a polytrauma patient by the mechanism of injury and the clinical examination, we recommend an early abdominal CT or Whole-Body-CT scan for primary diagnostics. Not to forget there is an up to 15% chance of false negative results. If in doubt, take the laparoscope in and be aware, delayed diagnosis can be fatal (Figures 2 and 3).
References
- Committee on Trauma, American College of Surgeons (2008) ATLS: Advanced trauma life support program for doctors (8thedn). Chicago: American College of Surgeons. ISBN 978-1-880696-31-6. OL 22228190M.
- Zanobetti M,CoppaA, Nazerian S, Grifoni M, Scorpiniti F, et al. (2015) Chest abdominal-focused assessment sonography for trauma during the primary survey in the emergency department:The CA-FAST protocol. Eur J Trauma Emerg Surg. 2015.
- Niederee MJ, Byrnes MC, Helmer SD, Smith RS (2003) Delay in diagnosis of hollow viscus injuries: Effect on outcome. Am Surg 69:293-298.
- Brownstein MR, Bunting T, Meyer AA, Fakhry SM (2000) Diagnosis and management of blunt small bowl injury: A survey of the membership of the American assiciation of the surgery of trauma. J Trauma 48:402-427.
- Huber-Wagner S, Biberthaler P, Häberle S, Wierer M,Dobritz M, et al. (2013) Whole-body CT in haemodynamically unstable severely injured patients: A retrospective, multicentre study. PLoS One 8: e68880.
- Fakhry SM, Watts DD, Luchette FA(2003) Group EM-IHVIR. Current diagnostic approaches lack sensitivity in the diagnosis of blunt small bowl injury: Analysis from2275,557 trauma admissions from the EAST Multi-Institutional HVI Trial. J Trauma 54:295-306.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences