Two-Dimensional Ultrasound Fetal Adrenal Gland Enlargement to Predict Spontaneous Preterm Birth in Singleton Pregnancy at GA 240/7-296/7 Weeks
Porntip Tassananutriyakul, Sukanya Chaiyarach* and Piyamas Saksiriwutth
Department of Obstetrics and Gynecology, Khon Kaen University, Muang, Thailand
- *Corresponding Author:
- Sukanya
Chaiyarach
Department of Obstetrics and Gynecology,
Khon Kaen University,
Muang, Thailand,
E-mail: Sukanyatanoorat@hotmail.com
Received Date: October 7, 2021; Accepted Date: October 21, 2021; Published Date: October 28, 2021
Citation: Chaiyarach S, Tassananutriyakul P, Saksiriwutth P (2021) Two-Dimensional Ultrasound Fetal Adrenal Gland Enlargement to Predict Spontaneous Preterm Birth in Singleton Pregnancy at GA 240/7-29 6/7. J Womens Health Reprod Med Vol.5 No.6: 21.
Abstract
Objectives: To predict spontaneous Preterm Birth (PTB) in asymptomatic singleton pregnant women by two-dimensional (2D) ultrasound measurement of Fetal Zone Enlargement (FZE).
Methods: A prospective cohort study was conducted at Srinagarind Hospital, Khon Kaen University. Asymptomatic singleton pregnancies between 240/7 and 296/7 weeks were included. Fetal adrenal gland size was assessed using Trans abdominal 2D ultrasound. Ratios between fetal zone and total adrenal gland in transverse, coronal and sagittal planes as length/Length (l/L), width/Width (w/W) and depth/ Depth (d/D), respectively were used to measure FZE. The ratio of each dimension was used to predict spontaneous preterm birth, with the receiver operating characteristic (ROC) curve used to assess diagnostic accuracy.
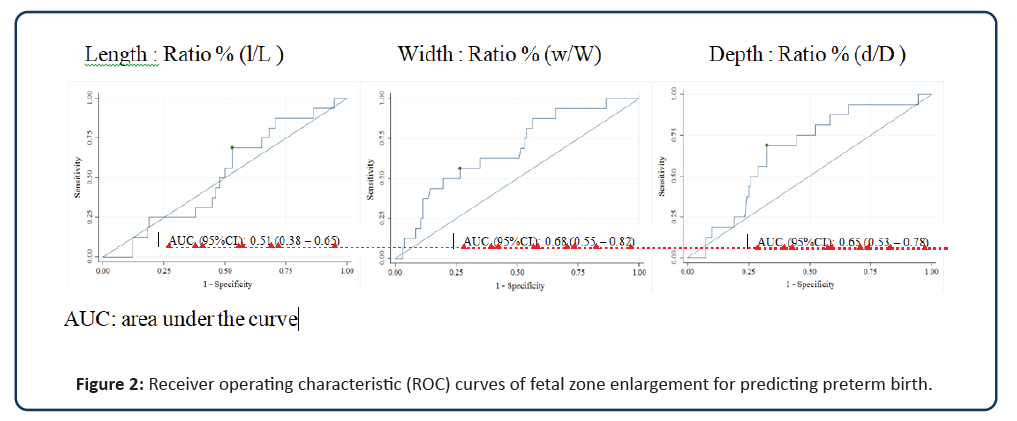
Results: A total of 148 pregnancies were included in the study. Sixteen pregnant women (10.81%) had spontaneous preterm birth. The fetal Zone Enlargement in coronal (w/W) and sagittal planes (d/D) were statistically significantly higher in the preterm group (P<0.05). Cut-off values of w/W and d/D ratio greater than 61.80% and 60.15%, respectively were satisfactory predictors of spontaneous preterm birth (d/D ratio, area under curve (AUC)=0.65, 95% CI 0.53-0.78; w/W ratio, 0.68, 95% CI 0.55-0.81) compared to l/L ratio (AUC=0.51, 95% CI 0.38-0.65).
Conclusion: Fetal adrenal gland enlargement measurement by 2D ultrasound between 240/7 and 296/7 weeks successfully predicted spontaneous preterm birth in asymptomatic singleton pregnant women.
Keywords
Preterm birth; Fetal; Adrenal gland; Fetal zone; Ultrasonography
Introduction
Preterm Birth is a major complication and a leading cause of global neonatal morbidity and mortality. An estimated 15 million babies each year are born preterm worldwide. Among 184 countries, rates of preterm birth ranged from 5 to 18% [1]. Many screening modalities are available for prediction of spontaneous preterm birth including prior spontaneous preterm birth, cervical length measurement or biochemical marker tests as the fetal fibronectin test. However, these methods have poor efficacy in identifying women destined to deliver preterm.
Preterm labor (PTL) has a multifactorial etiology including decreased cervical incompetence and inflammatory or ischemic insult to the uteroplacental barrier [2]. Activation of the fetal hypothalamic-pituitary pathway also plays an important role in initiating the parturition process [3]. Jovana, et al. studied the development of the fetal adrenal gland. They found that the central zone of the adrenal gland (fetal zone) produced dehydroepiandrosterone (DHEA) as the precursor of placental estrogen production that regulates the timing of the labor process, with subsequent enlargement during gestation [4]. Several studies have shown enlargement of the fetal zone of the adrenal gland as a predictor of preterm delivery within 7 days in symptomatic pregnant women [5-7], while one study found that fetal adrenal gland size was not predictive of preterm birth in asymptomatic pregnant women [8]. These findings led us to examine ultrasound measurement of the fetal adrenal gland to predict spontaneous preterm birth.
Materials and Methods
A prospective cohort study was performed in the obstetric outpatient clinic at Srinagarind Hospital, Khon Kaen University (KKU) between August 2020 and July 2021. The KKU Ethics Committee in Human Research approved this study and all registered women provided informed consent. The 152 consecutive women with asymptomatic singleton pregnancies between 240/7 and 296/7 weeks of gestation were enrolled. Pregnant women with medical disorders such as diabetes mellitus or gestational diabetes, maternal heart disease, chronic hypertension, preeclampsia, eclampsia, hydramnios, placental previa or abruption, fetal abnormalities, growth restriction, non-reassuring fetal heart rate tracing and fetal adrenal gland that could not be measured were excluded from the study. The preterm birth was defined as a baby born before 37 weeks of gestation.
Maternal demographic data including age, gestation, body mass index, risk factors of preterm labor such as smoking, alcohol drinking, previous cervical surgery and history of previous preterm delivery were collected. All examinations were performed by one operator, using an ultrasound Samsung HS50 with a 2-5 MHz abdominal transducer.
Assessment of fetal zone enlargement
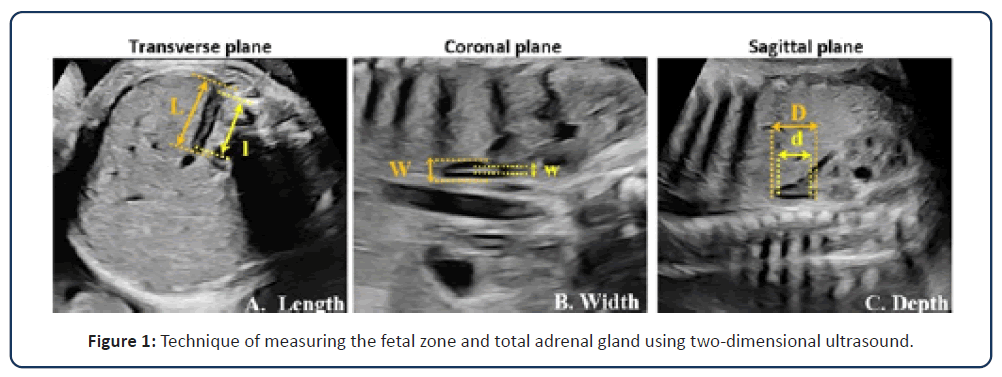
A 2D ultrasound was performed for fetal biometry and structural survey before adrenal gland measurement. Previous reports suggested that the fetal adrenal gland on the right side was less variable than on the left side [8,9]. Therefore, only the right adrenal gland was measured. The central zone of the adrenal gland (fetal zone) is an echogenic area. The total adrenal gland and fetal zone were measured in transverse, coronal and sagittal planes as length, width and depth, respectively (L, l; W, w; and D, d) (Figure 1). The Fetal Zone Enlargement was calculated by dividing the fetal zone and total gland in each dimension (l/L, w/W and d/D), with results used to determine the risk of preterm birth.
Finally, all birth information was recorded as gestational age and neonatal outcome for analysis.
Statistical analysis
Statistical analysis was performed using STATA version 10 for Windows. The continuous variables were compared by Student’s t-test. Data were presented as median [IQR] and mean ± SD as appropriate. The Kolmogorov-Smirnov test was used for data normality testing, with Fisher’s exact and the Chi-square test for categorical variables. P value<0.05 was considered as statistically significant. The ROC was used to find the optimal cut-off value of Fetal Zone Enlargement to predict spontaneous preterm birth. Sensitivity, specificity, likelihood ratio, positive predictive value and negative predictive value were used to quantify diagnostic accuracy.
Results
A total of 152 pregnancies were recruited into this study. Of these, four were excluded due to DFIU from placental abruption, gestational diabetes, pre-eclampsia and fetal growth restriction. Thus, 148 pregnancies were included for statistical analysis. Demographic data, sonographic characteristics and neonatal information of both groups are shown in Table 1. All participants were Thai race. None of the women had undergone cervical surgery, smoked or used illicit drugs. Women at risk of preterm birth were likely to be older, have higher BMI, history of previous preterm delivery and less fetal body weight at the date of recruitment. However, there were no differences between the groups (Table 1). Spontaneous preterm birth was recorded in 16 (10.81%) pregnancies with 132 (89.19%) term birth pregnancies. Median gestation of delivery in the preterm group was 35.93 weeks (IQR 34.72-36.64), while the term group was 38.86 weeks (IQR 38.14-39.43).
| Characteristics | Preterm delivery | Term delivery | P-value |
|---|---|---|---|
| N=16 | N=132 | ||
| Maternal characteristics | |||
| Maternal age (years), mean ± SD | 32.44 ± 5.45 | 29.91 ± 5.10 | 0.07 |
| Parity (%) | |||
| Nulliparity | 8 (50) | 63(47.73) | 0.86 |
| Multiparity | 8 (50) | 69 (52.27) | |
| BMI (kg/m2), median (IQR) | 23.67 (20.90-30.26) | 21.47 (19.68-24.14) | 0.05 |
| Prior preterm delivery (%) | 2 (12.50) | 4 (3.03) | 0.13 |
| Education (%) | |||
| Less than or secondary school | 3(18.75) | 33(25) | 0.76 |
| Complete college or higher | 13 (81.25) | 99(75) | |
| Underlying disease | 0 (0) | 6 (4.55) | >0.99 |
| GA at recruitment (weeks), median (IQR) | 26.86 (25.65-27.93) | 27.57 (25.64-28.71) | 0.32 |
| Fetal body weight (g), mean ± SD | 941.63 ± 209.57 | 1075.49 ± 268.86 | 0.06 |
| Fetal zone-Total adrenal gland | |||
| Length (mm), median (IQR) | |||
| Total gland | 16.51 (3.06) | 17.23 (3.66) | 0.46 |
| Fetal zone | 10.01 (1.97) | 10.45 (3.37) | 0.44 |
| Ratio (l/L) (%) | 61.29 (55.76-68.74) | 60.95 (52.91-69.71) | 0.86 |
| Width (mm), median (IQR) | |||
| Total gland | 12.67 (4.94) | 14.29 (3.78) | 0.12 |
| Fetal zone | 7.8 (7.1-10.77) | 7.6 (5.6-9.9) | 0.47 |
| Ratio (w/W) (%) | 62.10 (10.02) | 54.26 (12.41) | 0.02 |
| Depth (mm), median (IQR) | |||
| Total gland | 11.8 (9.05-14.1) | 12.55 (10.2-15.3) | 0.32 |
| Fetal zone | 7.8 (6.15-9.6) | 6.7 (5-8.75) | 0.25 |
| Ratio (d/D) (%) | 63.87 (55.33-65.47) | 54.69 (45-64.84) | 0.04 |
| Perinatal outcome | |||
| GA at delivery (weeks), median (IQR) | 35.93 (34.72-36.64) | 38.86 (38.14-39.43) | <0.01 |
| Birth weight (g), mean ± SD | 2585.63 ± 510.87 | 3191.82 ± 395.98 | <0.01 |
| Male sex (%), mean ± SD | 10 ± 62.5 | 79 ± 59.85 | 0.84 |
Note: BMI-Body Mass Index; GA-Gestational Age; IQR-Interquartile Range; SD-Standard Deviation;
L, W and D, Length, Width And Depth, respectively of the total adrenal gland; L, W And D-Length, Width and Depth, Respectively of the fetal zone.
Table 1: Maternal characteristics, sonographic data and perinatal outcome among preterm delivery and term delivery groups.
Comparisons of fetal zone and total adrenal gland size in each dimension between groups are shown in Table 1. The FZE in the coronal plane (w/W) and sagittal plane (d/D) of preterm birth were significantly higher than in pregnant women with term birth (P<0.05). Optimal cut-off values for FZE to predict preterm birth were investigated using the ROC curve. Ratios of w/W and d/D greater than 61.80% and 60.15%, respectively had higher area under the curve at more than 0.6 as satisfactory predictors (d/D ratio, AUC=0.65, 95% CI 0.53-0.78; w/W ratio, 0.68, 95%CI 0.55- 0.81) compared to l/L ratio (0.51, 95% CI 0.38-0.65) (Figure 2). Sensitivity, specificity, likelihood ratio, positive predictive and negative predictive values of the adrenal gland dimension ratio at the cut-off values are shown in Table 2.
| Optimal cutoff | Sensitivity | Specificity | +LR (95% CI) | -LR (95% CI) | PPV | NNV |
|---|---|---|---|---|---|---|
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |||
| l/L>59.73% | 68.8 | 47 | 1.3 | 0.67 | 13.6 | 92.5 |
| (41.3-89) | (38.2-55.8) | (0.90-1.87) | (0.32-1.41) | (6.98-23) | (83.4-97.5) | |
| w/W> 61.80% | 56.3 | 73.5 | 2.12 | 0.6 | 20.5 | 93.3 |
| (29.9-80.2) | (65.1-80.8) | (1.26-3.56) | (0.34-1.05) | (9.8-35.3) | (86.6-97.3) | |
| d/D>60.15% | 68.8 | 67.4 | 2.11 | 0.463 | 20.4 | 94.7 |
| (41.3-89) | (58.7-75.3) | (1.4-3.18) | (0.22-0.97) | (10.6-33.5) | (88-98.3) |
Note: CI-Confidence Interval; l/L-length of fetal zone/length of total gland; w/W-width of fetal zone/width of total gland; d/D-depth of fetal zone/depth of total gland; +LR-positive likelihood ratio; -LR-negative likelihood ratio; PPV-positive predictive value; NNV-negative predictive value.
Table 2: Value of fetal zone enlargement in three planes for predicting preterm birth.
Discussion
Currently, the standard recommendation for screening preterm birth uses cervical length and a biochemical marker as fetal fibronectin. However, routine cervical length screening in asymptomatic pregnancies provides insufficient evidence [10], while the presence of fetal fibronectin as an indicator of Preterm Premature Rupture of the Membrane (PPROM) to predict preterm birth shows high false-positive values [11]. This study evaluated the usability of fetal adrenal gland enlargement to predict preterm birth in asymptomatic pregnancies, based on the hypothesis that the fetal zone of the adrenal gland produces DHEA as a precursor in the hypothalamic-pituitary-adrenal axis that regulates the timing of human parturition, resulting in fetal adrenal gland enlargement [4]. As supporting evidence, fetal adrenal gland enlargement was statistically significantly associated with preterm birth. The best predictor was w/W ratio greater than 61.8% (AUC=0.68, 95%CI 0.55-0.81) and the second predictor was d/D ratio greater than 60.15% (AUC=0.65, 95% CI 0.53-0.78). These applications had low sensitivity and specificity but were useful to rule out the risk of preterm birth due to high negative predictive value (Table 2). The FZE was an independent predictor that mostly benefited general pregnancies, while also reducing costs of some patients through avoidance of unnecessary treatment. The 2D ultrasound used to measure the size of the fetal adrenal gland in hospitals may be challenging because this method depends on fetal position, amount of amniotic fluid, maternal habitus and the operator.
A previous study noted that fetal zone and total adrenal gland depth ratio was higher in preterm delivery [12], while several studies combined fetal adrenal gland ratio enlargement with other predictors. Santipap M, et al. found that the combination of fetal zone dimension enlargement and high levels of Placental Alpha Macroglobulin-1 (PAMG-1) was effective for predicting preterm birth within 7 days in symptomatic pregnancies [13]. Other studies revealed that FZE and Adrenal Gland Volume (AGV) using 2D and 3D ultrasound, respectively could predict preterm birth within 7 days in symptomatic pregnancies. When compared with cervical length, FZE and AGV were superior predictors in identifying women at risk from preterm birth within 7 days [5,6].
By contrast, a large multicentre observational cohort study of asymptomatic nulliparous women found that fetal adrenal size measured at 220/7 and 306/7 weeks did not predict spontaneous preterm birth [14]. This was not surprising because a variety of pathways lead to preterm labor including intrauterine infection, uterine ischemia, uterine over-distension, abnormal allogenic recognition, allergic-like reaction, cervical disease and endocrine disorders [2]. Changes in the adrenal gland occur before preterm labor within 5-7 days, and may not be accurately used to identify preterm birth in asymptomatic pregnancies [14].
Currently, no effective screening method exists to identify preterm birth in low-risk pregnancies. Our results can be used to identify the risk of preterm birth in asymptomatic pregnancies using 2D ultrasound fetal zone-total adrenal gland ratio. The strength of our study results was demonstrated in healthy asymptomatic pregnant women excluding maternal disease, placental previa, fetal anomalies, fetal infection and indicated preterm delivery that had different etiology of preterm labor. All the pregnant women were followed up until delivery. Limitations of our study were the small cohort size, with all participants as Thai race. One operator determined all adrenal gland measurements. Further larger studies are required to support our results. Future studies of adrenal gland size should include gestational age as a baseline reference.
Conclusion
Fetal adrenal gland enlargement measured by two-dimensional ultrasound between 240/7 and 296/7 weeks successfully predicted spontaneous preterm birth in asymptomatic singleton pregnant women.
References
- WHO. 2018. Preterm birth.
- Romero R, Espinoza J, Kusanovic JP, Gotsch F, Hassan S, et al. (2006 )The preterm parturition syndrome. BJOG: An International Journal of Obstetrics & Gynaecology.113:17-42.
- Behrman RE, Butler AS. Preterm birth: Causes, consequences, and prevention.
- Kaludjerovic J, Ward WE (2012). The interplay between estrogen and fetal adrenal cortex. J Nutr Metab.
- Turan OM, Turan S, Funai EF, Buhimschi IA, Campbell CH, et al. (2011) Ultrasound measurement of fetal adrenal gland enlargement: An accurate predictor of preterm birth. AJOG.204(4):311.
- Ibrahim MI, Sherif A, El-Kady M, Ellaithy M, Husseiny A, et al. (2015) Can three-dimensional ultrasound measurement of fetal adrenal gland enlargement predict preterm birth? Arch Gynecol Obstet 292(3):569-578.
- Lemos AP, Feitosa FE, Araujo Junior E, Feitosa HN, Pereira JG, et al. (2016) Delivery prediction in pregnant women with spontaneous preterm birth using fetal adrenal gland biometry. J. Matern.Fetal Neonatal Med. 29(23):3756-3761.
- Scott EM, Thomas A, McGarrigle HH, Lachelin GC (1990) Serial adrenal ultrasonography in normal neonates. J Ultrasound Med. 9(5):279-283.
- Iijima S (2018) Sonographic evaluation of adrenal size in neonates (23 to 41 weeks of gestation). BMC pediatrics. 18(1):1-7.
- Berghella V, Saccone G (2019) Cervical assessment by ultrasound for preventing preterm delivery. Cochrane database of systematic reviews.
- Varley-Campbell J, Mújica-Mota R, Coelho H, Ocean N, Barnish M, et al. (2019) Three biomarker tests to help diagnose preterm labour: a systematic review and economic evaluation. Health Technol Assess. 23(13):1-226.
- Guler AE, Pehlivan H, Cakmak B, Baser I. Assessment of fetal adrenal gland enlargement in term and preterm labor cases.
- Santipap M, Phupong V (2018) Combination of three-dimensional ultrasound measurement of foetal adrenal gland enlargement and placental alpha microglobulin-1 for the prediction of the timing of delivery within seven days in women with threatened preterm labour and preterm labour. J Obstet Gynaecol. 38(8):1054-1059.
- Hoffman MK, Turan OM, Parker CB, Wapner RJ, Wing DA, et al. (2016) Ultrasound measurement of the fetal adrenal gland as a predictor of spontaneous preterm birth. Obs Gyn. 127(4):726.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences