ISSN : 2576-392X
Dentistry and Craniofacial Research
Thrombocytopenia Associated With Oral Infection: A Case Report
Kholoud Alamri* and Ibtisam Al Bakr
Department of Oral Medicine and Special Care Dentistry, Dental Center, PSMMC Riyadh, Saudi Arabia
- *Corresponding Author:
- Kholoud Alamri, Department of Oral Medicine and Special Care Dentistry, Dental Center, Riyadh, Saudi Arabia, Tel: 966550512178; E-mail: kholod.a.alamri@gmail.com
Received: 14-Mar-2022, Manuscript No. IPJDCR-22-12219; Editor assigned: 17-Mar-2022, Pre QC No. IPJDCR-22-12219(PQ); Reviewed: 31-Mar-2022, QC No. Q-12219; Revised: 5-Apr-2022, Manuscript No. IPJDCR-22-12219(Q); Published: 12-Apr-2022, DOI: 10.36648/2576-392X/22.7.9
Citation: Alamri K, Al Bakr I (2022) Thrombocytopenia Associated With Oral Infection: A Case Report. Dent Craniofac Res Vol:7 No:2
Abstract
Thrombocytopenia is a hematologic disorder that is characterized by a markedly decreased number of circulating blood platelets (below 150 × 109/L). It can be further classified into mild (100-150 × 109/L), moderate (50-100 × 109/L), and severe (<50 × 109/L).
Platelets count less than 10 × 109/L is usually associated with an increased risk of spontaneous bleeding, petechiae, and bruising. Life-threatening hemorrhage may occur in patients with platelets count less than 5 × 109/L.
Keywords
Life-threatening; Thrombocytopenia; Petechia; Hemorrhagic blisters
Introduction
Thrombocytopenia can be caused by decreased platelet production by megakaryocytes in the bone marrow, increased destruction of circulating platelets, and abnormal secretion of platelets in the spleen [1-3].
Infections, whether viral or bacterial, can lead to thrombocytopenia [1,4]. A link between sepsis and thrombocytopenia has been proposed [5,6]. Thrombocytopenia may serve as an indicator of the severity of infection. In most acute infections, thrombocytopenia is transient and resolves after treating the underlying cause [6-9]. Facial infections can cause coagulation abnormalities ranging from thrombocytopenia to a fulminant state of disseminated intravascular coagulation [10,11].
In the mouth, soft tissue thrombocytopenic lesions usually appear in regions subjected to trauma, including the buccal mucosa, lip, and the junction between soft and hard palate [12]. Petechia, hemorrhagic blisters, and spontaneous gingival bleeding are examples of these lesions [13]. The dentist may notice the first clinical signs of thrombocytopenia. His role as a healthcare professional is to screen for undiagnosed hematological disorders by ordering appropriate blood tests and to provide the patient with an immediate referral to hematologists.
Here we report a case of transient thrombocytopenia associated with an orofacial infection that showed only unilateral oral manifestation and resolved completely after treatment of the underlying cause.
Case report
A 58-year-old male patient was referred to the department of oral medicine and special care dentistry at (PSMMC/Riyadh, Saudi Arabia), with a complaint of two days painless swelling over the right side of his face, as well as an intraoral lesion. At presentation, the patient was clinically stable. He did not report dysphagia or dyspnoea. However, a slight increase in body temperature that was controlled by antipyretics was reported. His past medical history was significant for type 2 diabetes mellitus. His daily medication consisted of metformin 500 mg 3 times daily. The patient denied any recent changes in medication, recent hospitalization, immunization, or travel. The patient also denied acute or chronic alcohol intake. His family history did not reveal any significant findings.
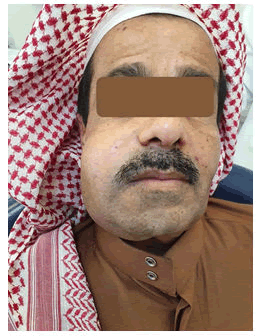
On physical examination, the patient was well-nourished, had no pain, no airway obstruction, and no limitation of mouth opening. There was a huge, non-tender swelling on the right side of the face, extending from the cheek to the submandibular area. The overlying skin had normal color (Figure 1).
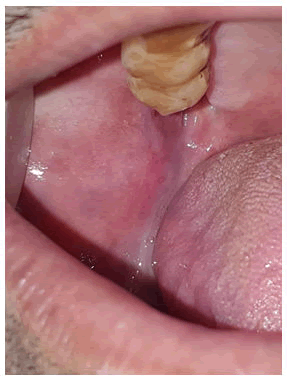
Intraoral examination revealed ecchymosis in the right buccal mucosa extending to the right soft palate, a large brown lobulated lesion in the right posterior buccal mucosa, and two haemorrhagic bullae in the right soft palate. Other oral sites were unremarkable (Figures 2 and 3). All upper and lower teeth had crowns/mobile implants, with very poor oral hygiene.
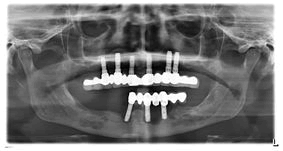
Orthopantomography (OPG) showed bone defects and infection around multiple implants (Figure 4).
Figure 4: OPG shows bone defect and infection around multiple implants.
On the basis of clinical examination; orofacial infection together with blood dyscrasia were mainly considered. Other differential diagnosis of the intraoral lesions included hematoma, vascular lesion/neoplasm.
The patient was given an antibiotic (Augmentin 1000 mg twice/day), and instructed to go to the emergency department in case of increased swelling, dysphagia, or difficulty in breathing.
Routine haematological investigations and cell count studies were performed. It revealed the following: extremely low platelets count (critical value 7 × 109/L), normal white blood cells count with increased monocyte absolute (1.3 × 109/L), normal red blood cells count, low haemoglobin (96 g/L), and preserved coagulation studies (Prothrombin Time (PT), International Normalized Ratio (INR), and Partial Thromboplastin Time (PTT). Blood chemistry showed normal values for electrolytes, urea, and creatinine, as well as liver enzymes.
Haematology consultation was sought, the platelet count was repeated to exclude the possibility of pseudo-thrombocytopenia, peripheral blood smear was reviewed which was unremarkable with no hemolysis.
Further investigations were performed to rule out other possible causes of thrombocytopenia. Viral serology for (HIV/HBV/HCV) was negative, autoimmune serology (ANA, ENA, RF) was negative, lactate dehydrogenase was elevated (269 U/L), vitamin B12, folate, and thyroid function tests were within normal limits.
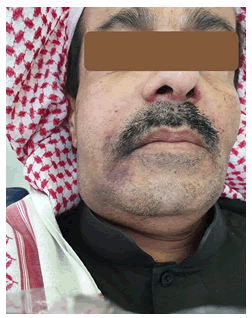
On the third day of clinical presentation, the patient showed a decrease in the extraoral swelling with the appearance of ecchymosis in the outer right facial skin (Figure 5). Intraoral examination revealed a decrease in the size of the buccal lesion (hematoma), with the appearance of focal ulcerative areas and surface necrosis.
There was ecchymosis extending to the soft palate [Figure 6]. When CBC was repeated, the platelet count rose to (56 × 109/L). On the fourth day, the platelets increased to (91 × 109/L) with leucocytosis and decrease in RBC (3.93).
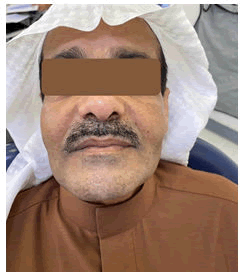
The patient continued to improve. Three weeks later, all extraoral swelling and intraoral lesions had resolved completely (Figures 7 and 8). Platelets, WBC, RBC, and lactate dehydrogenase returned to normal limits.
The patient improved clinically with antibiotics and the signs of active infection resolved. Thrombocytopenia was transient and was associated with infection and inflammation around the implants. The lower implants were removed and the patient was referred to a periodontist for assessment of the upper implants.
Discussion
Thrombocytopenia is a hematologic disorder that is characterized by a decreased number of circulating blood platelets. The normal platelets count ranges from (150-450 × 109/L). Thrombocytopenia can be further classified into mild (100-150 × 109/L), moderate (50-100 × 109/L), and severe (<50 × 109/L) [1-3]. However, there is no direct correlation between platelet count and clinical signs and symptoms, so such a classification has little clinical value [14].
The risk of spontaneous bleeding, petechiae, and bruising is usually associated with platelet counts less than 10 × 109/L [1,4]. Life-threatening hemorrhage may occur in patients with platelets count less than 5 × 109/L. However, spontaneous bleeding due to thrombocytopenia can occur at higher counts when fever, sepsis, and severe anemia are present or when platelet function is compromised by drugs [5,6].
Thrombocytopenia can be caused by one of three mechanisms: (1) increased destruction of platelets, as seen in immune-mediated causes; (2) decreased production of platelets, usually due to an underlying bone marrow disorder; or (3) sequestration of platelets within the spleen, as seen in splenomegaly-causing conditions [6,7].
A low platelet count can result from a wide range of conditions, including viral infections (e.g.: HIV infection, hepatitis B and C infection, Epestein-Barr virus, cytomegalovirus, varicella-zoster, rubella, and mumps), bacterial infections (e.g.: Helicobacter pylori), leukemia, aplastic anemia, gestational thrombocytopenia, congenital cytopenia, autoimmune diseases, some medications, alcohol intake, and nutritional deficiency anemia [15-17].
Occasionally, a low platelet count can be the only early sign of an underlying problem that is more dangerous than thrombocytopenia itself (e.g.: HIV infection or myelodysplastic syndromes), or it may be a useful indicator of disease activity (e.g.: thrombotic microangiopathies). It is critical to correctly identify the causes of thrombocytopenia in order to treat these patients appropriately [4].
Secondary immune-mediated thrombocytopenia is frequently caused by infections [5,18]. The infectious agent can induce the production of antibodies that cross-react with the platelet surface antigens causing their destruction and elimination [19].
Thrombocytopenia induced by the infection usually resolves after resolution of the infection [8].
Transient bacteremia resulting from poor oral hygiene or oral infection can cause sepsis, which is one of the predominant risk factors for the development of thrombocytopenia [20-22].
Although there are many reports of thrombocytopenia due to sepsis in the literature, the occurrence of thrombocytopenia with maxillofacial infection is rare. To our knowledge, only one case report published by Kumar and Rajan described life-threatening thrombocytopenia in a patient with an odontogenic infection that resulted in buccal, submandibular, and canine space infections. The case presented unique diagnostic and management challenges to the surgeon [11].
Oral manifestations of thrombocytopenia can be the first clinical signs recognized by the dentist and serve as a guide to the patient's detailed medical history. Spontaneous gingival bleeding or bleeding induced by brushing or flossing is often the first sign of thrombocytopenia. Other oral manifestations include small single or multiple petechial hemorrhages, ecchymosis, or hemorrhagic blisters. The epithelium overlying hemorrhagic blisters may slough and the resulting erosion may become secondarily infected [13].
In the mouth, the thrombocytopenic lesions are usually on the soft tissues most vulnerable to trauma, such as the buccal mucosa, lateral borders of the tongue, the junction between the hard and soft palate, and the gingiva [12,23].
Diagnosis of thrombocytopenia is often challenging, particularly in hospitalized patients, due to the presence of several potential causes, including drugs and infections [4]. Identifying the cause of the patient’s thrombocytopenia is essential to select the most appropriate treatment and avoid unnecessary intervention [6].
However, the cause is not always immediately apparent, and further investigations are usually warranted [1]. Particular attention should be paid to the duration of symptoms. This helps determine if the patient has acute or chronic thrombocytopenia [6].
Preliminary laboratory tests include a Complete Blood Count (CBC) with a differential, along with an examination of the peripheral blood smear to evaluate both for the presence of platelet clumps, indicating pseudo-thrombocytopenia, and for other abnormal cell morphologies [6,15]. Other first-line laboratory tests when investigating thrombocytopenia include renal and liver function tests, coagulation tests and fibrinogen, bilirubin, reticulocyte count, Vitamin B12 and folate studies, autoimmune serology: ANA, ENA, ANCA, rheumatoid factor, viral studies: HIV/HBV/HCV serology, lactate dehydrogenase, and thyroid function tests [4].
Treatment of thrombocytopenia is based on the etiology. In most cases of thrombocytopenia caused by bacteria or viruses, the treatment approach is to treat the underlying infection and continue monitoring. Treatment of the secondary cause results in the normalization of platelet counts [15,24].
Conclusion
Thrombocytopenia can be one of the serious complications of orofacial infection. Spontaneous bleeding, or bleeding induced by trauma, or hemorrhagic bullae may be the first oral manifestations of low platelets count detected by a dentist. Thrombocytopenia increases the risk of bleeding, alters the dental treatment plan, and may serve as an indicator of the severity of infection.
References
- Tang K (2019) A practical approach to thrombocytopenia. Medical Republic.
- Khammissa R, J Fouriea, A Masilanaa, S Lawrenceb, J Lemmera, et al. (2018) Oral manifestations of thrombocytopenia. Saudi Dent J 30:19-25
- Arnold DM (2015) Bleeding complications in immune thrombocytopenia. Hematol Am Soc Hematol Educ Progr 237-242
- Stasi R (2012) How to approach thrombocytopenia. Hematol Am Soc Hematol Educ Progr 1:191-197
- Julie A and Panepinto MD (2011) Berman's Pediatric Decision Making. (Fifth Edition) Elsevier, United States.
- Cecil RL, Goldman L, Schafer AI (2012) Goldman's Cecil Medicine, Expert Consult Premium -Enhanced Online Features and Print, Single: Goldman's Cecil Medicine. Elsevier Health Sciences. (24 Edition). Elsevier Health Sciences, New York.
- Scully’s (2014) Medical Problems in Dentistry; chapter 8: haematology. (Seventh Edition). Churchill Livingstone/Elsevier, Scotland
- Konkle, BA (2010) Harrison’s Hematology and Oncology (Third Edition); chapter 20: Disorders of platelets and vessel wall. McGraw-Hill Education, New York.
- Rajendran R, Nooh N (2012) Shafer’s Textbook of Oral Pathology; Diseases of the blood and blood forming organs. (Seventh Edition). Elsevier, India.
- Vadasz Z, Toubi E (2015) Infection and Autoimmunity Chapter 52-Acute and Chronic Infections: Their Role in Immune Thrombocytopenia. (Second Edition) . Science direct, Israel.
- Kumar Verma D, Rajan R (2011) A case of thrombocytopenia due to odontogenic infection. J Dent Res Dent Clin Dent Prospects 5:144-147
- Regezi JA, Sciubba JJ (1993) Oral Pathology Clinic Pathologic Correlations. (Second Edition). Saunders, United States.
- Mccarthy PL, Shklar G (1964) Oral manifestations of blood dyscrasias, Diseases of the oral mucosa. McGraw-Hill, USA 263-264
- Vinholt PJ (2014) An overview of platelet indices and methods for evaluating platelet function in thrombocytopenic patients. Eur J Haematol 92:367-376
- Robert L, Gauer, Michael M Braun (2012) Am Fam Physician 85:612-622
- Nakhoul IN, Kozuch P, Varma M (2006) Management of adult idiopathic thrombocytopenic purpura. Clin Adv Hematol Oncol 4:136-44[Crossref]
- Stasi R, Provan D (2004) Management of immune thrombocytopenic purpura in adults. Mayo Clin Proc 79:504-522
- Ekstrand C (2016) Increased susceptibility to infections before the diagnosis of immune thrombocytopenia. J Thromb Haemost 14:807-814
- Bettaieb A (1992) Presence of cross-reactive antibody between human immunodeficiency virus (HIV) and platelet glycoproteins in HIV-related immune thrombocytopenic purpura. Blood 80:162-169
- Xiaojing LI (2000) Systemic Diseases Caused by Oral Infection. Clin Microbiol Rev 13:547-558
- Johansson D (2018) Thrombocytopenia in bacteremia and association with bacterial species. Epidemiol Infect 146:1312-1317
- Moreau D (2007) Platelet count decline: an early prognostic marker in critically ill patients with prolonged ICU stays. Chest 131:1735-1741
- Satoskar S (2016) Oral manifestations of immune thrombocytopenic purpura: A diagnosis of exclusion. IOSR-JDMS 15:65-67
- Kudaravalli P (2020) Acute on Chronic Immune Thrombocytopenia as a Cause of Thrombocytopenia in Sepsis. Cureus 12:8168
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences