ISSN : 2348-1927
Annals of Biological Sciences
The Role of Physical Activity on Cognitive Functions in Aged Patients with Alzheimer's disease: A Systematic Review
Gaied Chortane Oussama1, Boumiza S 1, Khalifa R1, Gaied Chortane S2
1Department of Sport Performance Optimization (CNMSS), Ksar-Said, Manouba University, Manouba, Tunisia
2Department of Biological Sciences, Higher Institute of Sport and Physical Education of Tunisia, Manouba, Tunisia
- *Corresponding Author:
- Gaied Chortane Oussama
Department of Sport Performance Optimization (CNMSS),
Ksar-Said, Manouba University, Manouba,
Tunisia.
E-mail: oussama.gaeid@gmail.com
Received date: July 13, 2022, Manuscript No. ABS-21-11881; Editor assigned date: July 15, 2022, PreQC No. ABS-21-11881 (PQ); Reviewed date: July 26, 2022, QC No. ABS-21-11881; Revised date: August 05, 2022, Manuscript No. ABS-21-11881 (R); Published date: August 29, 2022. DOI: 10.36648/2348-1927.10.8.42
Citation: Gaied CO, Boumiza S, Khalifa R, Gaied CS (2022) The Role of Physical Activity on Cognitive Functions in Aged Patients with Alzheimer’s Disease: A Systematic Review. Ann Biol Sci Vol.10 No.8:42
Abstract
Background: Alzheimer Disease (AD) is neurodegenerative pathology, and he is a primary cause of cognitive disorders and motor dysfunction in aged patients worldwide. Despite the enormous research funding in this context, there are no effective treatment for stopping definitely the progression of this disease. Recent studies provide the neuroprotective impacts of physical activity (PA) in AD patients with cognitive impairments. The aim of this study was to systematically review the effects of physical activity (PA) on cognitive functions in patients with AD. Most of funding results provide evidence and suggest that physical activity have a positive affects in cognitive functions in AD. The prevention of Alzheimer disease may be based on various types of interventions such as nutrition, musical-therapy and patients life style to slow down the progression of the disease.
Keywords
Alzheimer disease; Aged patients; Cognitive functions; Physical exercise
Introduction
During the last years, the prevalence of brain disease such as Alzheimer increase progressively and markedly with age as the most important symptom in the disease [1]. Many factors contribute to the development of Alzheimer’s disease (AD) such as biological and environmental factors [2]. Without prevention or treatment, the disease slowly affects and destroys brain regions with the progression of the dementia, in that, the patients lose the ability to carry out the daily life’s tasks. At the present time, AD still the most frequent neurodegenerative disease affected both cognitive and motor capacity [3]. Unfortunately, with all the scientific research findings on this disease, there is no drug available to stop or even to reverse the progression of AD [4]. Several studies have suggested beneficial and positive effects of physical activity (PA) as one of the best non-pahmalogical treatment therapy for AD patients [5]. During Alzheimer’s it has been reported that physical exercise (PE) constitute an effective therapeutic strategy to control and limit the progression of the disease [6]. Physical exercise may also prevent various complications caused by the disease such as falls, decreasing of muscular strength especially in the lower member, mobility disability and weigh loss (Physical activity and cardiovascular health, 1996).
Alzheimer’s disease
Preventive impact of physical activity against Alzheimer dementia
Most of the longitudinal epidemiological studies that have investigated the relation between PA and the risk of cognitive disorders support the idea that regular physical activity delays the progression of AD and dementia in older patients [7]. Regular physical exercise is a therapeutic treatment used to improve cognitive and motor capacity in patients with AD. In recent American study, 17,40 patients over the age of 65 years old with an incidence of neurodegenerative impairments 13.0 per 1,000 training patients with three times of physical exercise per week (balance , walk , cycling , swimming , strength training, stretching) compared with 19,7 per 1,000 patients with a fewer session per week [8].Exercise have positive effects on patients cognition , including memory attention , planning , working memory and dual-task performance in life daily routine [9].Current studies suggest the beneficial impact of physical rehabilitation in activity of daily living in patients with cognitive impairments [10].
Neurophysiology and physical activity in patients with AD
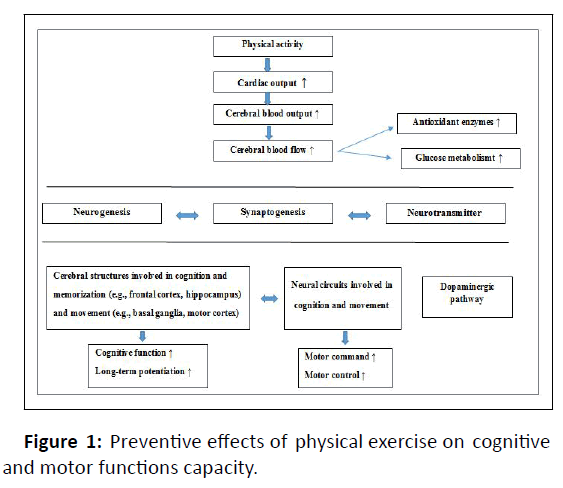
The inverse relationship between physical activity and the risk of neurocognitive impairments is widely documented [11]. Exercise could be a strategy to prevent and slowing the gravity of cognitive and motor disorders in patients with AD [12]. There is a great amount of research studies have undertaken to understand the neurophysiology of the brain, which is changed by the type of exercise [13]. As the disease progress, brain regions will be affected in three principals’ areas: vascular physiology, neurogenesis and hippocampal volumes, in that, oxygen and blood flow to the brain will be affected negatively [14]. It has been shown and confirmed that physical activity increase the blood flow to the brain regions in trained patients with moderate intensity exercise in comparison with others patients who were seated.
Physical exercise has also been shown to act favorably to improve cognitive functions and patient ability in relation with the progression of the hippocampal volume [15] (Figure 1).
Effects of physical activity on global cognition
Executive function
The beneficial impact of physical activity on executive function was evaluated in 10 studies,, 6 of them found a positive effect of exercise training used the verbal fluency test. For the measures of fluency tests authors has suggest the clock drawing test, symbol-digit substitution test. An intervention of 6 weeks based on walking exercises three session a week for 30 min, showed significant results in executive function measured with the verbal fluency trail making test A, B [16-19].
The effect of high intensity aerobic exercise (treadmill) used to verify the effects of physical activity on executive function. During 6 months of training intervention and 4 sessions, a week for 40-60 min a beneficial effect of physical activity was found in all measures in verbal fluency, trail making test b and task switching [18].
Memory
Scientific research studies confirm the association between physical activity and memory in patients with cognitive disorders [20]. Aerobic and balance exercise improve delayed recall and can be a powerful solution for controlling cognitive disorders [21]. In a study conducted by Smith, physical activity program improve cognitive functions such as memory, attention and executive functions in patients with AD , and the gravity of the disease can be lowered by 28% and 45% with a regular physical activity program [22].
Communication
Two only studies were examined the effects of physical activity on communication ability on patients with Alzheimer’s dementia. In a small intervention study with 30 patients, compared the effects of walking and conversation with conversation- only on communication skills in patients with dementia, communication skills has been performed in patients with dual-tasks compared to the conversation-only group [23]. Another larger intervention with 86 patients with AD did not find a beneficial impact between the dual-task performance in walk and talk and communication skills. Patients have both cognitive and motor functions disorders and they were in an intervention with 86 patients with AD did not find a beneficial impact between the dual-task performance in walk and talk and communication skills [24]. Patients have both cognitive and motor functions disorders and they were in an advanced stage of Alzheimer’s disease.
Attention`
Attention is one of the first brain regions to be affected in Alzheimer’s disease [25]. Some initial symptoms that are apparently due to episodic memory loss may be secondary to failures of attention processes. Attention was measured as a specific cognitive domain using a variety of neuropsychological tests such as the color-word Stroop test, the Digit Span Test, the visual search task for the selective attention [26-28].
What is the best physical exercise program speci ic for AD patients?
The beneficial impact of physical activity on cognitive function and cerebral plasticity has been documented over the recent years [29]. There are many physical exercises and programs simple and appropriate for patients with AD. Older patients are considered physically active when they perform physical activity program with moderate intensity training for a minimum of 30 min, 5 days per week, or a minimum of 20 min, 3 days per week of vigorous intensity exercises. Currently there is no best consensus regarding the best PE method used, but it is important to engage the patients in various types of activity. Physical activity program based on aerobic training has been the most method used as a treatment to slowing the negative progression of cognitive disorders in patients with Alzheimer disease [30].
The benefits of physical activity is related with the amount of activity training per day (energy expenditure), rather than the technique and the type of activity There is little doubt that regular physical activity and an active life style improves health condition. Regarding the specific exercises for Alzheimer’s patients, based on available evidence, it is difficult to suggest the best protocol to delay the progression of the disease. Most of studies suggest a various types of exercises and the possibility of maintaining the intervention longer to have better benefits [31].
Exercise prescription
Exercises based on low-intensity training such as walking, swimming, and cycling protects brain regions and cerebral plasticity. Regular physical activity has to be easily accepted and adopted it for the patients with AD to be pertinent. Maintaining a regular exercise program is important to preserve all the benefits, it takes some time, but leads to a long-term success.
Studies have shown that moderate physical activity can reduce the progression of neurodegenerative disease such as Alzheimer [32]. One year of moderate physical activity based on various aerobic exercises (3 days / week, 40 min / session) increase both hippocampal volume and the plasma concentration in older patients with dementia [33]. Regular physical exercise with 40 min – 4 times a week in a total period of 12 weeks, affect positively the brain regions [34]. Aerobic exercise with moderate to high-intensity training has a beneficial impact on neuropsychiatric symptoms (3 sessions /week for 3 months) [35]. Older patients are encouraged to engage in a physical activity program as much possible, patients who practiced 3 times of regular physical activity per weekend had a lower risk of cognitive function compared to other patients with less training sessions [8].
Home based physical activity program with a various types of exercises such as strength and balance resulted in improvements in executive function but there were no changes in other neurocognitive functions [36]. Aged patients with memory impairments showed after 24 weeks of physical exercise program with moderate intensity, a significant improvement in cognitive functions, the beneficial impacts lasted one year and a half after the physical exercise has stopped [37]. Physical rehabilitation is a key to prevent and to delay the progression of cognitive impairments and to improve behaviors and psychologic symptoms in patients with AD, few published studies have been concentrated on resistance training method, this type of physical activity improve cognitive function such as memory and attention (Table 1)[38-41].
| Author and studie name | Year of publication | Population-based Study | Follow-up Period | Assessment of Physical Activity | Major Findings |
|---|---|---|---|---|---|
| Albert et al., | 1995 | 1192 individuals aged 70 to 79 years | 2.5 years | Questionnaire including frequency and level | Strenuous physical activity but not moderate physical activity was associated with a reduced risk of cognitive decline |
| Fabrigoule et al., | 1995 | 1192 individuals aged 70 to 79 years | 3 years | 10 social and leisure activities Physical activity: yes/no | Physically active individuals had a lower risk of dementia |
| Broe et al., | 1998 | 1192 patients aged between70 to 79 years | 3 years | Self-reported questionnaire (no details) | Physically active individuals had a lower risk of AD disease |
| Lam et al., | 2011 | A total of 389 patients in the most are women, with mean age 72 years | 12 weeks | Tai Chi group, n=171: Tai Chi exercice, ≥ 3 × 30 min/week | MMSE, ADAS-Cog, delayed recall, trial, verbal fluency, subjective cognitive functions and attention were improved in exercise group |
| Scherder et al., | 2005 | 43 individuals with a mean age 86 years | 6 weeks | Walking group, n=15: walking exercise 3 × 30 min/week Hand and face exercises, n=13 Control group, n=15, normal social activities | Positive improvement in named trial test in both walking group and hand face group |
Table 1: Observational studies of physical activity and risk of Alzheimer’s disease.
Conclusion
To present the core information of this review, we investigate the therapeutic effects of physical activity for treating and to prevent Alzheimer disease in older patients. At present, there is not enough information’s to confirm the existence of the best exercise, in that, additional interventional studies are needed to examine the association between physical activity and Alzheimer pathology , however the type, duration, frequency and intensity need to be more developed. Physical rehabilitation program based on aerobic exercises decrease the gravity of the disease, but probably this kind of exercises alone is not the perfect method for treating Alzheimer disease, coordination, balance, gait and social activity contribute to improving functional and cognitive capacity . Future research should focus on developing more strategy for reducing the risk of neurodegenerative disease, a combined program based on various types of exercises (strength, stretching, static and dynamic balance), developing the coordination improve psychomotor function and the nervous control system in AD patients. The question is how to change the life style and to promote physical activity for the patients the longer period possible, preventive factors could be a decisive solution for modifying patients, caregivers and public health policy.
References
- Bonaconsa M, Colavito V, Pifferi F, Aujard F, Schenker E et al (2013) Cell clocks and neuronal networks: Neuron ticking and synchronization in aging and aging-related neurodegenerative disease. Curr Alzheimer Res 10: 597-608.
[Crossref] [Google Scholar] [Indexed]
- Paulson HL, Igo I (2011) Genetics of dementia. Semin Neurol 31: 449-460.
[Crossref] [Google Scholar] [Indexed]
- Ibanez V (2005) Les maladies neurodegeneratives: Problemes cliniques. Med Nucl 29: 213-219.
- Baldacci F , Lista S, Garaci F, Bonuccelli U, Toschi N et al (2016) Biomarker-guided classification scheme of neurodegenerative disease. J Sport Health Sci 5: 383-7.
[Crossref] [Google Scholar] [Indexed]
- Yu F, Vock DM, Barclay TR (2017) Executive function: Responses to aerobic exercise in Alzheimer’s disease. Geriatric Nursing.
[Crossref] [Google Scholar] [Indexed]
- Sutoo D, Akiyama K (2003) Regulation of brain function by exercise. Neurobiol Dis 13: 1-14.
[Crossref] [Google Scholar] [Indexed]
- Hamer M, Chida Y (2009) Physical activity and risk of neurodegenerative disease. A systematic review of prospective evidence. Psychol Med 39: 3-11.
[Crossref] [Google Scholar] [Indexed]
- Larson EB, Wang L, Bowen JD, McCormick WC, Teri L et al (2006) Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med 144: 73-81.
[Crossref] [Google Scholar] [Indexed]
- Colcombe S, Kramer A (2003) Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol Sci 14: 125-130.
[Crossref] [Google Scholar] [Indexed]
- Steinberg M, Leoutsakos JM, Podewils LJ, Lyketsos CG (2009) Evaluation of a home based exercise program in the treatment of Alzheimer’s disease. The Maximizing Independence in Dementia study. Int J Geriatric Psychiatry 24: 680-5.
[Crossref] [Google Scholar] [Indexed]
- Meda L, Cassatella MA, Szendrei GI, Otvos L, Baron P et al (1995) Activation of microglial cells by β-amyloid protein and interferon-γ. Nature 374: 647-650.
[Crossref] [Google Scholar] [Indexed]
- Pitkala KH, Poysti MM, Laakkonen ML, Tilvis RS, Savikko N et al (2013) Effects of the Finnish Alzheimer disease exercise trial. A randomized controlled trial. Intern Med 173: 894-901.
[Crossref] [Google Scholar] [Indexed]
- Marks BL, Katz LM, Styner M, Smith JK (2011) Aerobic fitness and obesity: relationship to cerebral white matter integrity in the brain of active and sedentary older adults. Br J Sports Med 45: 1208–1215.
[Crossref] [Google Scholar] [Indexed]
- Barnes JN (2015) Exercise, cognitive function, and aging. Adv Physiol Educ 39: 55–62. 10: 1152.
[Crossref] [Google Scholar] [Indexed]
- Erickson KI, Prakash RS, Voss MW, Chaddock L, Morris KS et al (2009) Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus 19: 1030–1039.
[Crossref] [Google Scholar] [Indexed]
- Van de Winckel A, Feys H, DE Weerdt W (2004) Cognitive and behavioural effects of music-based exercises in patients with dementia. Clin Rehab 18: 253–260.
[Crossref] [Google Scholar] [Indexed]
- Stevens J, Killeen M (2006) A randomised controlled trial testing the impact of exercise on cognitive symptoms and disability of residents with dementia. Contemp Nurse 21: 32–40.
[Crossref] [Google Scholar] [Indexed]
- Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW et al (2010) Effects of aerobic exercise on mild cognitive impairment. Arch Neurol 67: 71–79.
[Crossref] [Google Scholar] [Indexed]
- Scherder EJA, van Paasschen J, Deijen JB, van der Knokke S, Orlebeke JFK (2005) Physical activity and executive functions in the elderly with mild cognitive impairment. Aging Ment Health 9: 272–280.
[Crossref] [Google Scholar] [Indexed]
- Van Uffelen JG, Chinapaw MJ, Van Mechelen W, Hopman-Rock M (2008) Walking or vitamin B for cognition in older adults with mild cognitive impairment? A randomized controlled trial. Br J Sports Med 42: 344–351.
[Crossref] [Google Scholar] [Indexed]
- Nagamatsu LS, Chan A, Davis JC, Beattie BL, Graf P et al (2013) Physical activity improves verbal and spatial memory in older adults with probable mild cognitive impairment: a 6-month randomized controlled trial. J Aging Res 861-893.
[Crossref] [Google Scholar] [Indexed]
- Smith PJ, Blumenthal JA, Hoffman BM (2010) Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials. Psychosomatic Medicine 72: 239-52.
[Crossref] [Google Scholar] [Indexed]
- Friedman R, Tappen R (1991) The effect of planned walking on communication in Alzheimer’s disease. J Am Geriatr Soc 39: 650–654.
[Crossref] [Google Scholar] [Indexed]
- Cott CA, Dawson P, Sidani S, Wells D (2002) The effects of a walking/talking program on communication, ambulation and functional status in residents with Alzheimer’s disease. Alzheimer Dis Assoc Disord 16: 81–87.
[Crossref] [Google Scholar] [Indexed]
- McGuinness B, Barrett SL, Craig D, Lawson J, Passmore AP (2010) Attention deficits in Alzheimer’s disease and vascular dementia. J Neurol Neurosurg Psychiatry 81: 157–9.
[Crossref] [Google Scholar] [Indexed]
- Ben-David BM, Tewari A, Shakuf V, Van Lieshout PH (2014) Stroop effects in Alzheimer’s disease: selective attention speed of processing, or color-naming.A meta-analysis. J Alzheimers Dis 38: 923–38.
[Crossref] [Google Scholar] [Indexed]
- Bossers WJ, van der Woude LH, Boersma F, Scherder EJ, van Heuvelen et al (2012) Recommended measures for the assessment of cognitive and physical performance in older patients with dementia: A systematic review. Dement Geriatr Cogn Dis Extra 2: 589–609.
[Crossref] [Google Scholar] [Indexed]
- Lafont S, Marin-Lamellet C, Paire-Ficout L, Thomas-Anterion C, Laurent B et al (2010) The Wechsler Digit Symbol Substitution Test as the best indicator of the risk of impaired driving in Alzheimer disease and normal aging. Dement Geriatr Cogn Disord 29: 154–63.
[Crossref] [Google Scholar] [Indexed]
- Hillman CH, Erickson KI, Kramer AF (2008) Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci 9:58–65.
[Crossref] [Google Scholar] [Indexed]
- Sofi F, Valecchi DB, Abbate R, Gensini GF, Casini A (2011) Physical activity and risk of cognitive decline: a meta-analysis of prospective studies. J Intern Med 107-117.
[Crossref] [Google Scholar] [Indexed]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO et al (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 39: 1435–1445.
[Crossref] [Google Scholar] [Indexed]
- Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C (2014) Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol 13: 788-794.
[Crossref] [Google Scholar] [Indexed]
- Coelho FG, Vital TM, Stein AM, Arantes FJ, Rueda AV et al (2014) Acute aerobic exercise increases brain-derived neurotrophic factor levels in elderly with Alzheimer’s disease. J Alzheimers Dis 39:40-408.
[Crossref] [Google Scholar] [Indexed]
- Pereira AC, Huddleston DE, Brickman AM, Sosunov AA, Hen R et al (2007) An in vivo correlate of exercise-induced neurogenesis in the adult dentate gyrus. Proc Natl Acad Sci USA 104: 5638-5643.
[Crossref] [Google Scholar] [Indexed]
- Hoffmann K, Sobol NA, Frederiksen KS, Beyer N, Vogel A et al (2016) Moderate-to-high intensity physical exercise in patients with Alzheimer’s disease: a randomized controlled trial. J Alzheimers Dis 50 443-453.
[Crossref] [Google Scholar] [Indexed]
- Ohman H, Savikko N, Strandberg TE (2016) Effects of Exercise on Cognition. The Finnish Alzheimer Disease Exercise Trial: A Randomized, Controlled Trial. J Am Geriatr Soc 64: 731-738.
[Crossref] [Google Scholar] [Indexed]
- Lautenschlager NT, Cox KL, Flicker L (2008) Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease A randomized trial 300: 1027-37.
[Crossref] [Google Scholar] [Indexed]
- Heyn P, Abreu BC, Ottenbacher KJ (2004) The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Meta-Analysis 85: 1694-704.
[Crossref] [Google Scholar] [Indexed]
- M Garuffi, JL Costa, SS Hernández TM, Vital AM, Stein JG et al (2013) Effects of resistance training on the performance of activities of daily living in patients with Alzheimer's disease Geriatr Gerontol Int 13: 322-328.
[Crossref] [Google Scholar] [Indexed]
- Fiatorone MA , Singh NG, N Saigal, GC Wilson, J Meiklejohn et al (2014) The study of mental and resistance training (SMART) study-resistance training and/or cognitive training in mild cognitive impairment: a randomized, double-blind, double-sham controlled trial. J Am Med Dir Assoc 15: 873-880.
[Crossref] [Google Scholar] [Indexed]
- Scarmeas N, Luchsinger JA, Brickman AM, Cosentino S, Schupf N et al (2011) Physical activity and Alzheimer disease course Am J Geriatr Psychiatry 19: 471-481.
[Crossref] [Google Scholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences