The Premier Nodal Platform- Sentinel Lymph Node
Anubha Bajaj*
Department of Pathology, Punjab University, Chandigarh, India
- *Corresponding Author:
- Anubha Bajaj
Consultant Pathologist, Department of Pathology
Punjab University, Chandigarh, India.
Tel: 098 1169 3956
E-mail: anubha.bajaj@yahoo.com
Received Date: May 02, 2018; Accepted Date: May 22, 2018; Published Date: May 30, 2018
Citation: Bajaj A (2018) The Premier Nodal Platform- Sentinel Lymph Node. J Biol Med Res. Vol.2 No.2:10
Abstract
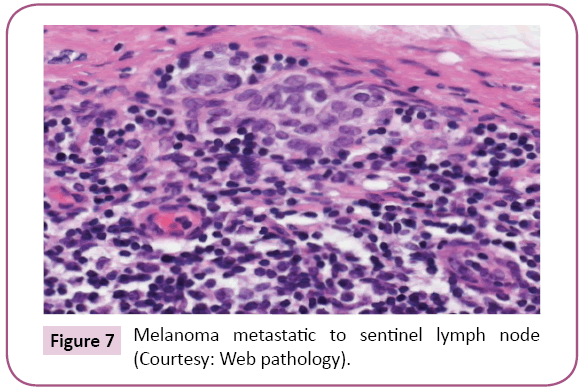
Sentinel Lymph Node (SLN) is an evaluation of malignant metastasis in regional lymph nodes. The draining lymph nodes pertinent to the malignant territory can be estimated with a minimal invasion and examination of a few lymph nodes. The sentinel lymph node is decreed as the first transformed node specific to the malignant segment (guard of the lymph nodes). SLN interpretation reduces the surgical insult and morbidity in contrast surgical resection accompanied with the traditional nodal sacrifice. The substance of lymph node metastasis in parotid carcinoma was the preliminary implementation of SLN followed by penile carcinoma. Analysis and metastasis of nodal breast carcinoma and melanoma are preponderantly discerned by SLN. The dissemination of gastro intestinal tumors and endocrine tumors is also reviewed. Primary surgical intervention based on the SLN evaluation is beneficial, however secondary, extensive surgery enhances the surgical insult. The lymphatic dissipation of the tumor decides the procedure of SLN. A gamma radiation discharging Sulphur colloid is injected throughout the tumor prior to surgery. Besides, a viable dye (iso-sulphan blue) can be introduced in the intra dermal site of incision. The blue gamma radiating nodes are recognized and biopsied. The methodologies may be implemented singly or in coalition. The truncal lymphatic drainage is unpredictable in the melanomas. Pre-operative lymphatic scintigraphy scanning elucidates the lymph nodes in the primary effluvium of the tumor. SLN of this domain can thus be biopsied. Occult micro metastatic conditions can be illustrated by the SLN. Tumor accumulations of <2 mm indicate a poor outcome. Optimal intervention can eliminate the malignant evolution. Thus, a malignant melanoma >0.75 mm thick, lacking nodal expression, requires an assay with SLN biopsy. Thinner melanomas infrequently present tumor positive lymph nodes. Delineation of a malignant melanoma metastatic to the lymph node is a verified, independent and distinct prognostic factor. Thus, malignant melanoma identifiable in the SLN stipulates a lymphatic eradication.
Keywords
Axillary lymph node; Sentinel lymph node
Abbreviations
OS: Overall Survival; DFS: Disease Free Survival; SLN: Sentinel Lymph Node Biopsy; ALN: Axillary Lymph Node; ALND: Axillary Lymph Node Dissection; FS: Frozen Section; CK: Cyto Keratin; mRNA: Messenger RNA; ECE: Extra Capsular Extension; IOE: Intra-Operative Evaluation; NASBP-B32: National Surgical Adjuvant Breast and Bowel Project; IHC: Immunohistochemistry; AJCC: American Joint Committee on Cancer; ACOSOGZ0011: The American College of Surgeons Oncology Group; AMARO: After Mapping of Axilla: Radiotherapy or Surgery; IBCSG: International Breast Carcinoma Study Group; ASCO: American Society of Clinical Oncology; FS: Frozen Section
Introduction
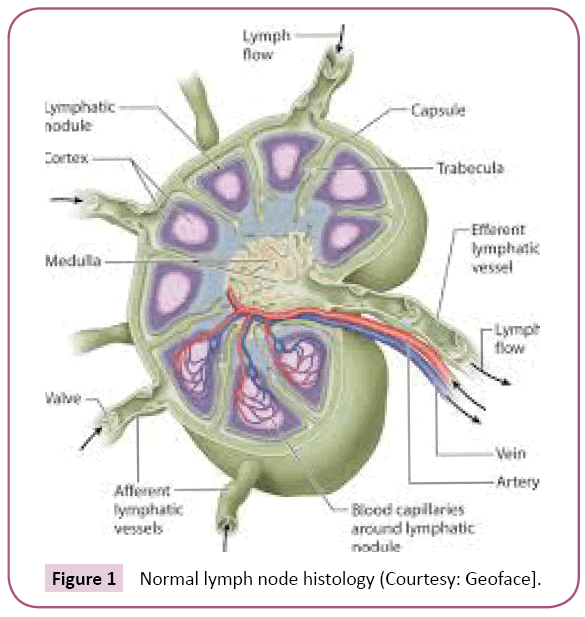
Axillary lymph node
Grading of axillary lymph node (ALN) is a valuable consideration in the prognosis of breast carcinoma. ALN dissection was initially employed for tumor staging [1]. Axillary Lymph Node dissection(ALND) in women with invasive breast carcinoma eventuates morbidity and delayed complications which affect the quality of life such as restricted shoulder activity, paranesthesia, limb paralysis and lymphedema [1,2]. Lymph node staging determines the axillary specifications in breast carcinoma Sentinel lymph node (SLN) biopsy is employed to diminish the complications of axillary surgery. The SLN is the initial, primary node draining a tumor zone, thus evolves into the first location of lymph node metastasis. Contemporary breast carcinomas may be miniscule, with a diminished nodal tumor load. Majority of the patients are managed with adjuvant systemic chemotherapy which regulates the local/systemic neoplasm. SLN is comparable to axillary staging in node negative individuals (cN0) [3]. ALND may be excluded in limited cN0 patients with metastatic carcinoma restricted to one or two SLNs [4]. This approach modifies the clinical practice with connotations on SLN evaluation (Figure 1).
ALN performance
The nodal contamination is assessed as per the tumor stage as defined by the TNM staging system and the AJCC (American joint committee on cancer) Macro-metastasis are the tumor deposits >2 mm (p N1), micro-metastasis varies from 0. 2 – 2 mm and comprise of about 200 carcinoma cells in a single section of the lymph node (pN1mi). Isolated tumor cells (ITC) are single cells or cell aggregates <0.2 mm and accumulate <200 carcinoma cells in one lymph node section [pN0 (i+)] irrespective of the method of discovery (Table 1).
| pN0 (1+) | Isolated tumour cells or cell deposits no larger than 0.2 mm or fewer than 200 cells |
| pN1 (mi) | Metastasis > 0.2 mm and /or > 200 cells, but none greater than 2.0 mm |
| pN1 (a) | Macromutations in 1 to 3 ALN (at least 1 tumour deposit> 2.0 mm). |
| pN2 (a) | Macromutations in 4-9 ALN (at least 1 tumour deposit> 2.0 mm). |
| pN3 (a) | Macro metastasis in 10 or more ALN (at least 1 tumour deposit> 2.0 mm) |
Table 1: American Joint Committee of Cancer TNM (7th edition).
Literature Review
Metastatic carcinoma unmasked by molecular testing utilizes the (pN0mol+) label. As per the current AJCC manual, discarding lymph node tissue for molecular analysis, which could be utilized for histopathology and tumor staging, is not advisable particularly when the forfeited tissue comprises of a macro-metastasis.
Precision axillary staging
cN0 patients require an SLN. NSABP – B32 CLINICAL TRIAL: The National Surgical Adjuvant Breast and Bowel project (NSABP B32) randomized prospective clinical trial institutes the SLN biopsy as a safe, efficient technique of axillary staging. Thus, the SLN biopsy is comparable to ALND in the T1 and T2 tumors. SLN biopsy of the cN0 invasive breast carcinoma demonstrates a false negative rate of 7.3% (delineated by a single H&E section per block). The false negative SLN biopsies are elucidated in lobular or poorly differentiated carcinoma, prominent duct histology and/or partial nodal substitution.
Connotations of occult metastases
An occult metastasis is one which is not delineated and is overlooked on initial observation utilizing a conventional protocol. Enhanced pathology ascertains the occult metastasis and surmises patient outcome. Characteristically, it recruits H&E step level sections from SLN blocks which lack the indication of carcinoma. The NSABP B32 analysis elucidates therapeutic possibilities, clinical implications or occult metastasis. The SLNs are segmented at a 2 mm distance, embedded in paraffin and the blocks are evaluated - one H&E stained slide per block. The macro metastasis (>2 mm) are discerned. Extended assessment with experimental B32 protocol is performed with blocks which are inadequate. Sections at 0.5 mm and 1.0 mm gap from the paraffin blocks are stained with H&E and CK-IHC to reveal metastasis >1 mm in size. Age <50 years, tumor size >2.0 cm and planned mastectomy are factors which contribute to occult metastasis. Systemic therapy (hormonal/chemotherapy), outlined by the clinical/pathologic features, are prescribed to the individuals. Occult SLN metastasis obligates chemotherapy and/ or endocrine therapy. Comprehensive protocol is employed in the H&E stained sections of the nodal blocks displaying minimal metastasis. Supplementary CK-IHC sections through the entire block at 0.18 mm depth are salvaged to expose metastasis 0.2 mm or more in size. All tumors do not relapse, and patients are prescribed numerous therapeutic options, so the protocol may seem superfluous. SLN and ALN staging is recommended by interpreting one H&E stained section [5].
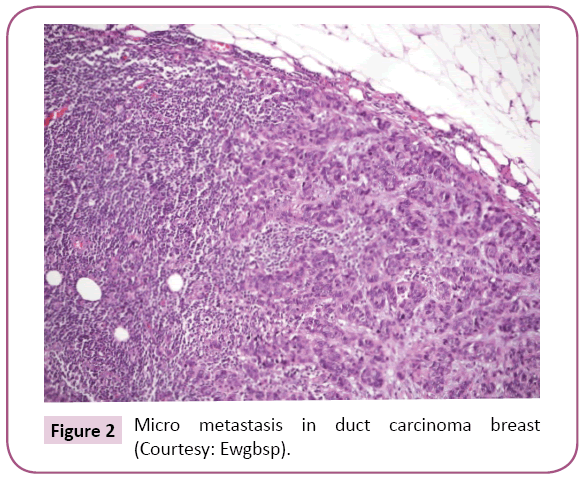
Essence of micrometastasis
Metastasis 0.2 mm to 2.0 mm in diameter is elucidated as micro-metastatic breast carcinoma. Micro metastasis displays a superior OS in contrast to macro-metastasis (>2 mm). The Surveillance, Epidemiology and End result (SEER) evaluation denotes poorer survival in individuals with micro metastasis in contrast to patients with absent metastasis (hazard ratio 1.35). However, the survival is much improved when compared to the individuals displaying macro-metastasis (hazard ratio 0.86) [6] (Figure 2).
Adjunct metastasis with conclusive (positive) SLN
The axillary disease residuum is inconsistent (40%) Thus ALND provides no advantage and ramifications may ensue. Varied clinico-pathologic specifications and prognostic mathematical implementations, denominated as nomograms, are utilized to appraise the nodal metastasis [7]. Nomograms assign criterion such as tumor size, tumor type, nuclear grade, lymph vascular invasion, multifocal metastasis, estrogen receptor(ER) status, mode of analyzing SLN tumor deposits, intra operative detection, routine H&E staining, serial H & E stained sections in conjunction with IHC and the quantification of positive and negative SLN’s, to evaluate the ALN disease residuum. The precise, distinctive receiver operating characteristic (ROC) curve thus formulated is at 0.76 (range 0.71 to 0.82). Specific histology and clinical guidelines are attributed to the drafting of ROCs and nomograms. It depicts the percentage probability of adjunctive ALN metastasis.
Exhaustive ALND in SLN metastasis
The American college of surgeons oncology group (ACOSOG Z0011) prospective randomized clinical trial estimates the benefit of ALND with 1-2 SLNs denoting metastasis. Diagnostic parameters enumerate the invasive breast carcinoma as <5 cm diameter and which lack palpable ALNs (T1 or T2 with cN0) (Table 2).
| NASBP-B-32 | Negative | SLN alone versus SLN B +ALND in T1 or T2 cN0 patients undergoing mastectomy or BCS |
| IBCSG 23-01 | Positive. 1 or more micro metastasis | SLN alone versus SLN B +ALND in T1 or T2 cN0 patients undergoing mastectomy or BCS |
| ACOSOG Z0011 | Positive. 1 or 2 positive SLN | SLN alone versus SLN B +ALND in T1 or T2 cN0 patients undergoing BCS or whole breast irradiation. |
| AMAROS | Positive. 1 or 2 positive SLN | ALND versus axillary radiotherapy in T1 or T2 cN0 patients undergoing mastectomy or BCS |
Table 2: Major SLN trials.
Discussion
Metastasis are delineated in 1-2 SLNs (H&E) and managed with breast conservation because of tumor – free surgical margins with whole breast irradiation.
Parameters for elimination from the trial are
1. Three or more SLNs depicting metastasis (on H&E).
2. Entangled (matted) lymph nodes
3. Gross extra capsular extensions (ECE).
4. SLN metastasis recognized on CK-IHC.
5. Total mastectomy.
6. Radiotherapy to the axilla.
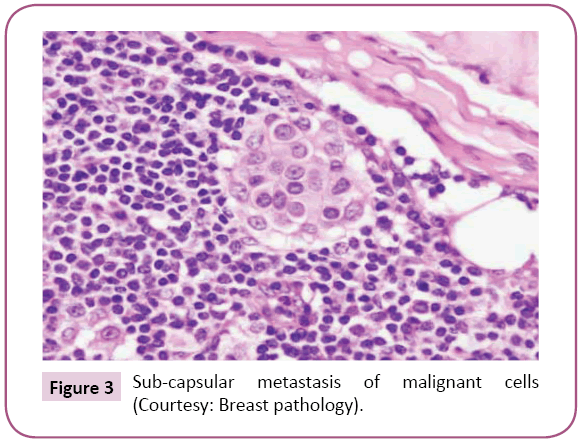
Adjuvant systemic chemotherapy is recommended for patients interpolated in the trial. Breast conservation surgery and whole breast irradiation is utilized for T 1 and T2 tumors with two or <2 or implicated SLNs. Such patients are marginally ameliorated with ALND. Thus, as per ASCO guidelines (2014), comprehensive ALND for cases with <three metastatic SLN in the absence of massive metastasis or apparent ECE and with whole body irradiation are not recommended. ALND and/or Radiotherapy are advised for individuals with diagnosed metastatic SLNs [8] (Figure 3).
Figure 3: Sub-capsular metastasis of malignant cells (Courtesy: Breast pathology).
Amaro trial
The AMARO (After Mapping the Axilla: Radiotherapy or Surgery?) prospective randomized control trial elucidates guidelines for the tumor control in the axilla of T1/T2 patients with detectable SLNs [9]. Arbitrary selections to ALND or axillary radiotherapy are performed. The axillary reoccurrence, DFS or OS are comparable with both therapies. ALND is accompanied with lymph-oedema, in contrast to a localized radiotherapy (23 versus 11%). However, the therapeutic strategies can produce an equivalent axillary tumor containment. Axillary reoccurrence can be palliated in the absence of ALND or radiotherapy (as detailed in the Z0011). Evaluation of mastectomy in a subset of the AMAROS trial could be beneficial.
Extra Capsular Extension (ECE)
Breast carcinoma can metastasize in the fibro adipose tissue of the axilla. ECE should be noted and communicated. Magnitude of invasion beyond the lymph node capsule is observed besides the extent of the nodal metastasis Focal ECE is evidenced in 19-30% of the cN0 SLNs [10]. Also, early breast carcinoma may produce the non SLN metastasis. ECE forecasts a poor prognosis. It acts in conjunction with predictors such as lympho-vascular invasion and SLN macro metastasis. The College of American Pathologists advocates describing the ECE as “Present” instead of “Not identified” or “Indeterminate”. ECE appears in the older patients, with larger, multifocal, estrogen receptor positive tumors which delineate lympho-vascular ingress. ECE of dimensions >2 mm are frequently associated with adjunct nodal metastasis versus an ECE <2 mm. Thus, an ECE>2 mm area when combined with the Z0011 guidelines may imply an extended treatment of the axilla.
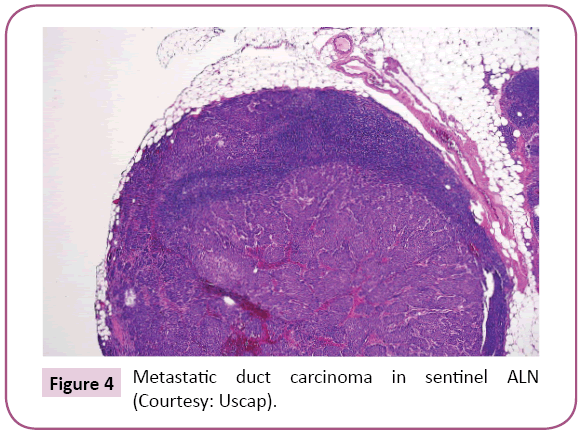
Intra Operative Evaluation (IOE) of SLNs
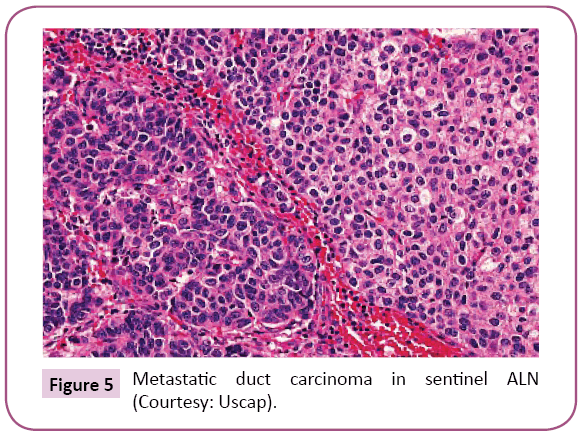
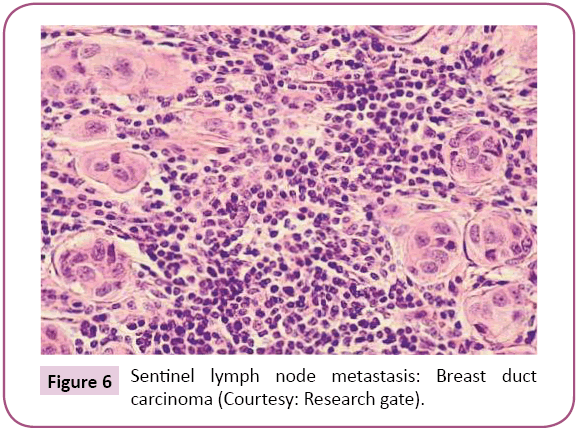
Intra operative identification of breast carcinoma metastasis in the SLN may culminate in ALND, thereby preventing a second surgery. IOE of the SLN results in enhanced duration of surgery and probable false positive conclusions. Frozen section (FS), imprint cytology/touch preparation or a cytology smear can be employed for IOE of the SLNs. Cytology preparations deliver a quick outcome than the FS with minimal tissue deprivation of the node. The Cytology methods may be disputable for confirmation of the diagnostic features, which require corroboration on tissue sections. Imprint cytology has a detection rate of macro metastasis as 81% and that of micro-metastasis as 22%. Frozen section (FS) is a slow process as freezing instils tissue distortion artefacts, slicing the FS block could decimate the analytical features. However, FS remains the procedure of choice for IOE. FS is reliable in macro metastasis, in contrast to the micrometastasis (94% versus 40% detection rate). The Cytology touch preparations, cytology smears and the FS display comparable sensitivities (59%, 57%, and 59% respectively). Each procedure displays a higher sensitivity for discovering macro- metastasis (96%, 93% and 93% respectively) rather than micro-metastasis (27%, 27% and 30%). One step nucleic acid amplification is a molecular technique that assesses the CK 19 mRNA in a homogenized preparation of SLN and is used for IOE. One step nucleic acid amplification is extremely susceptible to the evaluation of minimal nodal metastasis. Tissue homogenization is a pre-requisite for analysis. It calculates relevant morphological characters such as the magnitude of the metastasis and ECE [11]. The application of Z0011 trial has diminished the employment of IOE. The ALND manifests when the clinical and decisive pathological input is entirely accessible. Multidisciplinary teams may utilize the IOE to evolve treatment protocols contingent to the local practice (Figures 4-7).
Histologic assessment of SLN
This is accomplished as per CAP and ASCO guidelines. A definitive sentinel node assay constitutes of accurate gross and histological evaluation. The number of sentinel lymph nodes discovered with metastasis decides if a patient of T1 or T2 cN0 and qualifies for the Z0011 trial guidelines. The sentinel lymph node is visualized, the enveloping adipose tissue is eliminated, and the number of nodes is ascertained. Each sentinel LN is slivered into 2 mm thick slices parallel to the nodal long axis [12]. One H&E section per block is observed to visualize the entire SLN segment besides the sub-capsular space and the nodal capsule. Cytokeratin stained section are obtained with IHC.
Conclusion
Adjunctive sections at additional levels can be studied to evaluate specific morphological alterations. The final communication should consist of the total number of SLN, the percentage/ number of SLN displaying metastatic carcinoma, the dimensions of the metastasis and the elucidation of ECE. (present, absent, indeterminate) besides the area of ECE (<2 mm, 2 mm or >2 mm).
References
- Borup Christensen S, Lundgren E (1989) Sequelae of axillary dissection versus axillary sampling with or without irradiation for breast carcinoma: A randomized control trial. Acta Chirugica Scand 155: 515-519.
- Kell MR, Burke JP, Barry M, Morrow M (2010) Outcome of axillary staging in early breast carcinoma: a meta-analysis. Breast Carcinoma Res Treatment 120: 441-447.
- Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, et al. (2010) Sentinel lymph node resection compared with compared with conventional axillary lymph node dissection in clinically node negative patients with breast carcinoma: overall survival findings from the NSABP=B32 randomized phase 3 trial. Lancet Oncol 11: 927-933.
- Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, et al. (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: A randomized clinical trial. JAMA 305: 569-575.
- Invasive Breast Cancer Version 1 (2015) NCCN Clinical Practice Guidelines in Oncology.
- De Boer M, Van Dijck JA, Bult P, Borm GF, Tjan-Heijnen VC (2010) Breast carcinoma prognosis and occult lymph node metastasis, isolated tumour cells and micro metastasis. J Natl Cancer Inst 102: 410-425.
- Houvenaeghel G, Nos C, Giard S, Mignotte H, Esterni B, et al. (2009) A nomogram predictive of non-sentinel lymph node involvement in breast cancer patients with a sentinel lymph node micrometastasis. Eur J Surg Oncol 35: 690-695.
- Tiernan JP, Verghese ET, Nair A, Pathak S, Kim B, et al. (2014) Systematic review and meta-analysis of cytokeratin 19-based one-step nucleic acid amplification versus histopathology for sentinel lymph node assessment in breast cancer. Br J Surg 101: 298-306.
- Boughey JC (2014) How do the AMAROS trial results change practice. Lancet Oncol 15: 1280-1281.
- Kell MR, Kerin M (2004) Sentinel lymph node biopsy. BMJ 328: 1330.
- Maguire A, Brogi E (2016) Sentinel lymph nodes for breast carcinoma: A paradigm shift. 140: 791-798.
- Apple SK (2016) Sentinel lymph node in breast carcinoma: A review article from a pathologist’s point of view. J Pathol Transl Med 50: 83-95.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences