The Effect of a Body-Weight Supported Treadmill Rehabilitation Program on Gait Symmetry Restoration in Patients with Various Neurological Conditions
Eldar Vinarov*
Physiotherapist at Cerebrum Clinic, Tashkent, Uzbekistan
- *Corresponding Author:
- Eldar Vinarov
Physiotherapist at Cerebrum Clinic, Tashkent,
Uzbekistan,
E-mail: eldar.vinarov@gmail.com
Received date: January 22, 2024, Manuscript No. IPJNDD-24-18567; Editor assigned date: January 25, 2024, PreQC No. IPJNDD-24-18567 (PQ); Reviewed date: February 08, 2024, QC No. IPJNDD-24-18567; Revised date: February 15, 2024, Manuscript No. IPJNDD-24-18567 (R); Published date: February 22, 2024, DOI: 10.36648/ipjndd.7.1.5
Citation: Vinarov E (2024) The Effect of a Body-Weight Supported Treadmill Rehabilitation Program on Gait Symmetry Restoration in Patients with Various Neurological Conditions. J Neurodegenero Dis Disord Vol.7 No.1: 5.
Abstract
Background: As neurological conditions are considered the leading cause of disability and the second leading cause of death worldwide, it is necessary to respond to their increased burden by introducing new medical technologies enabling safe, effective and time-saving rehabilitation.
Materials and methods: A total of 39 neurological patients from 3 indication groups (neuromuscular diseases and disorders, paresis after stroke and postoperative/post injury states of CNS and PNS) completed a treatment program involving six body-weight supported treadmill exercise sessions combined with conventional rehabilitation. Symmetry indexes of gait parameters (stance time, step length, step time, swing time, swing/stance time ratio and weight loading proportion) measured during the first and last session were statistically processed and evaluated.
Results: The asymmetry of all monitored gait parameters improved statistically significantly within the entire cohort of treated patients by 40%, 50%, 61%, 62%, 67% and 68% in terms of stance time, step length, step time, swing time, swing/stance time ratio and weight loading proportion, respectively. The comparison of the indication groups shows that post-stroke patients achieved the highest average improvement across all gait parameters.
Conclusion: The research was the first to prove the effectiveness of Body-Weight Supported Treadmill (BWST) therapy in restoring gait symmetry in neurological patients. Presented findings predispose BWST therapy to become an integral part of the gait retraining program already in the early phase of rehabilitation.
Keywords
Treadmill rehabilitation; Gait parameters; Neuromuscular diseases; Neurological conditions; Neurological disorders
Introduction
With the growth and aging of the population, there is a global increase in the prevalence of neurological disorders and the associated demands for treatment, rehabilitation and supportive care of neurological patients. Given that neurological conditions are considered the leading cause of disability and the second leading cause of death worldwide, it is necessary to respond to their increased burden by introducing new medical technologies enabling safe, effective and time-saving rehabilitation [1]. The main limitations of these patients are difficulties with walking and above all the loss of mobility, which represents the most valued activity [2]. Up to 60% of neurological patients suffer from impaired mobility caused by gait and balance disorders. These limitations can have a major impact on the patient's independence in performing daily activities, his involvement in social life and overall quality of life. Gait impairment in neurological patients is often associated with an increased risk of falling, subsequent musculoskeletal injury and risk of death [3]. Up to 46% of neurological patients experience one or more falls per year and the incidence of falls is approximately 2-4 times higher than in healthy individuals of the same age. Existing clinical research suggests a possible link between fall risk and some gait parameters and their between-limb asymmetry [4].
Identical behavior of the limbs during the gait cycle leads to a symmetrical gait pattern, which, however, can be disturbed due to pain or as a result of underlying impairment. In the long term, the persistence of an asymmetric gait pattern can lead to the development of associated musculoskeletal problems. For example, the uneven distribution of limb load in post-stroke patients leads to a loss of bone mineral density in the paretic limb, patients with unilateral amputation or osteoarthritis may suffer from low back pain, osteoarthritis or even amputation of a healthy limb. The design of the gait retraining protocol should therefore be designed in such a way that gait asymmetry is reduced or completely eliminated already in the early phase of rehabilitation [5].
Due to the health limitations of neurological patients and their increased risk of falls, the Body-Weight Supported Treadmill (BWST) is the only suitable method of gait retraining. During walking, the patient's lower half of the body is ixed in an overpressure chamber, which allows partial or complete relief of his body weight and at the same time makes it impossible to fall. The elimination of overloading of the lower limbs reduces the need for the patient to compensate for the movement with an uneven load and thus allows the restoration of the symmetrical pattern earlier compared to standard overground rehabilitation.
The BWST principle of gait symmetry restoration was confirmed in patients recovering after total joint replacement surgery and in a case series study also in patients with various neurological disorders [6-8]. Although there are studies focusing on the effect of BWST on gait asymmetry in post-stroke patients, there is practically no evidence of a positive impact of this therapy on the symmetry of gait parameters during the gait retraining program. While Hassid et al. rather focused on evaluating the correlation between BWST therapy settings and single limb stance time ratio and loading ratio, Combs et al. were not able to demonstrate a positive effect of BWST on gait symmetry restoration for any gait parameter [9,10]. Despite the absence of direct evidence of asymmetry improvement in neurological patients, the benefit of BWST therapy has been demonstrated in patients with multiple sclerosis, spinal cord injury, cerebral palsy, Parkinson's disease and post-stroke survivors [11-21].
The primary aim of the present study is to evaluate the effect of BWST therapy on the reduction of gait asymmetry in neurological patients. A secondary aim is to compare the results across various neurological diseases: Post-stroke paresis, neuromuscular disease and postoperative/post injury states of the Central Nervous System (CNS) or Peripheral Nervous System (PNS). This research is unique in its scope, allowing mutual comparison of effectiveness for individual neurological conditions. Clinical evidence in this regard is still insufficient as there is a complete lack of research into the effect of BWST on gait asymmetry in patients with neuromuscular diseases or postoperative conditions of CNS or PNS.
Materials and Methods
Patients suffering from one of three neurological disorders neuromuscular disease, post-stroke paresis or after surgery/injury of the CNS or PNS were recruited. Patients who, in addition to a neurological disorder, also suffered from some contraindication bronchial asthma, angina pectoris, severe cardiovascular disease, disc herniation, pregnancy, epilepsy or any conditions with increased abdominal pressure were excluded. Before starting the treatment program, all patients were properly informed about its course and possible risks and were then asked to sign an informed consent. The study met the criteria of the 1975 declaration of Helsinki Ethical Guidelines adopted by the Convention on Human Rights and Biomedicine of the Council of Europe (1997) and by the General Assembly of the World Medical Association (1997-2000) [22].
As this is the very first study on neurological patients, it was not possible to estimate the sample size based on the published results. For that reason, the minimum number of patients was estimated based on research performed on patients with musculoskeletal disorders at least 33 patients were required to detect statistical significance of 0.05% with a power of 80% [6,7].
As part of the treatment program, participants completed 6 BWST gait retraining sessions followed by conventional rehabilitation. These combined sessions were scheduled three days apart and data acquisition using pressure sensors (H8C cell load) integrated within the treadmill path was part of each BWST exercise. In the current research, a positive pressure BWST (BTL Industries, Ltd.) was used, which, unlike its predecessors, does not create a tensile force on the patient due to suspension vests and other accessories. The principle of positive pressure enables completely natural walking without a negative effect on gait parameters [23]. Before the start of the therapy, the patient is fixed in an inflatable bag surrounding the treadmill path and the lower half of the patient's body. Special shorts equipped with a half zipper, which can be zipped into the bag opening, are used for this purpose. The device is then calibrated to the patient's weight and adjusted to their physical and health capabilities. It enables adjusting treadmill inclination in the range of 0%-15%, unweighting element in the range of 0%-100% and speed from -8 km/h to 25 km/h. The settings are adjusted by the operator before each session and at least minimal patient progress is assumed during each exercise. During the therapy, the inflatable bag is inflated and thereby lightens the patient's weight by the desired proportion. The patient can thus fully concentrate on walking correctly without fear of overloading or falling.
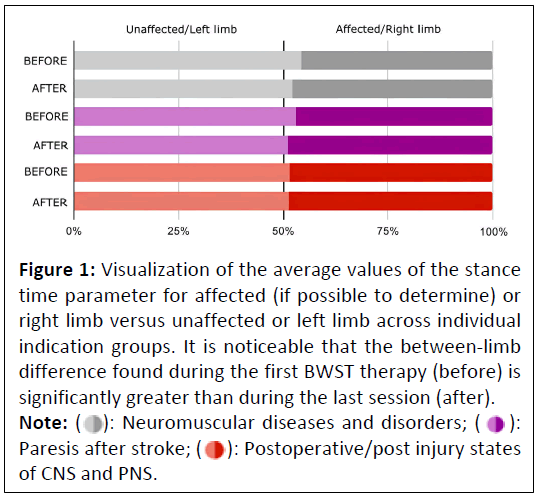
Gait parameters including stance time, step time, step length, swing time and weight bearing proportion were recorded for the left and right limbs. The values measured during the first and last exercise session were used to evaluate BWST effectiveness. Subsequently, the swing/stance time ratio was determined and the Symmetry Index (SI) was calculated for all values using the following formula:
Where:
PR=Value of the parameter measured on the right or affected limb, if it was possible to determine this side in the patient.
PL=Value of the parameter measured on the right or unaffected limb, if it was possible to determine this side in the patient.
While SI level=0% means complete symmetry, SI level=100% corresponds to complete gait asymmetry.
Data processing for the purposes of visual representation and statistical evaluation was performed in the Matlab programming environment using a custom written script. (MatLab R2010b, Mathworks, Inc., Narick, MA, USA). In the first step, the data were tested for normality using the Shapiro-Wilk test. As the normal distribution was rejected, the statistical significance of the achieved result of the treatment program was evaluated by the non-parametric Wilcoxon Sign Rank test.
Results
The total number of 40 recruited patients with various neurological disorders, 39 completed the entire treatment program. One patient did not complete the full study course due to his decision not to participate in the study any further. During the entire program, none of the patients experienced any side effects; the therapy was generally well accepted. The distribution of individual indications and patient demographics are shown in Table 1.
| Total number | Gender, male/female | Age, mean (SD) | |
|---|---|---|---|
| Neuromuscular diseases and disorders | 22 | 12/10 | 61.86 (11.43) |
| Paresis after stroke | 8 | 5/3 | 73.63 (8.53) |
| Postoperative/post injury states of CNS and PNS | 9 | 5/4 | 45 (4.61) |
| Total | 39 | 22/17 | 60.38 (13.58) |
Table 1: Demographics and distribution of indications in study participants.
comparison of symmetry index values for individual gait parameters measured during the first and last session across individual neurological indications is shown in Table 2. Improvement in asymmetry was noted for all gait parameters across all indication groups. The evaluation of the results within the entire treated cohort showed a statistically significant improvement in gait symmetry for all monitored gait parameters.
| Gait parameter | Indication | Before | After | Improvement (%) | P |
|---|---|---|---|---|---|
| Stance time SI | Neuromuscular diseases and disorders | 12.06 | 4.86 | 59.72 | <0.001 |
| Paresis after stroke | 11.78 | 3.6 | 69.43 | 0.016 | |
| Postoperative/post injury states of CNS and PNS | 15.84 | 5.44 | 65.67 | 0.02 | |
| Total | 12.73 | 4.96 | 61.01 | <0.001 | |
| Step length SI | Neuromuscular diseases and disorders | 5.03 | 2.99 | 40.58 | 0.073 |
| Paresis after stroke | 7.57 | 4.08 | 46.11 | 0.109 | |
| Postoperative/post injury states of CNS and PNS | 9.52 | 5.41 | 43.24 | 0.04 | |
| Total | 6.06 | 3.64 | 40 | 0.002 | |
| Step time SI | Neuromuscular diseases and disorders | 15.17 | 7.71 | 49.19 | 0.019 |
| Paresis after stroke | 14.88 | 5.48 | 63.2 | 0.016 | |
| Postoperative/post injury states of CNS and PNS | 14.42 | 9.46 | 34.36 | 0.027 | |
| Total | 14.42 | 7.15 | 50.39 | <0.001 | |
| Swing time SI | Neuromuscular diseases and disorders | 24.93 | 14.28 | 42.71 | <0.001 |
| Paresis after stroke | 29.32 | 9.12 | 68.9 | 0.008 | |
| Postoperative/post injury states of CNS and PNS | 24.4 | 6.96 | 71.46 | 0.02 | |
| Total | 25.16 | 9.49 | 62.31 | <0.001 | |
| Swing/stance time SI | Neuromuscular diseases and disorders | 34.89 | 12.51 | 64.14 | <0.001 |
| Paresis after stroke | 41.61 | 12.22 | 70.64 | 0.008 | |
| Postoperative/post injury states of CNS and PNS | 38.17 | 10.96 | 71.3 | 0.012 | |
| Total | 37.63 | 11.89 | 68.39 | <0.001 | |
| Weight bearing proportion SI | Neuromuscular diseases and disorders | 12 | 4 | 66.67 | <0.001 |
| Paresis after stroke | 10 | 4 | 60 | 0.09 | |
| Postoperative/post injury states of CNS and PNS | 12 | 8 | 33.33 | 0.02 | |
| Total | 12 | 4 | 66.67 | <0.001 |
Table 2: Development of gait asymmetry in terms of symmetry index for individual indication groups during the treatment program. A value of P<0.05 determined using the Wilcoxon sign rank test is considered statistically significant.
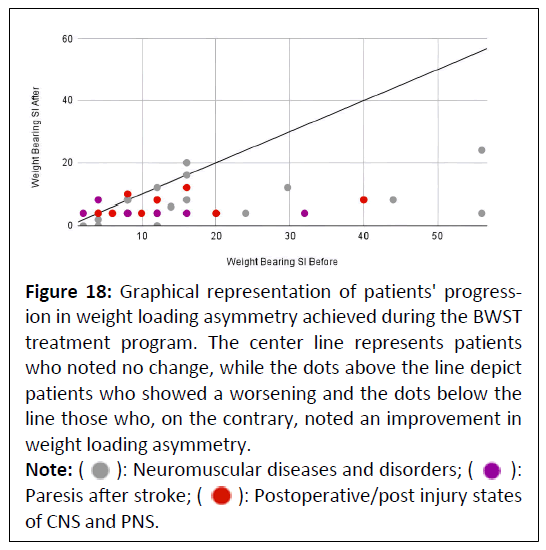
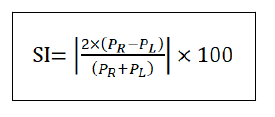
Stance time
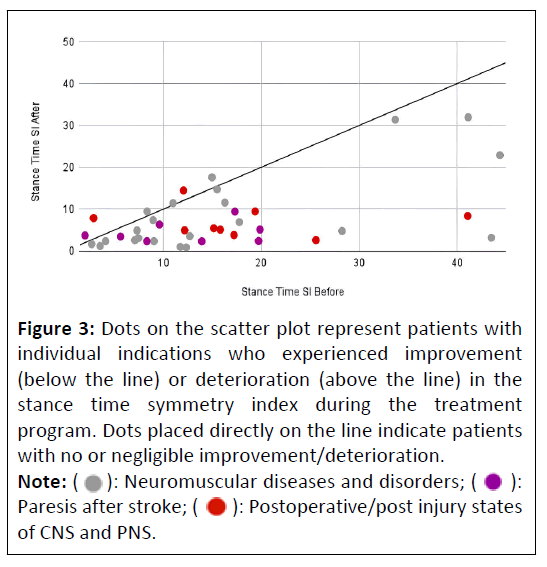
The between-limb difference in stance time decreased statistically significantly during the treatment program in the entire patient cohort as well as within the individual indication groups. Post-stroke survivors experienced the greatest reduction in asymmetry, patients recovering from neuromuscular diseases and disorders experienced the smallest reduction, still achieving almost a 60% improvement (Table 2). While the decreasing trend of the between-limb difference in stance time is visualized in Figure 1, the development and distribution of the symmetry index data across the indication groups are shown in Figure 2. From Figure 3, it can be seen that out of a total of 39 patients, only 6 patients did not experience improvement and therefore, it can be concluded that almost 85% of patients improved their gait symmetry from the standpoint of the stance time parameter.
Figure 1: Visualization of the average values of the stance time parameter for affected (if possible to determine) or right limb versus unaffected or left limb across individual indication groups. It is noticeable that the between-limb difference found during the first BWST therapy (before) is significantly greater than during the last session (after).
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 2: Box plot graph showing the evolution of the stance time symmetry index distribution during the first (before) and last (after) BWST session for individual indication groups.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 3: Dots on the scatter plot represent patients with individual indications who experienced improvement (below the line) or deterioration (above the line) in the stance time symmetry index during the treatment program. Dots placed directly on the line indicate patients with no or negligible improvement/deterioration.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Step length
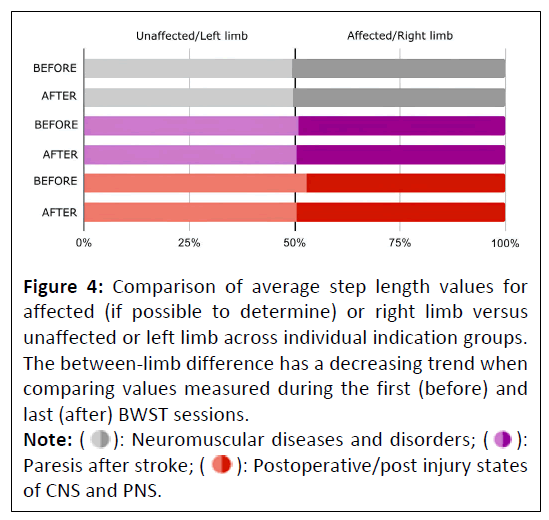
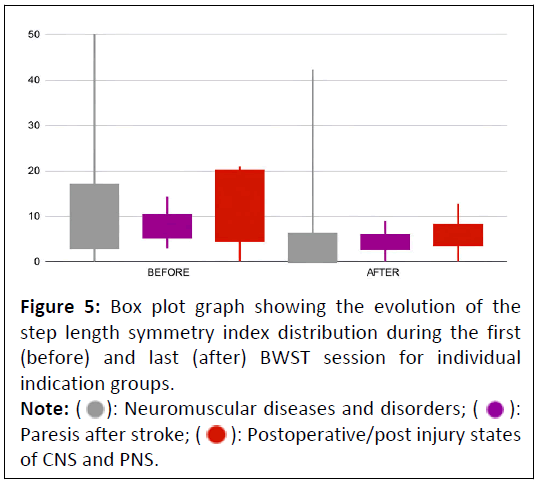
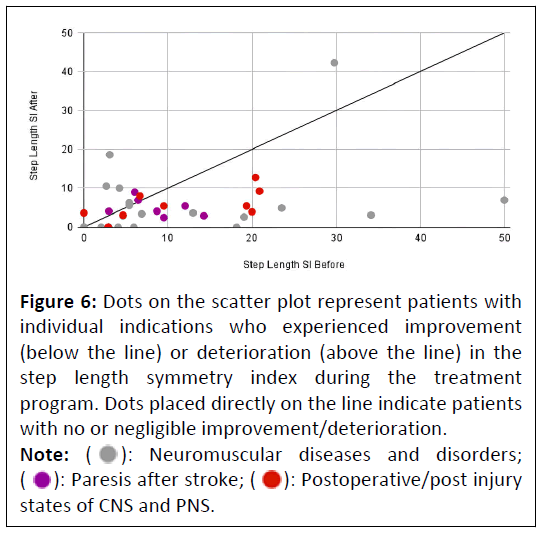
Although an improvement in step length asymmetry was noted within the entire cohort of neurological patients, in some indication groups this improvement did not reach statistical significance, specifically in patients recovering from neuromuscular diseases and disorders and in post-stroke patients. It can be seen from Figure 4 that these two indication groups already showed a minimum level of between-limb difference in step length before the start of the treatment program. In its course, an average improvement of 40% was recorded (Table 2), which is also confirmed by the decreasing trend of the symmetry index in Figure 5. A total of 10 patients did not experience improvement and therefore almost 75% of patients experienced a reduction in step length asymmetry (Figure 6).
Figure 4: Comparison of average step length values for affected (if possible to determine) or right limb versus unaffected or left limb across individual indication groups. The between-limb difference has a decreasing trend when comparing values measured during the first (before) and last (after) BWST sessions.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 5: Box plot graph showing the evolution of the step length symmetry index distribution during the first (before) and last (after) BWST session for individual indication groups.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 6: Dots on the scatter plot represent patients with individual indications who experienced improvement (below the line) or deterioration (above the line) in the step length symmetry index during the treatment program. Dots placed directly on the line indicate patients with no or negligible improvement/deterioration.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
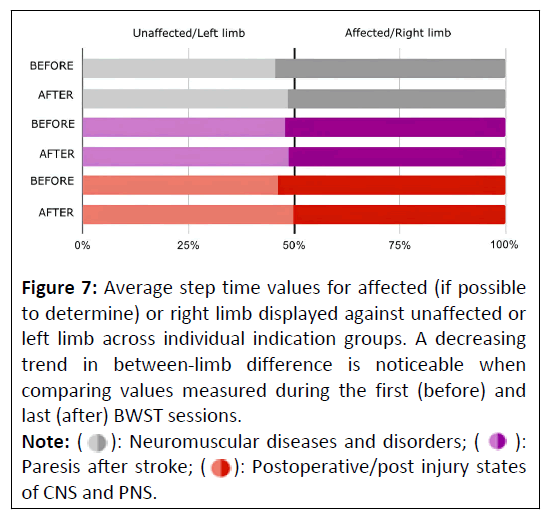
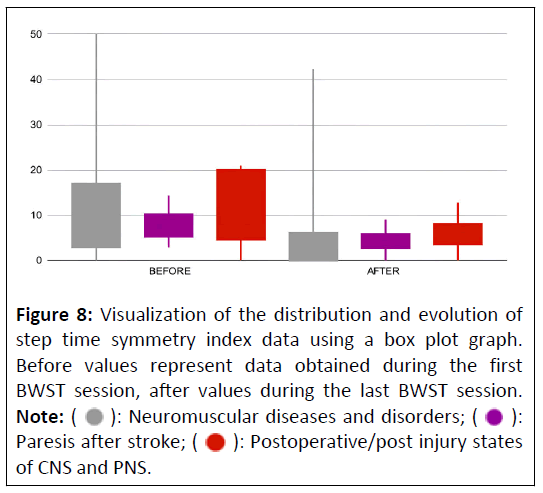
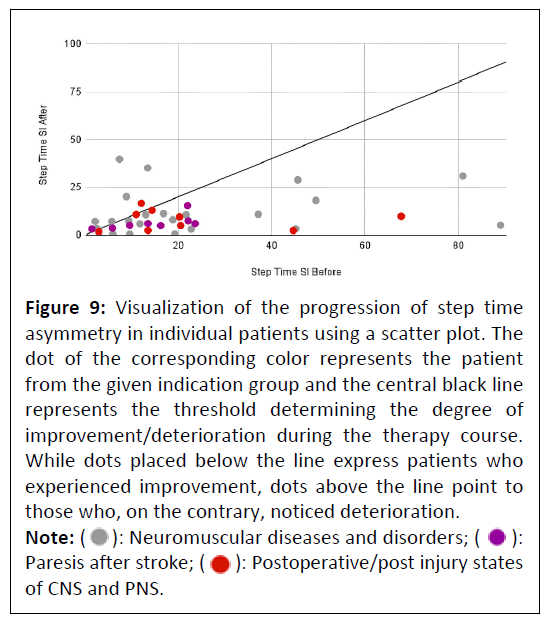
Step time
Patients of all indication groups reported a statistically significant improvement in step time asymmetry during six BWST sessions by an average of 50%. While the largest reduction exceeding 63% was recorded by post-stroke patients, the least significant improvement was observed in patients after CNS and PNS surgery or injury, by almost 35% (Table 2). These findings are not entirely consistent with Figure 7 showing the largest mean between-limb difference in patients after PNS and CNS injury or surgery. A simple explanation is provided by the fact that in this type of injury, the affected part of the body and therefore the affected limb is relatively easy to determine and therefore the between-limb difference can be more striking. The decreasing trend of step time asymmetry for all indicator groups is also confirmed in Figure 8, which enables comparison of the symmetry index data distribution. Almost 80% of patients noticed an improvement in step time symmetry during the treatment program, which leaves only eight patients without a positive change in step time asymmetry (Figure 9).
Figure 7: Average step time values for affected (if possible to determine) or right limb displayed against unaffected or left limb across individual indication groups. A decreasing trend in between-limb difference is noticeable when comparing values measured during the first (before) and last (after) BWST sessions.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 8: Visualization of the distribution and evolution of step time symmetry index data using a box plot graph. Before values represent data obtained during the first BWST session, after values during the last BWST session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 9: Visualization of the progression of step time asymmetry in individual patients using a scatter plot. The dot of the corresponding color represents the patient from the given indication group and the central black line represents the threshold determining the degree of improvement/deterioration during the therapy course. While dots placed below the line express patients who experienced improvement, dots above the line point to those who, on the contrary, noticed deterioration.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
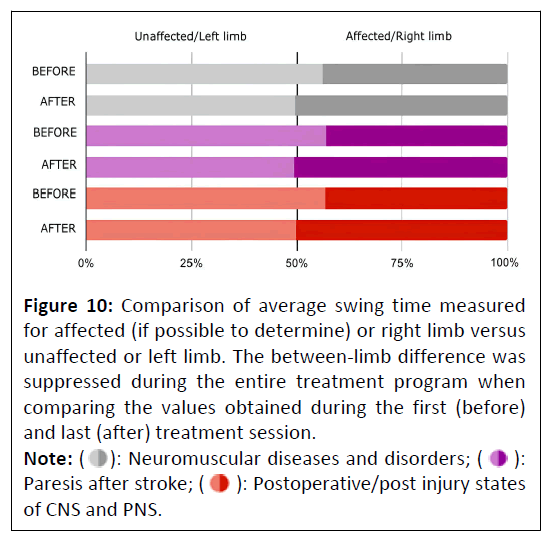
Swing time
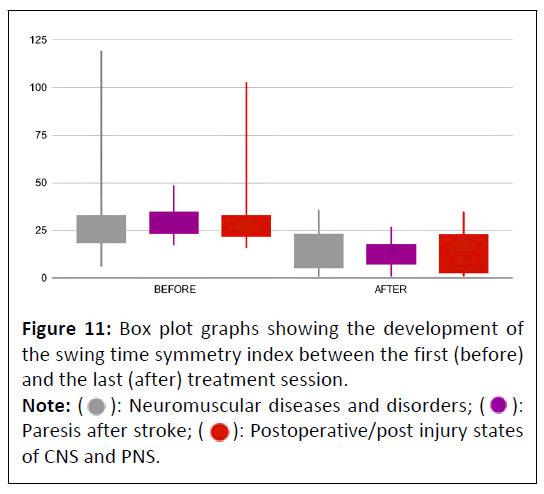
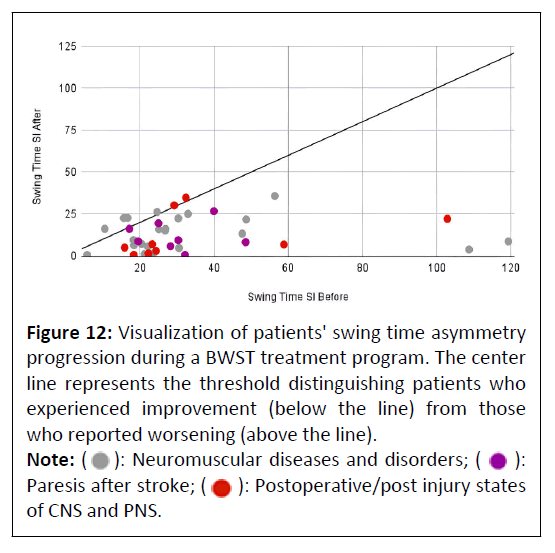
Swing time asymmetry improved statistically significantly in patients of all indication groups by an average of 62% (Table 2). This trend is confirmed by the swing time ratio of both limbs shown in Figure 10 and the box plot graph visualizing the distribution of the swing time symmetry index in Figure 11. Out of the total number of 39 patients, only 6 remained without improvement, which means that almost 85% of patients experienced an improvement in swing time asymmetry Figure 12. Interestingly, positive progress was reported for all poststroke survivors who completed the entire treatment program.
Figure 10: Comparison of average swing time measured for affected (if possible to determine) or right limb versus unaffected or left limb. The between-limb difference was suppressed during the entire treatment program when comparing the values obtained during the first (before) and last (after) treatment session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 11: Box plot graphs showing the development of the swing time symmetry index between the first (before) and the last (after) treatment session. Box plot graphs showing the development of the swing time symmetry index between the first (before) and the last (after) treatment session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 12: Visualization of patients' swing time asymmetry progression during a BWST treatment program. The center line represents the threshold distinguishing patients who experienced improvement (below the line) from those who reported worsening (above the line).
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
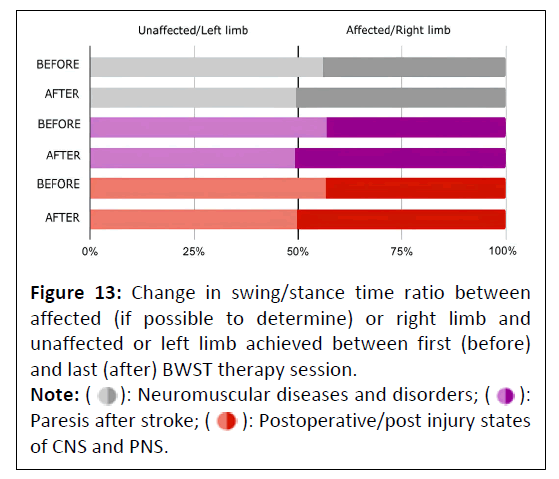
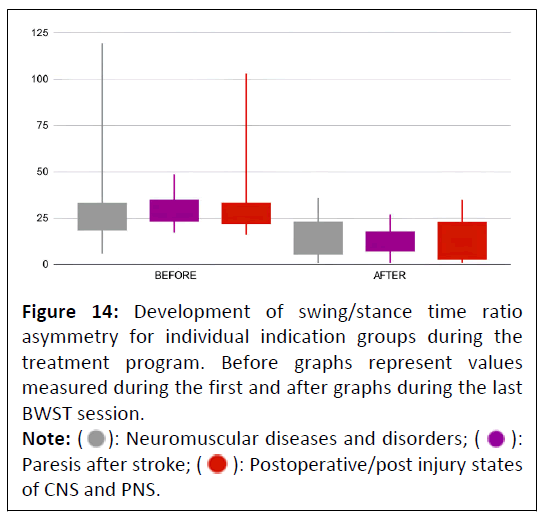
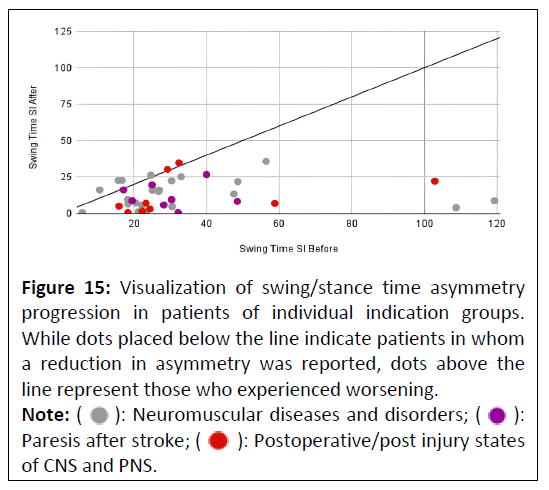
Swing/stance time ratio
The swing/stance time ratio showed a significant asymmetry before the start of the treatment program and recorded the most significant improvement of all the monitored gait parameters. Asymmetry reduction exceeded 68% across the treated cohort of neurological patients. For all indication groups, the improvement reached statistical significance and exceeded 60%. This finding is confirmed by the graphic visualization of the between-limb difference and the evolution of the symmetry index data distribution in Figure 13 and Figure 14, respectively. From Figure 15, showing the improvement achieved in individual patients, it can be seen that only 5 patients experienced deterioration during the treatment program and more than 87% of patients reported a reduction in swing/stance time asymmetry.
Figure 13: Change in swing/stance time ratio between affected (if possible to determine) or right limb and unaffected or left limb achieved between first (before) and last (after) BWST therapy session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 14: Development of swing/stance time ratio asymmetry for individual indication groups during the treatment program. Before graphs represent values measured during the first and after graphs during the last BWST session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 15: Visualization of swing/stance time asymmetry progression in patients of individual indication groups. While dots placed below the line indicate patients in whom a reduction in asymmetry was reported, dots above the line represent those who experienced worsening.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
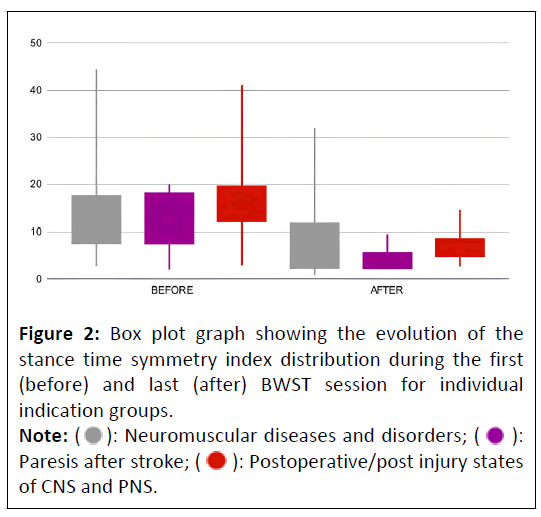
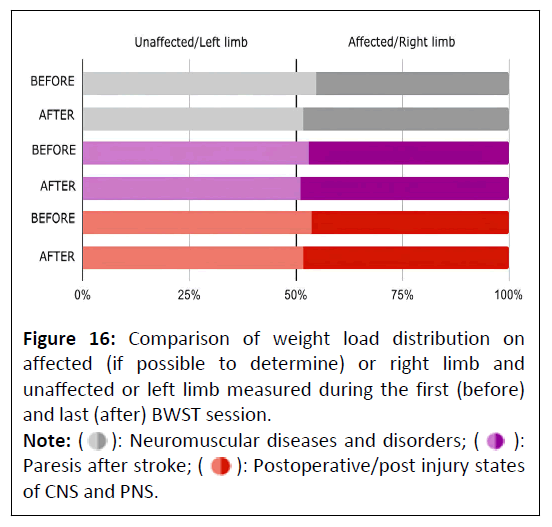
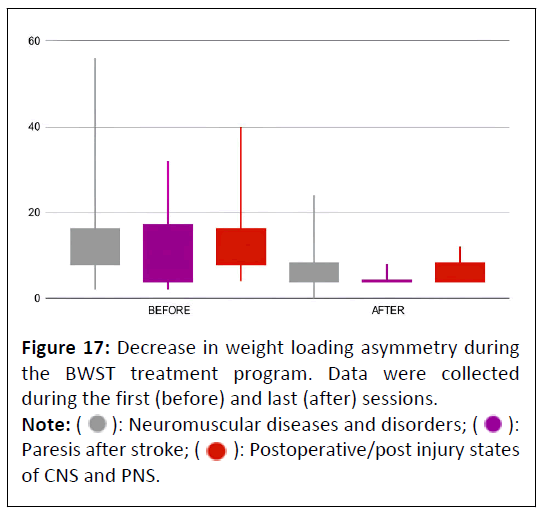
Weight bearing proportion
Asymmetry of weight bearing proportion recorded a statistically significant decrease across the entire treated patient cohort. In post-stroke patients, this decrease did reach a 60% improvement, but the Wilcoxon Sign Rank test did not show statistical significance. For the remaining indication groups, the test confirmed a statistically significant improvement in asymmetry. The decreasing trend of the between-limb loading difference can be observed in Figure 16 and the decrease in weight loading proportion asymmetry for individual indication groups in Figure 17. A total of 10 patients did not notice an improvement in weight loading asymmetry during the BWST sessions 4 experienced deterioration and 6 remained at the same values. Almost 75% of patients showed an improvement in limb load asymmetry (Figure 18).
Figure 16: Comparison of weight load distribution on affected (if possible to determine) or right limb and unaffected or left limb measured during the first (before) and last (after) BWST session.
Note: (  ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; ( ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Figure 18: Graphical representation of patients' progression in weight loading asymmetry achieved during the BWST treatment program. The center line represents patients who noted no change, while the dots above the line depict patients who showed a worsening and the dots below the line those who, on the contrary, noted an improvement in weight loading asymmetry.
Note: ( ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; (  ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.
Discussion
The present study is the first research on an appropriate sample size to demonstrate the effectiveness of BWST therapy in reducing gait asymmetry in neurological patients. These findings are in line with the proven beneficial impact of BWST therapy in patients with multiple sclerosis, spinal cord injury, cerebral palsy, Parkinson's disease and post-stroke survivors [11-21]. The positive effect on gait asymmetry can be further explained by the theory and principle of BWST therapy. This therapy enables exercise with reduced or zero body-weight bearing, allowing neurological patients to begin a gait retraining program despite their common muscle weakness and inability to bear full bodyweight [8,24]. The therapy also prevents the patient from falling, which is one of the key features of walking therapy for neurological patients suffering from impaired balance. In general, it can be assumed that once the gait retraining protocol is designed with regard to suppressing the source of the patient's need for compensatory behavior, gait asymmetry will be significantly reduced. This was confirmed in patients after locomotor system operations, in whom the main cause of asymmetry is the need to compensate for pain and weakness in the impaired segment [6,7]. This may not apply to neurological patients who, in addition to the above-mentioned, also show limitations of a nervous origin. It can be expected that the very possibility of integrating walking exercise into their rehabilitation routine will lead not only to the improvement of gait parameters but also to the reduction of gait asymmetry. The only existing practical evidence of the authenticity of this theory is a smallscale case series study monitoring the progression of gait asymmetry during the BWST program in 4 neurological patients [8]. Now the positive effect has been demonstrated in a largescale study.
General conclusions cannot be drawn from the comparison of results between patients of individual indication groups. First, the sample of patients for the individual groups is not sufficient and second, the between-group difference in the reduction of asymmetry is not significant. Post-stroke patients achieved the greatest average improvement across individual monitored gait parameters, patients with neuromuscular disease or disorder and those recovering from PNS or CNS injury or surgery also experienced an improvement exceeding 50%. This finding can be seen as very promising in the context of neurological rehabilitation BWST therapy can improve walking asymmetry and walking parameters in general, regardless of the origin and nature of the neurological disease.
The main limitation of the present trial is the absence of a control group that would have completed a stand-alone program of conventional rehabilitation. It would enable a better evaluation of the effect of BWST therapy compared to standard methods. A mutual comparison of efficacy for individual neurological indications would require a larger sample size. The present study leaves these goals to future research, which could also focus on other neurological diseases, e.g., multiple sclerosis, Parkinson's disease, radicular syndrome, etc. A detailed analysis of the gait cycle and gait parameters and their asymmetry could provide information about the course of gait recovery in the rehabilitation of various neurological impairments.
A detailed analysis of the gait cycle and gait parameters and their asymmetry could provide information about the course of gait recovery in the rehabilitation of various neurological impairments. The present trial, despite certain shortcomings, brings revolutionary findings about the possibilities of using BWST therapy in a gait retraining program for neurological patients. Complete or partial removal of asymmetry already in the early phase of rehabilitation represents the promise of walking recovery, independence in daily activities and reintegration of patients into society.
Conclusion
The research was the first to prove the effectiveness of BWST therapy in restoring gait symmetry in neurological patients. The average reduction of asymmetry exceeding 58% across the monitored gait parameters in only 6 sessions predisposes BWST therapy to become an integral part of the gait retraining program already in the early phase of rehabilitation. It is very important for patients suffering from a neurological disability to be able to perform effective walking training without the risk of falling. The principle and effectiveness of the BWST method thus represent a unique tool for their independence and return to normal activities.
References
- GBD 2016 Neurology Collaborators (2019) Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(5): 459-480.
[Crossref] [Google Scholar] [Indexed]
- Pearson OR, Busse ME, van Deursen RW, Wiles CM (2004) Quantification of walking mobility in neurological disorders. QJM 97(8): 463-475.
[Crossref] [Google Scholar] [Indexed]
- Wuehr M, Huppert A, Schenkel F, Decker J, Jahn K, et al. (2020) Independent domains of daily mobility in patients with neurological gait disorders. J Neurol 267 (Suppl 1): 292-300.
[Crossref] [Google Scholar] [Indexed]
- Ehrhardt A, Hostettler P, Widmer L, Reuter K, Petersen JA, et al. (2020) Fall-related functional impairments in patients with neurological gait disorder. Sci Rep 10(1): 21120.
[Crossref] [Google Scholar] [Indexed]
- Cabral S (2018). Gait symmetry measures and their relevance to gait retraining. In: Handbook of Human Motion. Springer, Cham.
[Crossref]
- Kubícek M, Brozek T (2023) The effect of body-weight supported treadmill therapy program on the gait asymmetry in patients after lower limb arthroplasty. Adv Tech Biol Med 11: 415.
- KubíÄÂek M, Brožek T (2023) Comparison of the effectiveness of body-weight supported treadmill therapy on the reduction of asymmetry between patients after hip and knee arthroplasty. J Med Phys Appl Sci 8(3): 38.
- Vinarov E (2023) Gait symmetry restoration in patients with common neurological diseases during a body-weight supported treadmill therapy program-a case series study. Med Case Rep 9(10): 328.
- Hassid E, Rose D, Commisarow J, Guttry M, Dobkin BH (1997) Improved gait symmetry in hemiparetic stroke patients induced during body weight-supported treadmill stepping. J Neuro Rehab 11(1): 21-26.
- Combs SA, Dugan EL, Ozimek EN, Curtis AB (2013) Bilateral coordination and gait symmetry after body-weight supported treadmill training for persons with chronic stroke. Clin Biomech 28(4): 448-453.
[Crossref] [Google Scholar] [Indexed]
- Prunerová A, Vinarov E (2023) Increase in metabolic rate and related parameters during an antigravity treadmill exercise program in neurological patients. J Neurodegenero Dis Disord 6(4): 4.
- Pilutti LA, Lelli DA, Paulseth JE, Crome M, Jiang S, et al. (2011) Effects of 12 weeks of supported treadmill training on functional ability and quality of life in progressive multiple sclerosis: a pilot study. Arch Phys Med Rehabil 92(1): 31-36.
[Crossref] [Google Scholar] [Indexed]
- Mansour WT, Atya AM, Aboumousa AM (2013) Improving gait and balance in multiple sclerosis using partial body weight supported treadmill training. Egypt J Neurol Psychiat Neurosurg 50(3): 271-276.
- Escudero FC, Lillo GR, Castro RT, Diaz GV (2019) Effects of body weight-support treadmill training on postural sway and gait independence in patients with chronic spinal cord injury. J Spinal Cord Med 42(1): 57-64.
[Crossref] [Google Scholar] [Indexed]
- Lotfian M, Dadashi F, Rafieenazari Z, Shahroki A, Rasteh M, et al. (2019) The effects of anti-gravity treadmill training on gait characteristics in children with cerebral palsy. Annu Int Conf IEEE Eng Med Biol Soc 2019:5256-5259.
[Crossref] [Google Scholar] [Indexed]
- Atan T, Taskiran OO, Tokcaer AB, Karatas GK, Caliskan AK, et al. (2019) Effects of different percentages of body weight supported treadmill training in Parkinson‘s disease: a double-blind randomized controlled trial. Turk J Med Sci 49(4):999-1007.
[Crossref] [Google Scholar] [Indexed]
- Plummer P, Behrman AL, Duncan PW, Spigel P, Saracino D, et al. (2007) Effects of stroke severity and training duration on locomotor recovery after stroke: a pilot study. Neurorehabil Neural Repair 21(2):137-151
[Crossref] [Google Scholar] [Indexed]
- McCain KJ, Pollo FE, Baum BS, Coleman SC, Baker S, et al. (2008) Locomotor treadmill training with partial body-weight support before overground gait in adults with acute stroke: a pilot study. Arch Phys Med Rehabil 89(4): 684-691.
[Crossref] [Google Scholar] [Indexed]
- Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Nadeau SE, et al. (2011) Body-weight–supported treadmill rehabilitation after stroke. N Engl J Med 364(21): 2026-2036.
[Crossref] [Google Scholar] [Indexed]
- Miller EW, Quinn ME, Seddon PG (2002) Body weight support treadmill and overground ambulation training for two patients with chronic disability secondary to stroke. Phys Ther 82(1): 53-61.
[Crossref] [Google Scholar] [Indexed]
- Lura DJ, Venglar MC, van Duijn AJ, Csavina KR (2019) Body weight supported treadmill vs. overground gait training for acute stroke gait rehabilitation. Int J Rehabil Res 42(3): 270-274.
[Crossref] [Google Scholar] [Indexed]
- Council of Europe (1997) Convention for protection of human rights and dignity of the human being with regard to the application of biology and biomedicine: convention on human rights and biomedicine. Kennedy Institute of Ethics Journal 7:277-290.
- KubíÄÂek M, Brožek T (2023) The relationship between antigravity treadmill therapy settings and gait cycle parameters. J Ortho Sports Med 5(4): 406-415.
- Nayak R (2017) Practical approach to the patient with acute neuromuscular weakness. World J Clin Cases 5(7): 270-279.
[Crossref] [Google Scholar] [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 ): Neuromuscular diseases and disorders; (
): Neuromuscular diseases and disorders; (  ): Paresis after stroke; (
): Paresis after stroke; ( ): Postoperative/post injury states of CNS and PNS.
): Postoperative/post injury states of CNS and PNS.