The Burden of Chronic Liver Disease Patients: Their Clinical and Laboratory Profiles at Jinnah Postgraduate Medical Centre, Karachi
Fahad Khan, Maryam Samad* and Fatima Arif
Sindh Medical College, Dow University of Health Sciences, Karachi, Pakistan
- *Corresponding Author:
- Maryam Samad
Sindh Medical College, Dow University of Health Sciences, Karachi, Pakistan.
Tel: +923433024294
E-mail: maryam.samad@hotmail.com
Received Date: November 29, 2017; Accepted Date: December 08, 2017; Published Date: January 01, 2018
Citation: Khan F, Samad M, Arif F (2018) The Burden of Chronic Liver Disease Patients: Their Clinical and Laboratory Profiles at Jinnah Postgraduate Medical Centre, Karachi. J Med Res Health Educ. Vol. 2 No. 1:3.
Abstract
Objective: To determine the burden of chronic liver disease patients, their clinical and laboratory profiles at Jinnah Postgraduate Medical Centre, Karachi.
Study design: Cross-sectional study.
Methodology: This study was conducted from November 2015 to September 2016 at Medical wards of Jinnah Postgraduate Medical Centre, Karachi. A total of 115 patients who had given informed consent and already had established diagnosis of CLD were included in it. A structured questionnaire was developed, containing all relevant questions and modified with the help of previous studies. Data analysis was done using SPSS version 20. Frequencies, percentages and p-values were reported for various categorical variables. Chi square analyses were conducted to determine association between age groups and presenting complains, duration of disease and Hb levels, cause of CLD and various variables including marital status, gender, Hb levels and sodium levels p-values of <0.05 was taken as statistically significant.
Results: A total of 115 patients were interviewed in which 59.1% patients were male. Demographic data showed majority of patients were in the age group 36-45 years (35.7%), married (91.3%) and non-alcoholics (95.7%). Hepatitis C was found to be the major cause of chronic liver disease (84.3%) and a large group of them (60.9%) had disease duration of >36 months. Majority of them presented with more than one sign and symptoms of decompensation including hematemesis, melena and distention (24.3%). It was shown that patients with longer duration of disease (36 months or more) were associated with mild anemia (Hb level 9.5- 13 gm/dl) (p=0.039). In age group 36-45 years had laboratory reports showing moderate thrombocytopenia (platelets count 50-99,000/μl) (p=0.005). Presented with more than one sign and symptom of decompensation (hematemesis, melena and distention) (p<0.0.5) Large number of people having Hepatitis C as a cause of CLD had lab reports showing mild anemia (9.5-13 gm/dl) (p=0.000) and mild to moderate hyponatremia (120-134 mEq/L) (p=<0.005).
Conclusion: Hence, it is concluded from our study that Hepatitis C is the most common cause of chronic liver disease found in JPMC, Karachi. Majority of patients with chronic liver disease were anemic and hyponatremic.
Keywords
Chronic liver disease; Hepatitis; Cirrohsis
Introduction
Liver diseases are now fifth common cause of death according to UK National Statistics [1] mortality rates of liver diseases are increasing [2] unlike other major diseases. Cirrhosis, the end stage of liver disease slowly occurs for a longer duration, results into gradual damage of the liver [3]. Cirrhosis and hepatocellular carcinoma are mostly caused by infection with hepatitis B and C virus [4]. People with chronic liver disease comprise a major burden on the nation’s economy [3]. In Pakistan, hepatitis is one of the 10 most common diseases [5] and among hepatitis the most common cause of CLD is Hepatitis B and C [6]. In developing countries, including Pakistan, the average age to develop Chronic liver disease is significantly lower than developed countries [2]. Pakistan conveys one of the highest burden of decompensated liver disease in the world [7]. Among Pakistani population Cirrhosis is the leading cause of mortality and recurrent visit in hospitals [7].
The approximate number of HBV and HCV infected individuals worldwide are 370 and 130 million respectively and about 3 million HBV and 4.5 million HCV are co infected with HIV positive [8]. It is anticipated that 15% to 40% of chronic hepatitis B virus infected patient will develop cirrhosis [9]. The carrier rate of HBV in Pakistan is 3-4%, being in an intermediate prevalence zone [10]. In Sindh Province of Pakistan, there are about 1 million and 1.7 million chronic carrier of HBV and HCV respectively [11]. In high prevalence areas of HBV, delta Hepatitis is also found. Approx. 28.3% patients in Karachi with HBV are co-Infected with HDV, while in other areas of Sindh it is about 60.7% [12]. Around 3% of world population is likely to be infected with chronic Hepatitis C virus, with 3-4 million new cases yearly [13]. There is an increasing number of HCV related chronic liver disease in Pakistan [2]. About 10 million people in Pakistan are supposed to be infected with Hepatitis C virus [5]. According to WHO, Pakistan stood on 2nd after Egypt, in prevalence of HCV [14]. According to current data, about 60%- 70% of patient with chronic liver disease and about 50% of with hepatocellular carcinoma in Pakistan are likely to be positive for anti-Hepatitis C virus [15-18]. In Sindh Province of Pakistan, there are about 1 million and 1.7 million chronic carrier of HBV and HCV respectively [11].
The two major causes of hepatitis transmission in Pakistan are blood transfusion and reusable glass syringes for parenteral therapy. Reason for these two can be the scarcity of resources, illtrained staff, ineffective execution of policies, improper screening of blood for hepatitis [19]. Additional risk factors are used of non -sterile gloves, ear piercing material and shaving blades etc. [4]. The commonest complication of End stage liver disease is Esophageal Varices with Portal hypertension, while ascites which was reported in 59% of patients is another one [20,21].
In Pakistan, 24% of patients of DCLD died because of Spontaneous Bacterial Peritonitis. Worldwide, Liver cancer is the sixth most common cancer, It can affects 12/100,000 males and 4/100,000 females in Pakistan, mostly present in fourth and fifth decade of life [22].
Methodology
Setting: The targeted population was patients admitted with the diagnosis of CLD to Medical ward 6 and 7 (M6, M7) at Jinnah Postgraduate Medical Center, Karachi.
Duration: November 2015 to September 2016.
Study design: Cross-sectional study.
Sampling size: The sample size has been calculated using Rao software calculator for sample size determination, which came out to be 115.
Sample selection
Inclusion criteria:
• Those patients giving informed consent.
• Those who already had the established diagnosis of CLD on the basis of history, physical examination (presence of ascites, varices, splenomegaly), laboratory findings (decreased serum albumin, increased prothrombin time, altered liver function tests), and ultrasound findings (portal hypertension, splenomegaly, varices, ascites), presenting to the hospital with signs and symptoms of decompensation of CLD.
• Those having chronic liver disease due to chronic hepatitis and alcoholism.
Exclusion criteria: Patients having age less than 15.
Study variables
Dependent variables: Cause of disease, duration of disease, presenting complains, alcohol intake, laboratory findings (Hb, platelets, TLC count and sodium levels).
Independent variables: Age groups, sex, marital status, residence, occupation, education, family history, comorbidities.
Data collection procedure: A total of 115 Patients participated after having informed consent using a structured questionnaire. A pilot study was conducted to assess the validity of questionnaire. The questionnaire was developed, containing all relevant questions and modified with the help of previous studies. Patients were assured of confidentiality. He/she was assured that no information regarding the interviews and test results will be shared to any one and that this information will be used only for research purpose. They were assured that the identity will not be disclosed at any point in time. Questionnaires have given an identification number.
Structured questionnaire: A structured questionnaire that included all relevant questions of objectives of the study was developed and adapted from previous studies.
Scales included:
• Range of hemoglobin greater than 13 gm/dl was considered normal, 9.5 gm/dl-13 gm/dl mild anemic, 8 gm/dl-9.5 gm/dl moderate anemic and hemoglobin level of less than 8 gm/dl considered as severe anemia [23].
• For total leucocytes count, 4-11 × 109/L was taken normal, less than 4 × 109 was considered leucopenia while count of greater than 11 × 109 was labelled leucocytosis [24].
• For platelets count, severe thrombocytopenia was (10- 49,000/μl), moderate thrombocytopenia (50-99,000/μl), mild thrombocytopenia (100-150,00/μl), normal platelet count (150-350,00/μl) and greater than 350,000/μl was taken as thrombocytosis [25].
• Normal sodium level was taken as 135-145 mEq/L, mild hyponatremia 130-135 mEq/L, moderate hyponatermia 120-129 mEq/L and sever hyponaterima as lesser than 120 mEq/L [26].
Data analysis plan: Data analysis was done using software of SPSS version 20. Frequency counts and percentages were used to describe demographic data and close ended questions (alcohol intake, family history of CLD, comorbidities, cause of disease, duration of disease, presenting complains, laboratory findings including Hb level, platelets and TLCs and sodium levels). Chi square analyses were conducted to determine association between age groups and presenting complains, duration of disease and Hb levels, cause of CLD and various variables including marital status, gender, Hb levels and sodium levels. P value of <0.05 was taken as statistically significant with confidence interval of 95%.
Results
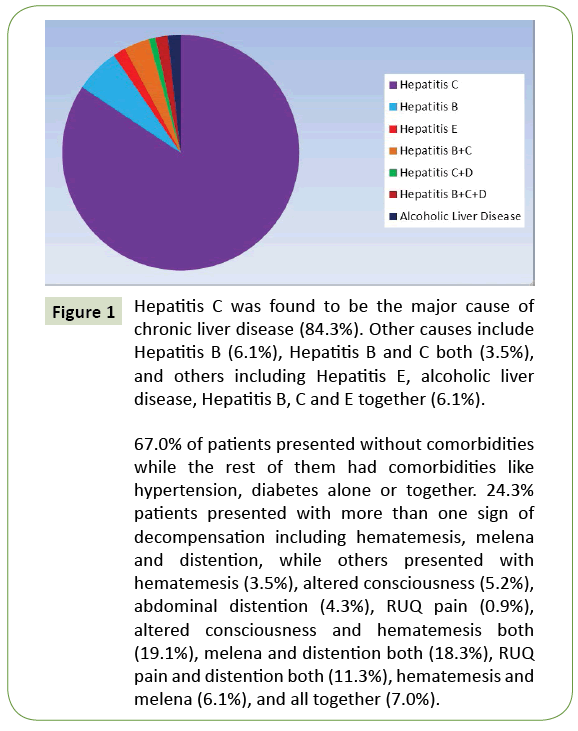
Results of the present study are illustrated in Figure 1 and Tables 1-5.
| Frequency (n) | Percentage (%) | Frequency (n) | Percentage (%) | ||
|---|---|---|---|---|---|
| Gender Male Female |
68 47 |
59.1 40.9 |
Alcohol Intake Yes No |
5 110 |
4.3 95.7 |
| Marital Status Married Unmarried |
100 10 |
91.3 8.7 |
Occupation Housewife Unemployed/retired Labors Services/Job Police Driver Farmer Shopkeeper Hawker Student |
43 29 15 06 05 05 04 04 02 02 |
37.4 25.2 13.0 5.2 4.3 4.3 3.5 3.5 1.7 1.7 |
| Age(49.46) (yrs.) 16-25 26-35 36-45 46-55 56-65 66-75 76-100 |
04 07 41 31 25 06 01 |
3.5 6.1 35.7 27 21.7 5.2 0.9 |
|||
| Residence Karachi Others |
96 19 |
83.5 16.5 |
Education Nil Pre Primary Primary Middle Secondary High School Graduate |
48 14 23 08 18 02 02 |
41.7 12.2 20.0 7.0 15.7 1.7 1.7 |
| FamilyHistory of CLD Yes No |
26 89 |
22.6 77.4 |
|||
| Total | 115 | 100 | Total | 115 | 100 |
Table 1: Socio-demographic factors: a total number of 115 patients were interviewed out of which 59.1% were males and 40.9% were females. Demographic data showed that 35.7% of patients were from age group 36-45 years and only 3.5% from age groups 16-25 years with mean age of 49.46 years. Majority (91.3%) of them was married and 83.5% were residents of Karachi. Greater number of patients was non alcoholics in this study (95.7%). Large number of subjects were housewives (37.4%) and 41.7% patients were illiterate. 77.4% patients denied of any family history of CLD.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| Hemoglobin Ranges | ||
| Severe anemia <8 gm/dl | 30 | 26.1 |
| Moderate anemia 8-9.5 gm/dl | 30 | 26.1 |
| Mild anemia 9.5-13 gm/dl | 49 | 42.6 |
| Normal>13 | 6 | 5.2 |
| Platelets Ranges | ||
| Severe thrombocytopenia (10-49,000/μl) | 12 | 10.4 |
| Moderate thrombocytopenia (50-99,000/μl) | 42 | 36.5 |
| Mild thrombocytopenia (100-150,000/μl) | 30 | 26.1 |
| Normal (150-350,000/μl) | 29 | 25.2 |
| Thrombocytosis (>350,000/μl) | 2 | 1.7 |
| TLC range | ||
| Leucopenia (<4 × 109) | 20 | 17.4 |
| Normal (4-11 × 109) | 71 | 61.7 |
| Leukocytosis(>11 × 109) | 24 | 20.9 |
| Ranges for Sodium | ||
| Severe hyponatremia (>120 mEq/L) | 2 | 1.7 |
| Mild hyponatremia (130-134 mEq/L) | 43 | 37.4 |
| Moderate hyponatremia (120-129 mEq/L) | 44 | 38.3 |
| Normal sodium(135-145 mEq/L) | 26 | 22.6 |
| Total | 115 | 100 |
Table 2: Laboratory profile of patients with CLD: analysis of clinical information which reveals that 42.6% individuals were mildly anemic (Hb in range of 9.5-13 gm/dl), 26.1% patients had severe anemia (8 gm/dl) and similar percentage of patients had moderate anemia (8-9.5 gm/dl). 36.5% patient had moderate thrombocytopenia (platelets count 50-90,000/μl) and 20.9% patients showed leukocytosis (TLC>11 × 109) and 17.4% had leukopenia (TLC<4 × 109). Mild hyponatremia (130-134 mEq/L) was present in 38.3% patients and moderate hyponatremia (120-129 mEq/L) was present in 37.4% patients.
| Duration of disease | Total | p-value | |||||
|---|---|---|---|---|---|---|---|
| <3 month | <6 month | <12 months | <36 months | 36 months or more | |||
| Ranges of Hb Severe anemia<8gm/dl Moderate anemia 8-9.5gm/dl Mild anemia 9.5-13gm/dl Normal>13 |
3 2 8 0 |
7 6 9 0 |
1 1 7 0 |
11 5 6 4 |
8 16 19 2 |
30 30 49 6 |
0.039 |
| Total | 13 | 22 | 9 | 26 | 45 | 115 | |
Table 3: Chi-Square Analyses of Duration of CLD with ranges of hemoglobin: patients with longer duration of disease (36 months or more) were associated with mild anemia (Hb level 9.5-13 gm/dl). Majority of patients had disease duration of 36 months or more from the time of diagnosis (60.9%).
| Age groups (yrs.) | Total | p-values | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 16-25 | 26-35 | 36-45 | 46-55 | 56-65 | 66-75 | 75-100 | |||
| Presenting Complains Hematemesis |
1 | 1 | 2 | 0 | 0 | 0 | 0 | 4 | 0.000 |
| RUQ pain | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
| Abdominal Distention | 0 | 0 | 1 | 1 | 2 | 1 | 0 | 5 | |
| ALOC | 0 | 0 | 3 | 1 | 1 | 1 | 0 | 6 | |
| ALOC and Hematemesis | 1 | 2 | 7 | 7 | 4 | 1 | 0 | 22 | |
| Hematemesis, melana | 0 | 0 | 2 | 4 | 1 | 0 | 0 | 7 | |
| Melana and distention | 1 | 1 | 8 | 7 | 3 | 1 | 0 | 21 | |
| RUQ pain and Distention | 0 | 1 | 6 | 2 | 3 | 1 | 0 | 13 | |
| Hematemesis, melana and distention | 1 | 2 | 10 | 7 | 8 | 0 | 0 | 28 | |
| Hematemesis, melana, RUQ pain, distention and ALOC | 0 | 0 | 2 | 2 | 3 | 1 | 0 | 8 | |
| Platelets Ranges severe thrombocytopenia (10-49,000/μl) |
0 | 2 | 7 | 3 | 0 | 0 | 0 | 12 | 0.005 |
| Moderate thrombocytopenia (50-99,000/μl) |
3 | 1 | 19 | 9 | 8 | 2 | 0 | 42 | |
| Mild thrombocytopenia (100-150,000/μl) |
0 | 4 | 5 | 9 | 8 | 4 | 0 | 30 | |
| Normal (150-350,000/μl) |
0 | 0 | 9 | 10 | 9 | 0 | 1 | 29 | |
| Thrombocytosis (>350,000/μl) |
1 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | |
Table 4: Chi-Square Analyses of age groups with different variables: large number of patients with in age group 36-45 years presented with more than one sign and symptom of decompensation (hematemesis, melena and distention) (p=<0.005) and had laboratory reports showing moderate thrombocytopenia (platelets count 50-99,000/μl) (p=0.005).
| Causes of CLD | Total | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HepB | Hep C | Hep E | Hep B+C |
Hep C+D |
Hep B+C+D |
Alcoholic Liver Disease |
|||
| Marital status Single Married |
3 4 |
6 91 |
1 1 |
0 4 |
0 1 |
0 2 |
0 2 |
10 105 |
0.013 |
| Hemoglobin ranges Severe anemia <8gm/dl Moderate anemia 8-9.5gm/dl Mild anemia 9.5-13gm/dl Normal >13 |
3 1 3 0 |
24 26 43 4 |
1 0 1 0 |
2 2 0 0 |
0 1 0 0 |
0 0 2 0 |
0 0 0 2 |
30 30 49 6 |
0.000 |
| Ranges for sodium Severe hyponatremia(>120mEq/L) Moderate hyponatremia (120-129mEq/L) Mildhyponatremia (130-134mEq/L) Normal sodium(135-145mEq/L) |
0 6 0 1 |
1 35 38 23 |
0 1 0 1 |
0 0 3 1 |
0 1 0 0 |
0 0 2 0 |
1 0 1 0 |
2 43 44 26 |
0.000 |
Table 5: Chi-Square Analyses of causes of CLD with different variables majority of married patients were suffering from Hepatitis C when compared with unmarried patients (p=0.013). Large share of female patients contributed to hepatitis C were housewives (p=0.015) and greater number of people having Hepatitis C as a cause of CLD had lab reports showing mild anemia (9.5-13 gm/dl) (p=0.000) and mild to moderate hyponatremia (120- 134 mEq/L) (p=<0.05).
Figure 1: Hepatitis C was found to be the major cause of chronic liver disease (84.3%). Other causes include Hepatitis B (6.1%), Hepatitis B and C both (3.5%), and others including Hepatitis E, alcoholic liver disease, Hepatitis B, C and E together (6.1%).
67.0% of patients presented without comorbidities while the rest of them had comorbidities like hypertension, diabetes alone or together. 24.3% patients presented with more than one sign of decompensation including hematemesis, melena and distention, while others presented with hematemesis (3.5%), altered consciousness (5.2%), abdominal distention (4.3%), RUQ pain (0.9%), altered consciousness and hematemesis both (19.1%), melena and distention both (18.3%), RUQ pain and distention both (11.3%), hematemesis and melena (6.1%), and all together (7.0%).
Discussion
Chronic liver disease is characterized by gradual destruction of liver parenchyma leading to fibrosis. It is caused by variety of different factor such as viral hepatitis, excessive alcoholism, genetic, autoimmune, NAFLD/NASH. It is one of the most leading causes of morbidity in developing and developed parts of the world.
In our study we have observed that the most common cause for chronic liver disease is Hepatitis C followed by Hepatitis B. which is consistent with the study done in civil hospital Karachi but in western word alcoholism is the most common cause of cirrhosis succeeded by hepatitis [27,28].
The mean age of patient presented in our study was 49.46 years, similar results were observed in study conducted in Balochistan [29]. While majority of individuals presented with chronic liver disease were in 3rd and 4th decade of life, which is also stated in previous study [30].
Greater no of individual in our study were presented with more than one sign and symptom of decompensation, similar results were stated in the study conducted at civil hospital Karachi. The most common sign of decompensation was upper GI bleeding (hematemesis or melena), which is consistent with the results found in study conducted in Punjab [31]. On contrary, ascites was found to be most common sign of cirrhosis in another study [20].
Electrolyte imbalances were observed in our study. Most of the subjects (77.4%) were hyponatremic while about 25.2% of patients were hypokalemic. Hyponatremia and hypokalemia were also found in the study conducted on patient of cirrhosis [30].
Hyponatremia is a major electrolyte disturbed in advance Cirrhosis and is associated with worsened clinical outcomes [32]. It can be classified as hypovolemic hyponatremia or hypervolemic hyponatremia depending upon overly use of diuretics or GI loss or activation of renin angiotensin system respectively [32,33].
As electrolytes can be majorly imbalanced with advance cirrhosis, caution must be paid while infusing diuretics and electrolytes must be routinely checked [23]. Hematological abnormalities are often associated with cirrhosis [30,34].
Over all, in our study, we have observed low hemoglobin level in about 109/115 (94.8%) subjects and decrease platelet count 84/115 (73%) of individual similar results of low hemoglobin and platelet counts were found in the study conducted in Jamshoro, Hyderabad [35].
While 24/115 (20.9%) in our study had increased total leukocyte count. The cause of anemia could be upper and lower GI bleeding due to portal hypertension or due to defective synthesis of coagulation factors by injured hepatocyte.
Numerous factor leads to development of thrombocytopenia, such as sequestration of platelet in spleen, suppression of platelet production in bone marrow due to chronic Hepatitis C virus or treatment with interferon therapy [25].
Due to limitation of resources, financial and time constraint, data was collected from one tertiary care hospital of Karachi. Risk factors were not evaluated. Patients were not assessed pre and post treatment.
Conclusion
Hence, it is concluded that Hepatitis C is the most common cause of chronic liver disease found in JPMC, Karachi. Most of the patients with CLD had presented with more than one sign of decompensations, mostly with upper GI Bleed. Majority of the patients with longer duration of disease were anemic and Greater number of patient with CLD were mild to moderately hyponatremic.
Declarations
Ethics approval and consent to participate
We took approval from the administration before enrolling the participants of study, every management staff operating in the study area was informed about the nature and objectives of the research. Participants were informed about study objective and procedures and informed consent was taken from the participant. The interviews were conducted in privacy and no sharing of information was done. Counseling was done after interview and no direct benefit to participant, study participants was free to withdraw from the study at any time.
Consent to publish
The aims and objectives of this study were explained to the participants properly and they were also told that we will use the information when the study will be published.
Availability of data and materials
Not applicable because we didn’t get the proper consent to submit the data and provide our data sets. Also we do not feel there is any need of doing it.
Competing interests
The Authors declare that there is no conflict of interest.
Funding
There are no funding sources for this study.
Author’s contributions
This article was prepared in collaboration between all authors. Authors Maryam Samad and Fatima Arif did conception and design, acquisition, analysis and interpretation of data and drafted the article. Author Fahad Khan did critical revision of the article and gave final approval of the version to be published. All authors read and approved the final manuscript.
Acknowledgements
There are no acknowledgements required.
References
- UKNationalStatistics.
- WilliamsR(2006)Globalchallengesinliverdisease.Hepatology44:521-526.
- RohraDK,KhowajaAA(2008)ModesofpresentationandreasonsofhospitalizationforpatientswithdecompensatedchronicliverdiseaseatCivilHospitalKarachi.JournalofDowUniversityofHealthSciences2:50-54.
- JafriW,JafriN,YakoobJ,IslamM,TirmiziSF,etal.(2006)HepatitisBandC:prevalenceandriskfactorsassociatedwithseropositivityamongchildreninKarachi,Pakistan.BMCInfectiousDiseases6:101.
- HamidS,UmarM,AlamA,SiddiquiA,QureshiH,etal.(2004)PSGconsensusstatementonmanagementofhepatitisCvirusinfection-2003.TheJournalofthePakistanMedicalAssociation54:146.
- HanifM,RazaJ,QureshiH,IssaniZ(2004)Etiologyofchronicliverdiseaseinchildren.PakistanMedicalAssociation54:119-122.
- MemonMS,ZakiM(2013)BurdenofchronicliverdiseaseandlivertransplantationinSindh.JLUMHS12:1.
- AlterMJ(2006)EpidemiologyofviralhepatitisandHIVco-infection.JournalofHepatology44:S6-S9.
- MaddreyWC(2000)HepatitisB:animportantpublichealthissue.JournalofMedicalVirology61:362-366.
- AndréF(2000)HepatitisBepidemiologyinAsia,theMiddleEastandAfrica.Vaccine18:S20-S22.
- MalikN,ButtT,MansoorN,KhanTG,AkbarMS,etal.(2008)PercentageofhepatitisBandCamongyoungadultmalesfrominteriorSindh.PakArmedForcesMedJ58:260-266.
- SeetlaniNK,AbbasZ,RazaS,YakoobJ,JafriW(2009)PrevalenceofHepatitisDinHBsAgpositivepatientsvisitingliverclinics.JournalofPakistanMedicalAssociation59:434.
- WorldHealthOrganization(2000) HepatitisC.FactsheetNo.164.RevisedOct2000.
- PrevalenceofHepatitisBandCinGeneralPopulationofPakistanByPakistanMedicalResearchCouncil,IslamabadintheYear2007-08.
- KhanAA,HaiderZ,ShafqatF(2002)SeroMarkersofHepatitisBandCinpatientswithcirrhosis.JournaloftheCollegeofPhysiciansandSurgeonsPakistan12:105-107.
- UmarM,KhaarHB,AnwarF,ZahidM(2000)ThemanagementofacutevaricealbleedingbyOctreotide.JRawalMedColl4:14-16.
- HamidS,TabbasumS,JafriW(1999)HepatitisChasreplacedHepatitisBasthemajorcauseofchronicliverdiseaseinPakistan.Hepatology30:s212.
- ChohanAR,UmarM,KhaarB,KhurramM,ZahidM,etal.(2001)Demographicfeaturesofhepatocellularcarcinoma.Astudyof30cases.JRawalMedColl5:81-83.
- DevrajaniBR,SoomroAA,AttraKM,QureshiGA(2009)Varicealbleedinganditsdependenceonportalveinsizeinlivercirrhoticpatients.AdvancesinMedicalandDentalSciences1:60-65.
- AlmaniSA,MemonAS,MemonAI,ShahI,RahpotoQ,etal.(2008)Cirrhosisofliver:Etiologicalfactors,complicationsandprognosis.JLiaquatUniMedHealthSci7:61.
- RamN,QadriHU,ShahA,ShaikhAS(2012)FrequencyofSpontaneousBacterialPeritonitisinPatientswithHepaticEncephalopathy.MedicalChannel18:36-38.
- HepatocellularCarcinomainRelationAnti-HCVPositivePatients.PosterPresentationatthe23rdConferenceoftheAsianPacificAssociationfortheStudyoftheLiver:Abstract.A-535-0028-01375.
- TheNewYorkTimes(2018)Availablefrom:https://www.nytimes.com/health/guides/disease/anemia/diagnosis.htmlAccessedon:22February,2018.
- Medscape(2015)LeukocyteCount(WBC)-September2015,Availablefrom:https://emedicine.medscape.com/article/2054452-overviewAccessedon:September15,2015.
- AfdhalN,McHutchisonJ,BrownR,JacobsonI,MannsM,etal.(2008)Thrombocytopeniaassociatedwithchronicliverdisease.JHepatol48:1000-1007.
- Medscape(2018)Hyponatremia-January2018,Availablefrom:https://emedicine.medscape.com/article/242166-overviewAccessedon:January06,2018.
- NaheedT(1998)Antigenemiainchronicliverdisease.Specialist(PakJMedSci)14:303-308.
- HussainI,NasrullahM,ShahAA(1998)PrevalenceofhepatitisBandCviralinfectionsinlivercirrhosisinPakistan.PakJGastroenterol12:7-11.
- DurraniAB(2000)ThespectrumofchronicliverdiseaseinBalochistan.JCollPhysiciansSurgPak11:95-97.
- AlamI,RazaullahHI,HumayunM,TaqweemMA,NisarM(2005)Spectrumofprecipitatingfactorsofhepaticencephalopathyinlivercirrhosis.PakJMedRes44:96-100.
- SheikhA,AhmedSI,NaseemullahM(2001)Aetiologyofhepaticencephalopathyandimportanceofuppergastrointestinalbleedingandinfectionsasprecipitatingfactors.JRawalMedColl5:10-12.
- YuC,SharmaN,SaabS(2013)Hyponatremia:clinicalassociations,prognosis,andtreatmentincirrhosis.Experimentalandclinicaltransplantation.OfficialJournaloftheMiddleEastSocietyforOrganTransplantation11:3-11.
- AngeliP,WongF,WatsonH,GinèsP(2006)Hyponatremiaincirrhosis:resultsofapatientpopulationsurvey.Hepatology44:1535-1542.
- Gonzalez-CasasR,JonesEA,Moreno-OteroR(2009)Spectrumofanemiaassociatedwithchronicliverdisease.WorldJGastroenterol15:4653-4658.
- DevrajaniBR,ShahSZ,DevrajaniT,KumarD(2009)PrecipitatingfactorsofhepaticencephalopathyatatertiarycarehospitalJamshoro,Hyderabad.TheJournalofthePakistanMedicalAssociation59:683.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences