ISSN : ISSN No. 2471-9781
Journal of Hospital & Medical Management
The Benefits and Effects of Using Marijuana as a Pain Agent to Treat Opioid Addiction
Howard University Hospital, Washington DC, USA
- *Corresponding Author:
- La France B
Anesthesiology Department
Howard University Hospital, 2041 Georgia Avenue
Washington DC, 20060, USA
Tel: (202) 865- 6714
E-mail: bemore1576@gmail.com
Received date: August 24, 2018; Accepted date: October 06, 2018; Published date: October 09, 2018
Citation: Griffith C, La France B (2018) The Benefits and Effects of Using Marijuana as a Pain Agent to Treat Opioid Addiction. J Hosp Med Manage Vol.4 No.3:7
DOI: 10.4172/2471-9781.100051
Abstract
A shocking population of Americans and Canadians succumb to opioid addiction daily. In response to this, various interventions including pharmaceutical therapies have been put in place to address overdose prevention. However, the adoption of pharmaceutical interventions such as the use of buprenorphine, α2-adrenergic agonists, and antiemetic’s pose the risk of harmful drug interaction and overdose. As such, Cannabis sativa (marijuana) is considered an adjunct therapy for opioid addiction due to its safety and efficacy. The present paper explores the benefits and potential effects of marijuana as a therapeutic option in treating opioid addiction. The study conducted a systematic literature review of published journals in America and Canada related to the use of marijuana for management of opioid addiction. Medical databases such as CINAHL, Cochrane, and PubMed were used to identify peer-reviewed articles between 2014 and 2018. The PRISMA flow diagram was used to identify and document the number of articles eligible for the research. 1,608 records were identified out of which 30 full-text articles were screened for eligibility. Out of the 30 items, 10 full-text articles met the inclusion criteria. These reported the safety and efficacy of the use of medical cannabis in managing opioid addiction. In essence, marijuana suppresses cravings induced by opiates and controls opioid withdrawal syndromes. However, cannabis may result in non-serious effects such as disorientation, lethargy, hallucinations, and confusion. The current literature review concludes that the use of marijuana for opioid addiction is safe and effective. Certainly, insufficient literature is available to establish the benefits and harms of medical cannabis as a therapy option for opioid addiction.
Keywords
Opioid addiction; Cannabis; Analgesics; Δ-9 tetrahydrocannabinol; Cannabidiol
Introduction
Background
The use of opioids dramatically increased during the 1990s following relaxed regulations on the need for the drug to function in pain management. However, as the indication of opiates gained traction, more parallel use of the drug especially for addiction raised more concerns about its benefits compared to the harm it poses [1]. The flop in the earlier realization of its peril thus leads to increased opioids related deaths. In the United States, prescription opioid-related overdoses stand as the current leading incidences of preventable deaths. On average, 91 Americans are killed every day due to opioid-related drug overdoses. Canada, a second country after the US, records an increased pattern of the use and abuse of opioids. For instance, Canada is reported to have had about 2,400 incidences of opioid-related deaths in 2016 alone [2]. As such, following these incidences, it is apparent that the use of prescription opioids are associated with addiction that pits more harm on the use of the drug for pain management compared to its benefits. Besides, a growing toll related to the opioid dependence in the United States, Canada, and the world as a whole necessitates a diversity of novel harm-reduction interventions.
Evidence from research indicates that conventional pharmaceutical intervention on opioid addiction through the use of buprenorphine and methadone pose the risk of harmful drug interaction and related overdose [3]. Equally, other drugs used to manage opioid withdrawal syndrome such as benzodiazepines, α2-adrenergic agonists, and antiemetics do not treat the underlying medical condition [4]. Instead, the intervention increases problems including addiction and burden to a number of medications used, which limits longterm treatment options for these patients. As such, the current research affirms the effectiveness of Cannabis sativa (marijuana) as a suitable therapeutic option for the management of opioidbased addictions and treating chronic pain. Marijuana has for long been used as a recreational drug but not readily indicated for medicinal purposes [5]. Even though clinical trials indicate promising results on the use of the drug for pain management, it is not currently approved for acute or chronic pain.
Conventional research on cannabis affirms that the drug can be effective in opioid-induced pain relief and treatment of opioid addiction. The use of marijuana reduces cravings for heroin addicts while at the same time manages the withdrawal symptoms associated with the addiction to opiates [6]. However, despite these benefits, the use of cannabis might pose adverse effects and related risk of addiction. It is therefore essential to conduct expanded research to assess the potential benefits and risk profile associated with the use of marijuana for treatment of opioid addiction.
Objectives
• To establish the benefits and risks associated with marijuana in treating opioid addictions.
• To find out the most abundant compound in marijuana vital for the management of opioid-induced pain.
• To determine the relationship between marijuana and opioids in pain management.
Materials and Methods
Design of the study
In order to address the objectives of this research, the study conducted a systematic literature review of published articles in the United States of America and Canada. Medical databases were searched to identify peer-reviewed journal articles published between the years 2014 and 2018. The eligible study articles were systematic reviews and addressed the use of medical cannabis for the treatment of opioid addiction [1]. The study reviews met the inclusion criteria if they were systematic reviews on the use of MC for opioid addiction treatment, peerreviewed articles, and published in English. On the other hand, journal articles were excluded if they were non-systematic reviews. Nonetheless, the studies incorporated for the research were those based on randomized control trials (RCTs). Besides, controlled (non-randomized) clinical trials (CCTs), and prospective and retrospective comparative cohort research design were used to analyze and compare published comprehensive data on the use of cannabis as an adjunct treatment for opioid addiction.
Materials used
The research used information sources developed from searching medical subject headings (Mesh) and text words related to the use of medical cannabis for treatment of opioid addiction on selected databases. Information sources were explored in medical databases following the PRISMA guideline. Systematic literature reviews were searched on the Cochrane Library, CINHAL, EMBASE, Medline, PubMed, and Google Scholar. So as to identify systematic reviews, the study used search terms combined with appropriate Boolean operators which included the subject heading terms for three key aspects: medical cannabis AND analgesics (opioid OR painkiller) AND addiction (non-medical use OR misuse).
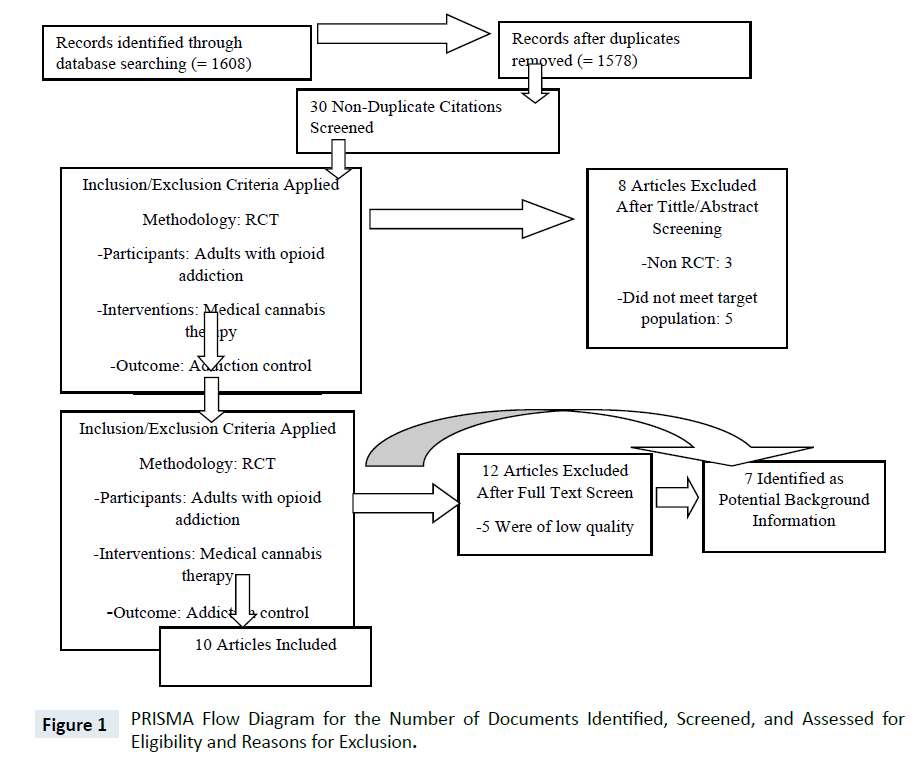
The study selection and screening method used a PRISMA flow diagram as illustrated in the figure below. In the search, totaling to 1608 unique hits, 1578 search articles were removed leading to a screening of 30 full-text journals. Out of these, 8 full-text papers were excluded since they used non-randomized control trials. Out of the 22 remaining articles, 7 were of low quality while 5 were of moderate quality and 10 yielded results of high quality.
The data in each of the studies were summarized as per the following aspects: databases used, journal name, name of the author, year of publication, theme of systematic reviews (opioid misuse and marijuana therapies) and review period [6]. Apparently, the data extraction process included systematic review articles, studied population, and the summary of findings in each study. A narrative approach was used to collect information on medical cannabis intervention for outcome analysis Figure 1.
Results
From the ten articles selected in the systematic reviews, varied results were established. In one study for opioid addicted patients enrolled in a medical cannabis program (MCP), a 21 month of observation yielded a positive outcome. MCP was related to 17.27 odds of ceasing compulsive use of prescription opioids (CI of 1.89 to 157.36, and p=0.012) [7]. Results of the same study indicated 5.12 higher odds associated with reduced prescription opioid dosages on a daily basis (CI of 1.56 to 16.88, p=0.007). Furthermore, the result reported a reduction of 47% points in the daily dosages of opioid use among the experimental group compared to the comparison group (CI -90.68 to -3.59, p =0.034). The participants in the survey reported pain reduction in addition to improvements in activity levels, social life, and overall quality of life. However, few side effects were reported one year after the enrollment of opioid addicts on the MCP (ps<0.001) [7].
In a cross-sectional study of Canada’s national system on medical cannabis administration, the research reported that 63% of the chronic pain patients substituted marijuana as a prescription drug (n=166), while 32% used prescription opioids for therapy (n=80) [2]. However, patients on prescription opioids reported increased incidences of addiction. Research further suggests that patients being managed for opioids addiction reported multiple benefits on the use of medical cannabis. The latter as a prescription medication had less adverse effects (39%, n=68), was safer (27%, n=48), and was better in the management of symptoms (16%, n=28) [2]. The study results showed similarity with the Veteran’s Affairs Canada (VAC) findings on the value of the medical cannabis. According to VAC, prescription marijuana significantly led to a reduction in the prescription of benzodiazepines by 30% and a decrease in the use of opioids by 16% [1].
Retrospective cohort studies established that marijuana indicated in treating opioid use disorder reduced cravings for heroin users. Pilot studies on cannabidiol (CBD), one of the cannabinoids found in the marijuana plant, had the most potent effects in lowering anxiety induced by heroin cues [4]. However, accumulating evidence from preclinical studies in human established that both opioids and cannabinoids regulate pain only that these two drugs had different effects on the brain. Studies on marijuana have found that the drug has a stronger effect on how it communicated sensation between the neurons in the brain [8]. Besides, marijuana yields a significant benefit in relieving inflammation-based chronic pain as opposed to opioid analgesics, which have a strong effect in reducing acute pain [9]. Contrary to cannabinoids, opiate painkillers can quickly lead to addiction. Moreover, marijuana has a broader window of therapeutic benefits because the drug can provide pain relief for opioid addicts without causing a potential overdose.
Discussion
Recent preliminary findings suggest that marijuana could be an effective therapy in the management of opioid addictions. Current studies indicate that medical cannabis significantly leads to a 33% reduction in the use of opioids and opioid-related fatalities. The findings are consistent with the report of the opioids addiction patients enrolled on the MCP [7]. Under this setting, the patients with the opioid use disorder were able to self-manage marijuana therapy and reduce the use of opioids for pain management. Nonetheless, meta-analysis shows that the safety and efficacy of the use of medical cannabis in the treatment of opioid addiction were statistically significant as the patients were able to engage in their own methods of harm reduction [3]. The latter included abstinence from the use of prescription opioids for pain relief.
Cannabis derivatives especially the CBD tends to be nonrewarding and can modulate the perception of anxiety common to patients addicted to opioids. Besides, CBD has no known side effects, and study reports indicate its low lethality [9]. Based on this aspect, medical cannabis can be considered a natural replacement for prescription opioids for pain management. Likewise, published reports in the Trends in Neurosciences reveal that clinical CBD restores the neurobiological damage caused by opioid addictions [6].
According to a study by Samoilov and Browne (2018), scientists have reported two major active chemicals found in the marijuana plant. These include the cannabidiol (CBD) and tetrahydrocannabinol (THC). According to the research studies, CBD impacts the brain without inducing addiction. However, the THC chemical has pain relieving properties but can significantly lead to addiction. Although limited scientific evidence has been conducted to ascertain the medical use of chemicals in cannabis, research indicates that there are more than 400 compounds in marijuana responsible for pain relief [10]. However, legitimate use of marijuana still limits it for management of opioids addiction due to its associated harm. Research studies by Esther & Choo indicate that chronic use of marijuana can lead to impaired memory, reduced ability to learn, and slow processing of information for children before attaining age 16. In adults diagnosed with or without other substancerelated disorders, short-term effects of marijuana have been reported. These include disorientation, drowsiness, dizziness, loss of balance, hallucinations, and confusion [9]. Apparently, most of these reported adverse effects of cannabis tend to be non-serious. Documented evidence has shown that smoked marijuana is relatively safer for adult patients diagnosed with opioid use disorder. The aspect is supported by the premise that smoked Cannabis sativa extracts are well-tolerated and are not associated with the risk of mortality for opioid addicts [6].
Several cannabis-based preparations in addition to smoked products include edible oil in vaporized or capsule form. It, however, remains uncertain on how each of the cannabis-based products influences the health of the patients diagnosed with opioid use disorder. Seemingly, consumption of the medical cannabis leads to euphoria and is associated with altered perception together with decreased anxiety [8]. Moreover, the CBD in marijuana modulates seizures, nausea, and possesses antipsychotic effects. Apparently, medical cannabis acts on the endocannabinoid system in which the endocannabinoid neurotransmitters initiate the signaling of the cannabinoid receptors indicated as 1 and 2 (CB1 and CB2) in the brain. CB1 is a
G-protein-coupled receptor abundantly found in the human brain. The activation of this protein facilitates the dopamine reward pathway, which is mostly associated with substance dependence and addiction. Conversely, the inhibition of the CB1 receptor can significantly decrease the ability of substances such as opiates, ethanol, nicotine, and cocaine to activate the dopamine pathways (Vyas, LeBaron & Gilson, 2018) [4]. Certainly, marijuana contains Δ-9 tetrahydrocannabinol (THC) active compound, and the latter is a partial agonist to the CB1 receptor in the brain. In other words, THC induces effects such as tachycardia, euphoria, and decreased pain response to substance misuse including those implicated with opioids addiction (Boehnke, Litinas & Clauw, 2016) [8].
Conclusion
Opioid epidemic remains a public health concern in the United States of America and Canada. Nonetheless, evidence regarding the efficacy of the use of medical cannabis for managing opioid addiction continues to accrue. However, the ability of marijuana to interfere with opioid addiction biochemistry is intriguing and remains obscure due to limited research on the topic. Besides, the use of cannabis as an alternative to opioids for pain management requires additional empirical research attention to reduce the potential harms of opioid addictions. Even though medical cannabis possesses associated risks, its severity is less when used to treat opioid addiction. Moreover, self-medication using marijuana decreases anxiety for opiate addiction, and potentials harms of opioids are remarkably reduced. Hence, in the long term, the use of marijuana as an adjunct therapy for opioid dependence can decrease opioid-related morbidity and mortality in addition to reducing the overall burden on the health care system.
References
- Rowell II PM (2016) Special Commentary: Advocating the rescheduling of marijuana in US federal and state drug law to permit the use of medical marijuana in the pediatric patient population. J Health Care Finance.
- Samoilov L, Browne CP (2018) The role of medical cannabis in the opioid crisis. Med J 87: 38-41.
- Lucas P, Walsh Z, Crosby K, Callaway R, Belle‐Isle L, et al. (2016) Substituting cannabis for prescription drugs, alcohol and other substances among medical cannabis patients: the impact of contextual factors. Drug Alcohol Rev 35: 326-333.
- Vyas MB, LeBaron VT, Gilson AM (2018) The use of cannabis in response to the opioid crisis: A review of the literature. Nurs Outlook 66: 56-65.
- Powell D, Pacula RL, Jacobson M (2018) Do medical marijuana laws reduce addictions and deaths related to pain killers? J Health Econ58: 29-42.
- Hourani W, Alexander SP (2018) Cannabinoid ligands, receptors and enzymes: Pharmacological tools and therapeutic potential. Brain Neurosci Adv.
- Sexton M, Cuttler C, Finnell JS, Mischley LK (2016) A cross-sectional survey of medical cannabis users: patterns of use and perceived efficacy. Cannabis and Cannabinoid Research 1: 131-138.
- Boehnke KF, Litinas E, Clauw DJ (2016) Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain Res17: 739-744.
- Bradford AC, Bradford WD (2017) Medical marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Aff 36: 945-951.
- Esther K, Choo MD (2016) Opioids Out, Cannabis in Negotiating the Unknowns in Patient Care for Chronic Pain. JAMA 316: 1763-1764.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences