The Anthropological View of Down’s Syndrome Prevalence in Abuja Nigeria (A Retrospective Study)
Donatus AA* and Abubakar I
Department of Anatomical Sciences, Faculty of Basic Medical Sciences, College of Health Sciences University of Abuja, Abuja, Nigeria
- *Corresponding Author:
- Donatus AA
Department of Anatomical Sciences,
Faculty of Basic Medical Sciences,
College of Health Sciences University of Abuja,
Abuja,
Nigeria
Tel: 08053046662
E-mail: drandrewabue@gmail.com
Received Date: July 13, 2021; Accepted Date: July 27, 2021; Published Date: August 03, 2021
Citation: Donatus AA, Abubakar I (2021) The Anthropological View of Down’s Syndrome Prevalence in Abuja Nigeria (A Retrospective Study). J Anat Sci Res Vol.4 No.5:1.
Abstract
Anthropologically, Down syndrome was first described in the medical literature by John Langdon Down in 1866. During this era individuals with cognitive impairment (i.e. mental retardation) were often referred to as idiots and imbeciles and rarely differentiated into subcategories based upon differential diagnoses. Using a hierarchical racial classification system that was popular during his age, John Langdon Down noted the resemblance of facial features among individuals with Down syndrome and individuals of Mongolian descent.
Objective: The main objective of this study is to determine the prevalence of Down's syndrome in University of Abuja Teaching Hospital (UATH) from January 2006 to December 2007.
Results and discussion: The prevalence of Down's syndrome of 1 in 832 (1.20 in 1,000) livebirths in the present study is similar to the prevalence reported from other parts of the world, Compared with the Uganda and Nigeria; that suggested rarity or non-existence of Down's syndrome among Africans many years ago, our results show the prevalence that is about five times higher.
Keywords
Prevalence; Down’s Syndrome; Abuja; Nigeria
Introduction
Anthropologically, Down syndrome was first described in the medical literature by John Langdon Down in 1866. During this era individuals with cognitive impairment (i.e. mental retardation) were often referred to as idiots and imbeciles and rarely differentiated into subcategories based upon differential diagnoses [1,2]. Using a hierarchical racial classification system that was popular during his age, John Langdon Down noted the resemblance of facial features among individuals with Down syndrome and individuals of Mongolian descent [3-6]. Down also noted the characteristic facial appearance and shared phenotypic features of unrelated individuals with Down syndrome in the following: when placed side by side, it is difficult to believe that the specimens compared are not children of the same parents. Based upon these observations Down determined that individuals with Down syndrome differed from other types of individuals with cognitive impairment and labeled these individuals as Mongolian idiots or mongoloids. Although other authors may have described individuals with Down syndrome before Down’s publication in 1866, Down is credited with being the first person to group together individuals with Down syndrome based upon their phenotypic similarities to define a subcategory of individuals with cognitive impairment. The hierarchical racial ladder of Down’s era viewed the races of mankind as being fixed and definite, with Caucasians being superior to all other races and Mongolians being at the bottom of the ladder. Although Down’s Mongolian idiot and mongoloid labels would be viewed as racist today, the use of these terms was a consequence of the prevailing ideas of racial hierarchies from his era. By combining this interpretative framework with his phenotypic observations of individuals with Down syndrome, Down made an argument for the unity of the human species.
Down reasoned that if a disease can break down supposedly fixed racial barriers by producing a Mongolian-like child from non-Mongolian parents, then the racial categories of mankind are likely not fixed at all and quite variable. This was an unpopular opinion at the time of Down’s publication. Interestingly, if Down had not favored this hierarchical racial classification system for understanding differences between individuals with cognitive impairment, it is likely that it would have taken much longer for medical scientists to classify Down syndrome as different from other forms of cognitive impairment [7-10].
Dr. Jerome Lejeune, a French physician, made the discovery that Down syndrome (DS) was the result of a chromosomal abnormality [11]. His research led him to the fat that the cells of people with Down syndrome (mongoloids, at the time) had 47 chromosomes whereas the cells of people without the syndrome only had 46 chromosomes Just a little while after that, it was discovered that chromosome number 21 contained an extra partial or complete chromosome in these so called ‘Mongoloids’ Thus, the term Trisomy 21 was born.
In 1961 a group of prominent geneticists from around the world got the name of this condition changed from Trisomy 21 to Down syndrome after John Langslon Down, The World Health Organization accepted this new name as standard in 1965. Today in the United States, Canada, and most other countries of the world Down syndrome is the accepted term when referring to this genetic disorder. In the United Kingdom, however, it is referred to as Down's syndrome.
Named after John Langdon Down, the first physician to describe the syndrome's common features as a distinct entity, Down syndrome is the most frequent genetic cause of mild to moderate mental retardation and associated medical problems. Three genetic variations can cause Down syndrome, which occurs in one out of 800 live births and in all races and economic groups. Most often, Down syndrome is caused by the presence of an extra chromosome 21 in all cells of the individual (called "trisomy 21"). In a small percentage of cases, the extra chromosome 21 is present in some, but not all cells of the individual (called "mosaic trisomy 21''). In about 3 percent to 4 percent of the cases, individuals have the normal number of chromosomes, but carry portions of material from chromosome 21 on other chromosomes, resulting in the features associated with Down syndrome (called translocation trisomy 21").
A random event during the formation of reproductive cells or during very early development tends to Down syndrome. These events do not appear to be attributable to any behavioral activity of the parents or environmental factors. In almost 9 out of 10 cases, the mother is the source of the extra copy of chromosome 21. As a woman ages, the likelihood that a reproductive cell she ovulates will contain an extra copy of chromosome 21 increases dramatically. A woman younger than age 30 who becomes pregnant has less than a 1 in 1,000 chance of having a baby with Down syndrome, but by age 42, the chance is 1 in 60. However, more than 75 percent of pregnancies that result in Down syndrome occur in women younger than age 40. Several prenatal diagnostic tests are available to detect Down syndrome, including amniocentesis, chorionic villus sampling, and percutaneous umbilical blood sampling.
Physical characteristics of infants born with Down syndrome include epicanthal folds around the eyes, a broad and flat nasal bridge, and a round flat face, eyes that slant upwards, small ears, a short neck, and a downward-turned mouth.
A syndrome is a condition distinguished by a number of features that may occur together at birth, many babies with Down syndrome will have some or all of the following features:
• Low muscle tone (a floppy baby)
• A face that appears flat with eyes slanting upward
• Small cars and a wider neck than usual
• A create across the palm of the hand and a gap between the first and second toes ‘sandal- zap' sign)
• Children with Downs syndrome vary considerably between individuals but may have variety of health problems including those which affect the heart digestive system and general development
• It is very unlikely that any one child with Down syndrome will be all of the Centres commonly associated with the syndrome While intellectual disability is a feature of the syndrome, those with the condition develop and learn throughout life, but at a slower pace than Early intervention programs are very effective in maximizing the potential of children wide Down syndrome.
Trisomy 21 in the primate lineage
Genetic lines of evidence indicate that the ancestral most 21 raised 30-50 million years ago. Interestingly, the condition of trisomy 21 is not limited to humans. In non-human apes chromosome 22 is analogues to human chromosome 21. Humans have two less chromosomes than our ape cousin because of a chromosome fusion that occurred several million years ago to produce human chromosome 2. Trisomy 22 is the genetic equivalent of Down syndrome in apes and has been reported in both a chimpanzee and orangutan. Taken together, these lines of evidence indicate that trisomy 21 has an incredibly long history in the primate lineage.
Scope and limitation of the study
This retrospective study will examine eight years (January 2006 December 2007) record of Paediatrics clinics for cases of Down's syndrome in University of Abuja Teaching Hospital (UATH Extending the period of study ever eight years of strategically situated hospital in the Federal capital Territory provides a large sample sire to allow the appreciation of the prevalence of the disease. It took until 1982 for Adeyokunnu, University College Hospital, Ibadan, Nigeria during a 9-year period (April 1972 to December 1980) to lay to rest the myth of the rarity of DS in Africans. Since then, very little further research has been undertaken, possibly because of the emphasis in Africa on the eradication of malnutrition and infectious diseases, coupled with the continuing lack of awareness of the incidence of DS and difficulties inherent in the diagnosis of the condition in African neonates. This retrospective study over nine years at the academic hospital, Ibadan, Nigeria, recorded an incidence of 1.16 per 1000 livebirths. It can be anticipated that the DS incidence reported in this series may have been lower than the true incidence owing to incomplete ascertainment of cases, but this was the first paper to document conclusively an incidence of DS in African newborns similar to other populations throughout the world More recently, in three separate prospective studies in South Africa, the DS incidence in African newborns has been shown to be as high as, and in some circumstances higher, than that occurring in other populations. In 1995 Delport et al. documented an incidence of 1.33 per 1000 livebirths in a Pretoria urban academic hospital, and Venter et al. recorded a figure of 2.09 per 1000 livebirths in a rural hospital [2,12]. Before this, Kromberg recorded an interim DS incidence of 1.67 per 1000[3].
Livebirths at an academic hospital in Johannesburg. In these three studies, 52%, 56%, and 55%, respectively, of the mothers of the DS infants were 35 years of age or older. Subsequently the incidence of DS in the latter study has been refined to 1.8 per 1000 livebirths for those infants born in Baragwanath Hospital, Johannesburg, and 1.2 per 1000 livebirths if the deliveries from the surrounding clinic maternity units were included (a G R Kromberg, personal communication.) The latter figures highlight the problem of ascertainment of cases in the South African studies and probably the Nigerian study. Owning to pressure on available beds, it is the policy in most South African maternity units to discharge all mothers and their infants within 24 hours of delivery if both are considered to be well. This policy, combined with the problems encountered in recognizing the African DS neonate, heighten the likelihood of DS cases not being recognized during the infant's postnatal maternity unit admission. This is highlighted by figures from a study of 55 DS infants and children, 3 months of age and older, seen by the author. In only nine (16.4%) cases was the diagnosis of DS entertained during the patients' post-delivery stay in hospital.
The report by Canfield provides a recent example of a large study to obtain an estimate of the birth prevalence of DS in the U.S [4]. They obtained data from 11 birth surveillance systems that used active-case finding methods. All pregnancy outcomes, including live births, fetal deaths, spontaneous and induced abortions, and all gestational ages were eligible. However, each active surveillance system varied in their case inclusion criteria with respect to pregnancy outcome, gestational age and the ability to ascertain prenatally diagnosed cases from specialized sources. The estimated maternal age-adjusted prevalence of DS based on the surveillance of 22% of the livebirths in the U.S. was 13.65 [95% confidence intervals (CI):13.22- 14.09] per 10,000 live births, or 1/732. This suggests that 5,400 of the 4 million infants born each year in the U.S. have DS. Canfield further investigated differences in maternal-age adjusted prevalence rates among the three major maternal racial/ethnic groups in the U.S [4]. Non-hispanic white, non-hispanic black and hispanic. Compared with non-Hispanic white mothers, the prevalence ratio was 0.77 (95% CI:0.69-0.87) for non-Hispanic black mothers and 1.12 (95% CI:1.03-1.21) for Hispanic mothers. The causes of the differences among racial/ethnic groups identified in this study are important. Differences could be related to technical issues in the study: the authors state that each surveillance system differed in its access to prenatal records and diagnoses, spontaneous abortions, stillbirths, and live births. Thus, completeness of ascertainment among racial/ethnic groups could differ. Prevalence rates could be influenced by factors that affect access to health care in general, such as socioeconomic class or education, Differences could be due to racial/ethnic variation in use of prenatal care, prenatal diagnosis, and/or selective termination. Lastly, there could be important environmental exposures or genetic risk factors beyond maternal age that vary by racial/ethnic group. Each one of these explanations is plausible and carries significant implications for future public health interventions.
Chromosome 21 nondisjunction
Candidate genes for chromosome 21 nondisjunction: Model organisms have been used to identify genes that are important in the proper segregation of chromosomes. Genes involved in the meiotic process (e.g., homologous pairing, assembly of the synaptonemal complex, chiasmata formation, sister chromosome cohesion, meiotic spindle formation) may predispose an organism to chromosome nondisjunction. To date, a large study to investigate the association of variants in these genes with nondisjunction of human chromosome 21 has not been conducted. Candidate gene studies of the folate pathway provide the best example of genetic epidemiological approaches being used to evaluate the association of genetic variants with nondisjunction. James provided preliminary evidence that the 677C>T polymorphism in the methylenetetrahydrofolate reductase (MTHFR) gene increased the chance of having a child with DS (OR 5 2.6; 95% CI: 1.2-5.8) [13]. This polymorphism is associated with an elevation in plasma homocysteine and/or low folate status. The authors hypothesized that low folate status, whether due to dietary or genetic factors, could induce centromeric DNA hypo methylation and alterations in chromatin structure. Such alterations could adversely affect DNA-protein interactions required for centromeric cohesion and meiotic segregation. Later studies of the MTHFR 677C>T polymorphism, as well as several other allelic variants in the folate pathway, generated inconsistent results especially when genotypes were assayed without biomarkers of metabolic phenotype. James provides an excellent review of these studies [14,15]. Those who have examined blood homocysteine levels, a broad-spectrum indicator of nutritional and/or genetic impairment in folate/B12 metabolism, have documented a significantly higher level among the mothers of children with DS compared with control mothers.
Several recent studies have focused on the interaction among genes in the folate pathway and continue to find intriguing correlations. Clearly, this story needs to be pursued [16,17]. Future studies should focus on gene-gene and gene-nutrition interactions in the folate pathway using large sample sizes, appropriate controls and genetic epidemiological methods that adjust for possible confounding due to population substructure [18-21].
Materials and Methods
Research design
This is a quantitative, observational and a longitudinal (retrospective) study that examines the prevalence of Down's syndrome in the Federal Capital Territory over the period of eight years (January 2000 - December 2007).
Data collection
The researcher was introduced to the hospital authority by the College and permission was duly sought from the Chief Medical director, Head of Paediatrics Department and the Head of Medical Records. The Head of Paediatrics Department also introduced the researcher to the Chief Nursing Officers of the five units of the department-Paediatrics out-Patient Department (POPD), Paediatrics Medical Ward (PMW), Paediatrics Surgical Ward (PSW), Special Care Baby Unit (SCBU) and Emergency Paediatrics Unit (EPU) - to allow the researcher access to the Admission/Discharge registers in the respective units. The Head of Medical Records also introduced the researcher to the Unit Head of Evaluation and Research to allow the researcher to retrieve the required folders. Having observed the above protocols, the researcher personally examined and reviewed the Medical records of patients that attended the Paediatrics Clinic of the UATH and those referred to the hospital during the period of study (Table 1).
| Year | Livebirths | No of Cases | Frequency per Livebirth |
|---|---|---|---|
| 2000 | 814 | 1 | 1 in 814 |
| 2001 | 1089 | 1 | 1 in 1089 |
| 2002 | 764 | 1 | 1 in 764 |
| 2003 | 1091 | 3 | 1 in 364 |
| 2004 | 1211 | 1 | 1 in 1211 |
| 2005 | 1263 | 1 | 1 in 1263 |
| 2006 | 1447 | 2 | 1 in 724 |
| 2007 | 1472 | 1 | 1 in 1472 |
| Total | 9151 | 11 | 1 in 832 |
Table 1: The Frequency of Down's syndrome Among 9151 Live births.
Results and Discussion
Prevalence of Down's syndrome
The prevalence of Down's syndrome of 1 in 832 (1.20 in 1,000) livebirths in the present study is similar to the prevalence reported from other parts of the world [1-4], Compared with the Uganda and Gupta in Nigeria; that suggested rarity or nonexistence of Down's syndrome among Africans many years ago, our results show the prevalence that is about five times higher [5-9]. This disparity could be due to the length of the present study, which covered 8 years, compared to others which covered one year. Previous workers' explanations of the apparent rarity or non-existence of Down's syndrome among Africans included early marriage and therefore motherhood at a younger age [22-25]. The low rate recorded in the past may also be explained by early discharge of mothers and their infants owing to inadequacy of beds and problems encountered in recognizing African DS neonates. However, in the present study, the incidence was high since mothers had a mean maternal age of 36.09 years [26-29]. If early maternity acted as a preventive measure against the birth of Down's babies, then high maternal age explains the higher risk of having babies with Down's syndrome as earlier hypothesized[30-33]. No epidemic occurred in Nigeria during the period of the study. There was no statistically significant variation in monthly, seasonal, or annual distribution of the cases [34,35].
The overall instability in the DS rate during the period of study may be influenced by the fact that most cases of Down's syndrome occurred in women older than 35 years of age, where parental age had great influence [36,37].
Karyotyping
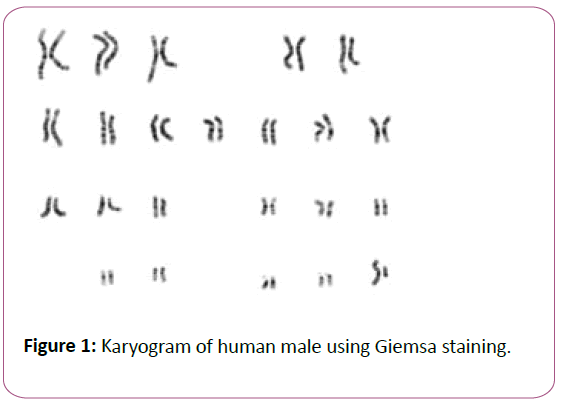
Karyotyping is the process by which photographs of Chromosomes are taken in order to determine the chromosome complement of an individual, including the number of chromosomes and any abnormalities. The term karyotype is also used for the complete set of chromosomes in a species or in an individual organism and for a test that detects this complement or measures the number [38]. Karyotypes describe the chromosome count of an organism and what these chromosomes look like under a light microscope. Attention is paid to their length, the position of the centromeres, banding pattern, any differences between the sex chromosomes, and any other physical characteristics. The preparation and study of karyotypes is part of cytogenetics (Figure 1).
The study of whole sets of chromosomes is sometimes known as karyology. The chromosomes are depicted (by rearranging a photomicrograph) in a standard format known as a karyogram or idiogram: in pairs, ordered by size and position of centromere for chromosomes of the same size.
The basic number of chromosomes in the somatic cells of an individual or a species is called the somatic number and is designated 2n. In the germline (the sex cells) the chromosome number is n (humans: n=23) p28 thus, in humans 2n=46.
So, in normal diploid organisms, autosomal chromosomes are present in two copies. There may, or may not, be sex chromosomes. Polypoid cells have multiple copies of chromosomes and haploid cells have single copies.
Karyotypes can be used for many purposes; such as to study chromosomal aberrations, cellular function, taxonomic relationships, and medicines and to gather information
Conclusion
In conclusion, the prevalence of Down's syndrome in UATH, Abuja, Nigeria is in keeping with those found elsewhere in the world. The findings in this study raise the issues of prenatal counseling for Nigerian women of advanced maternal age and for those with a previous DS infant, selective termination of affected fetuses, and counseling of older mothers regarding the advantages of family planning.
References
- Adeyokunno AA (1982) The incidence of Down syndrome in Nigeria. Med Genet 19(4):277-9.
- Delport SD, Christianson AL, van den Berg HJS, Wolmarans L, Gericke GS (1995) Descriptive profile of congenital anomalies in black South African neonates born in an urban hospital. SAfrMedJr 85: 15-20.
- Kromberg JGR, Christianson AL, Duthie-Nurse G, Zwane E, Jenkins T (1992) Down syndrome in the black population. S Afr Med 81(6):337.
- Canfield MA, Honein MA, Yuskiv N, Xing J, Mai CT, et al. (2006) National estimates and race/ethnic- specific variation of selected birth defects in the United States, 1999-2001. Birth Defects Res A Clin Mol Teratol 76(11):747-756.
- Tooth G (1950) Studies in mental illness in the Gold Coast. Colonial Research Publication Series No 6. London: HMSO.
- Jellife DB (1954a) Aetiology of mongolism. Lancet; ii:871.
- Jellife DB (1954b) Mongolism in Jamaican children. West Indian MedJ 3:164-5.
- Carter CO (1967) Congenital Malformations. WHO Chron 21: 287-92.
- Simpkiss M, Lowe A (1961) Congenital abnormalities in the African newborn. Arch Dis Child 36(118): 404-6.
- Gupta B (1969) Incidence of congenital malformations in Nigerian children. West Afr MedJ 11:22-5.
- Lejeune J, Gautier M, Turpin R (1959) "Etude des chromosomes somatiques de neuf enfants mongoliens". Comptes Rendus Hebd Seances Acad Sci 248 (11): 1721 -22.
- Venter PA, Christianson AL, Hutamo CM, Makhura MP, Gericke GS (1995) Congenital anomalies in rural black South African neonates - a silent epidemic?. S Afr Med 85:11-15.
- James SJ, Pogribna M, Pogribny IP, Melnyk S, Hine RJ, et al. (1999) Abnormal folate metabolism and mutation in the methylenetetrahydrofolate reductase gene may be maternal risk factors for Down syndrome. Am J Clin Nutr 70(4): 495-501.
- James SJ (2004) Maternal metabolic phenotype and risk of Down syndrome: beyond genetics. Am J Med Genet A 127(1):1-4.
- James SJ (2004) Response to letter: Down syndrome and folic acid deficiency. Am J Med Genet A 131(3):328-329.
- King RC, Stansfield WD, Mulligan P K (2006). A dictionary of genetics (7th ed.). Oxford University Press. p. 242.
- Richard F, B. Dutrillaux (1998) Origin of human chromosome 21 and its consequences: a 50-million-year-old story. Chromosome Research 6(4): 263- 8.
- Kasai F, Takahashi K, Koyama K, Terao Y, Suto K, et al. (2000) Comparative FISH mapping of the ancestral fusion point of human chromosome 2. Chromosome Res 8(8): 727-35.
- Wienberg JA. Jauch HJL, Senger G, Horsthemke B, Claussen U, et al. (1994) The origin of human chromosome 2 analyzed bycomparative chromosome mapping with a DNA microlibrary. Chromosome Res 2(5): 405-10.
- Yunis JJ, Prakash O (1982) The origin of man: a chromosomal pictorial legacy. Science 215 (4539): 1525-30.
- McClure HM, Belden KH, Pieper WA, Jacobson CB (1969) Autosomal trisomy in a chimpanzee: resemblance to Down's syndrome. Science 165(897): 1010-2.
- Luder J, Musoke LK (1955) Mongolism in Africans. Arch Dis Child 30(152):310-5.
- Leather CM, Leather HM (1957) An African mongol. East Afr MedJ 34(11): 589-92.
- Macgregor M (1958) Paediatrics in Western Nigeria. Arch Dis Child 33(170): 277-91.
- Hassan MM (1962) Mongolism in Sudanese children. J Trop Pediatr 8:48-50.
- Tompkins AB (1964) Down's syndrome in Nigerian children. J Med Genet 1(2): 115-7.
- Boroffice RA (1977) Chromosomal studies of 58 cases of Down's syndrome in Nigeria: type and frequency of chromosomal aberrations. Niger Med J 7: 323-9.
- Christianson AL, Kromberg JGR (1996) Maternal non-recognition of Down syndrome in black South African infants. Clin Genet 49(3): 141-4.
- Khoshnood B, De VC, Vodovar V (2004) A population-based evaluation of the impact of antenatal screening for Down's syndrome in France, 1981-2000. Br J Obstet Gynaecol 111: 485-490.
- Khoshnood B, De VC, Vodovar V, Bréart G, Goffinet F, et al. (2006) Advances in medical technology and creation of disparities: the case of Down syndrome. Am J Public Helath 96(12): 2139- 2144.
- Coory MD, Roselli T, Carroll HJ (2007) Antenatal care implications of population-based trends in Down syndrome birth rates by rurality and antenatal care provider, Queensland, 1990-2004. Med J Aust 186(5):230-234.
- Forrester MB, Merz RD (1999) Prenatal diagnosis and elective termination of Down syndrome in a racially mixed population in Hawaii, 1987-1996. Prenat Diagn 19(2):136-141.
- Siffel C, Correa A, Cragan J, et al. (2004) Prenatal diagnosis, pregnancy terminations and prevalence of Down syndrome in Atlanta. Birth Defects Res A Clin Mol Teratol 70(9): 565-571.
- Hook EB, Cross PK (1988) Maternal cigarette smoking. Down syndrome in live births, and infant race. Am J Hum Genet 42(3): 482-489.
- Hobbs CA, Sherman SL, Yi P, Torfs CP, Hine RJ, et al. (2000) Polymorphisms in genes involved in folate metabolism as maternal risk factors for Down syndrome. Am J Hum Genet 67(3): 623-630.
- O'Leary VB, Parle-McDermott A, Molloy AM, Kirke PN, Johnson Z, et al. (2002) MTRR and MTHFR polymorphism: link to Down syndrome?. Am J Med Genet. 107(2): 151-155.
- Bosco P, Gueant-Rodriguez RM, Anello G, Barone C, Namour F, et al. (2003) Methionine synthase (MTR) 2756 (A-> G) polymorphism, double heterozygosity methionine synthase 2756 AG/methionine synthase reductase (MTRR) 66 AG, and elevated homocysteinemia are three risk factors for having a child with Down syndrome. Am J Med Genet A 121(3):219-224.
- Stebbins GL (1950) "Chapter XII: The Karyotype". Variation and evolution in plants. Columbia University Press.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences