ISSN : 2348-9502
American Journal of Ethnomedicine
The Accuracy of Teledermatology Storeand- Forward e-Triage in Diagnosing and Treating Patients of the National Health Service in the United Kingdom
1Department of Dermatology, Royal Wolverhampton NHS Trust, University of Birmingham, Wolverhampton, UK
2Department of Dermatology, Royal Wolverhampton NHS Trust, Wolverhampton, UK
- *Corresponding Author:
- Mohammed Al Abadie
Department of Dermatology
Royal Wolverhampton NHS Trust, Wolverhampton, UK
Tel: +1214143344
E-mail: mohammed.abadie@nhs.net
Received Date: November 08, 2018; Accepted Date: November 28, 2018; Published Date: December 04, 2018
Citation: Abadie MA, Al-Rubaye M, Abadie DA, Oumeish F (2018) The Accuracy of Teledermatology Store-and-Forward e-Triage in Diagnosing and Treating Patients of the National Health Service in the United Kingdom. Am J Ethnomed Vol.5 No.2:12
DOI: 10.21767/2348-9502.100012
Abstract
Introduction: Teledermatology is a tool that is being used in many parts of the world to help provide dermatological expertise in the diagnosis and management of skin conditions for people who lack access to specialist services. The purpose of this study was to evaluate the accuracy of teledermatology store-and-forward e-triage in diagnosing and treating patients of the NHS in the United Kingdom when compared to the standard outpatient face-to-face consultation.
Methods: After obtaining consent to join the study our research nurse photographed the patients and took a short history before they were assessed by our consultant dermatologist in a face-to-face consultation who would provide a diagnosis and treatment plan on the day. The same consultant dermatologist would then assess the pictures and history taken by our research nurse and provide a diagnosis and treatment plan for the same patient at a later date. 46 skin complaints in 44 patients were assessed after the 3 months and the diagnoses and management plans of the 2 different methods were compared.
Conclusion: The results showed a high diagnostic correlation of 82% (38/46 cases) and a higher management plan accuracy of 85% (39/44 cases). These promising results have demonstrated that teledermatology store-and-forward e-triage can be an important but relatively accurate tool in providing skin specialist services for patients and areas where these services are scarce if provided.
Keywords
Telemedicine; Teledermatology; Store-and-forward e-triage
Introduction
‘Telemedicine’ is defined as the use of any means of communication in healthcare preferentially with help of images or visual aids in interchange for medical information for the management, diagnosis and prevention of disease and for the continuing education of healthcare providers all in the interest of advancing the health of individuals and their communities [1]. Telemedicine is used in two main modalities; Store-and-forward modality and live interaction modality [2], each one of them having their own benefits and disadvantages. In 1995 Perednia and Brown were the first to use the term ‘Teledermatology’ when it was used in the rural areas of Oregon in the United States of America due to the lack of dermatology or skin specialty services provided [3,4]. Teledermatology has since grown significantly and many papers were published over the last 2 decades regarding the way it has evolved and the significant impact it has had on doctors and patients alike. In essence the fact that dermatology revolves around photographic and visual clues to make a diagnosis has allowed teledermatology to flourish and grow rapidly around the world especially in areas where skin specialties are so sparse and needed [5,6]. Teledermatology is currently being used in different types of healthcare and medical settings such as hospital and primary care settings but also nursing homes and care homes. It is also being used to provide care in the developing world where many people who reside in areas with no access to dermatology expertise are benefiting from consultations being provided in developed countries [7,8]. In the United Kingdom, Teledermatology is seen as a tool to provide general practitioners fast access to secondary care skin specialist opinion especially in rural areas where patients have to travel long distances for dermatological access due to limited availability of specialists and centers (Figure 1) [9-11]. The growth in demand to provide dermatology services in secondary care in the United Kingdom has increased significantly over the last two decades which has led to an enormous amount of pressure on dermatologists but also more importantly extremely long waiting times [12]. This has created a large problem for primary care physicians and skin care specialists but also for patients who have grown frustrated with their skin problems due to the difficulty in obtaining specialist input. The teledermatology e-triage system can build new clinical networks between the primary and secondary care doctors which can result in an improvement of the service and direct healthcare to the patient in particular especially those that would have to travel long distances in addition to the long waiting times.
Figure 1: Images sent from a rural area to a secondary care dermatology consultant in a remote area to aid in the diagnosis and management of a skin disease and to help reduce waiting times for patients.
Aim of the Study
To demonstrate and evaluate the accuracy of diagnosing National Health Service patients referred from primary care General practitioners. At the same time not only evaluating the accuracy of the diagnosis but also evaluating the treatment and management plan proposed by the dermatologist using the system.
Method
Our research was based on the National Health System and on seeing patients who were initially referred by General practitioners for further dermatological advice and it is important to bear in mind that the average waiting time for such a nonurgent consultation/referral may take up to 3 months. In this study the diagnosis and treatment plan for adult patients referred to the dermatologist was recorded by teledermatology store-and-forward, e-triage and the outpatient face-to-face consultation for the same patients by the same dermatologist. The e-triage system used was provided by Symbermedica, United Kingdom. This e-triage system allowed primary care healthcare professionals to capture clinical information including structured proformas, questionnaires and digital photographs. This was then sent out through a secure network to remote consultant skin specialists for reporting. Patients referred to secondary care were asked to be involved in the study and after obtaining their consent they were asked to attend half an hour prior to their appointment with the consultant. They were then seen by a research nurse who would then take a thorough history followed by a photograph of the affected area or areas by using the average camera of 5 megapixels. This was then combined with the clinical information obtained through the General practitioner’s records and the patient would proceed to see the consultant dermatologist however only the General practitioner letter would be used in the consultation. After three months of storing the clinical information the results of the two different methods of consultation were compared. Both patient groups had the exact same constants in that the same consultant dermatologist produced a diagnosis and management plan and the disease was assessed before the dermatologist started any treatment. During the three-month period we were able to include 44 patients in the study and we were able to compare the e-triage diagnosis and treatment plan with the direct face to face diagnosis and management plan made by the same consultant.
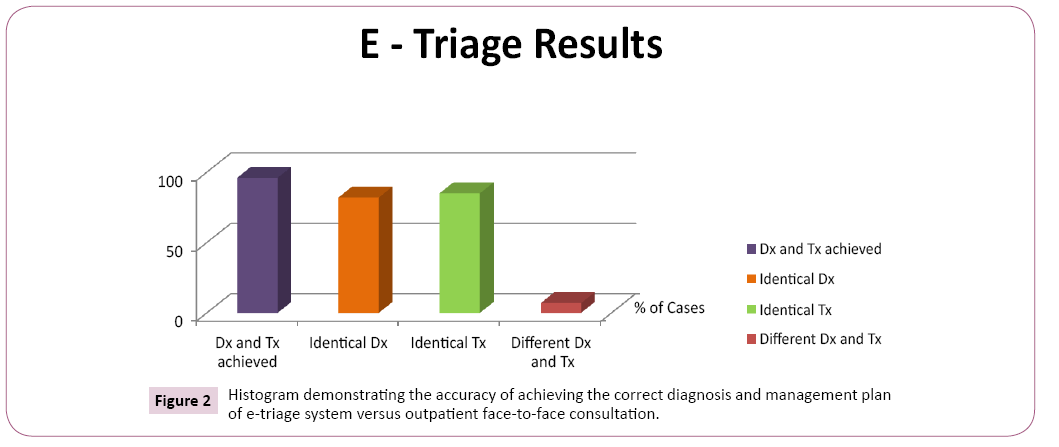
Results
A store-and-forward e-triage diagnosis and treatment plan was achieved in 96% (44) of cases. 46 skin complaints were assessed in 44 patients. It showed 82% (38 cases) diagnostic and 85% (39 cases) treatment planning accuracy of the e-triage diagnosis when compared to the outpatient consultations. In 7% (3) of cases there was no agreement in either a diagnosis or treatment plan (Figure 2). In 4% (2) of cases no e-triage diagnosis or treatment plan was reported due to poor image quality or unknown identity of a patient. An unclear picture (Table 1) was the most common cause for a discrepancy between in the diagnoses of the 2 methods but some of the differences were due to the fact that the patients required further tests such as Woods light or dermatoscopy. However in 1 of the 8 cases (12.5%) in which there was an unclear picture a biopsy was required to confirm the diagnosis. It was also noted that patients with skin types 3-6 ethnicity were more difficult to assess using store-and-forward e-triage as they made up 37.5% (3/8) of the cases in which there was a discrepancy. In most cases an accurate diagnosis and treatment plan was delivered by the e-triage system and in the cases where the diagnosis or management did not match no significant morbidity or adverse events followed.
Table 1: This table demonstrates the reasons for a difference between the diagnoses of patients being assessed by the 2 different methods. An unclear picture and the requirement for further tests were the most common culprits for this discrepancy.
| Skin type | Presentation | Reason for discrepancy | Treatment required | Biopsy required | |
|---|---|---|---|---|---|
| Case 1 | 1-2 | Rash/medical | Unclear picture | Yes | No |
| Case 2 | 1-2 | Rash/medical | Unclear picture | Yes | No |
| Case 3 | 5-6 | Lesion/surgical | Needing dermoscopy | No | No |
| Case 4 | 3-4 | Lesion/surgical | Unclear picture | Yes | Yes |
| Case 5 | 1-2 | Lesion/surgical | Needing dermoscopy | No | No |
| Case 6 | 1-2 | Lesion/surgical | Unclear picture | N/A | N/A |
| Case 7 | 3-4 | Rash/medical | Needing Wood’s light | Yes | No |
| Case 8 | 1-2 | Lesion/surgical | Unknown identity of patient | N/A | N/A |
Figure 2: Histogram demonstrating the accuracy of achieving the correct diagnosis and management plan of e-triage system versus outpatient face-to-face consultation.
Discussion
The results of this study show a high diagnostic correlation between the patients assessed by the teledermatology e-triage system and the patients who were assessed by the face-to-face direct consultation. In the majority of the skin complaints (82% or 38 cases), the diagnosis was the same however in 18% the diagnosis was different. Many factors could be responsible for the difference in the diagnosis namely not being able to clinically assess the rash or lesion directly and not being able to feel the skin to compare if it is rough or smooth. Another factor would be not being able to use medical equipment to help aid in diagnosing lesions such as a dermatoscope or Wood’s light. Although the diagnostic correlation between the 2 methods was high the aforementioned factors could be some of the contributing reasons to the low but significant number of cases in which the diagnosis was different. There was a discrepancy in 8/46 cases (18%) and in the majority of those an unclear picture was a contributing factor. The fact that a face-to-face consultation has many more advantages such as getting the history directly from the patient and being able to assess specific lesions or rashes directly with or without the use of dermatological equipment makes it a more reliable way of yielding a more accurate diagnosis. The fact that 8 of the cases assessed by the e-triage teledermatology method yielded a different diagnosis to the face-to-face consultation and this resulted in a different management plan in the majority of those cases. The results show us that some factors may influence the dermatologist to favoring a certain diagnosis in face-to-face consultations, which would result in a different management plan. Teledermatology can also work as an educating tool to primary care physicians where they send challenging cases and patients for diagnosis and treatment but also benefiting from advice on best ways to contribute to a management plan. Improvement on the technology and quality of cameras will improve the outcome in ethnic minority skin types 3-6 and at the same time taking more detailed pictures and to include pictures with a dermatoscope attached to the camera will further enhance the outcome.
Conclusion
Teledermatology can be an effective way of providing dermatological specialist opinion to patients with no access to secondary care. It has been used in rural areas where dermatology specialist services are scarce and it has been used in developing areas where access to secondary care is limited or non-existent. The benefit of teledermatology is the fact that dermatology as a specialty revolves around imaging or visual clues i.e. the answer may be visible to the naked eye. In this study we compared two sets of methods in obtaining a diagnosis of the same patient made by the same consultant. The 2 methods were teledermatology store-and-forward e-triage method and the old-fashioned faceto- face outpatient consultation. The results were promising in that we yielded a high diagnostic sensitivity of 82% or 38 out of 46 skin complaints. This resulted in a slightly higher management plan correlation of 85% (39/46). The difference in the diagnostic correlation may have been due to poor imaging quality or due to clinical disadvantages in the store-and-forward e-triage system such as not being able to use dermatological equipment, or take a face-to-face medical history and not being able to feel the skin. The results however show that the teledermatology method can be a useful tool to dermatologists, primary care physicians but most importantly patients who lack resources and those who are unable to access secondary care dermatological services.
References
- World Health Organization (1998) A health telematics policy in support of WHO’s Health for global health development: report of the WHO group consultation of health telematics. December, Geneva, 1997, World Health Organization.
- Loane MA, Bloomer SE, Corbett R, Edey DJ, Hicks, et al. (2000) A comparison of real time and store-and-forward teledermatology: A cost-benefit study. Br J Dermatol 143: 1241-1247.
- Perednia DA, Brown NA (1995) Teledermatology: one application of telemedicine. Bull Med Libr Assoc 83: 42-47.
- Armstrong AW, Wu J, Kovarik CL (2012) State of teledermatology program in the United States. Am Acad of Dermatol 67: 939-44.
- Tensen E, van der Heijden JP, Jaspers MWM, Witkamp L (2016) Two decades of teledermatology: Current Status and integration in National Healthcare systems. Curr Dermatol Rep 5: 96-104.
- Coates SJ, Kvedar J, Granstein RD (2015) Teledermatology: from historical perspective to emerging techniques of the modern era: part I: history, rationale, and current practice. J Am Acad Dermatol 72: 563-574.
- Ford JA, Pereira A (2015) Does teledermatology reduces secondary care referrals and is it acceptable to patients and doctors? A service evaluation. J Eval Clin Pract 21: 710-716.
- Ismail A, Stoff BK, McMichael JR (2018) Store-and-forward teledermatology service for primary care providers in Afghanistan. Int J Dermatol.
- Cheung CM, Muttardi K, Chinthapalli S, Ismail F (2018) Pilot Teledermatology Service for Assessing Solitary Skin Lesions in a Tertiary London Dermatology Center. J Healthc Qual 9.
- Gregory S, Llewellyn C (2018) Store and forward Teledermatology - The Newport way. J Vis Commun Med 41: 45-51.
- Livingstone J, Solomon J (2015) An assessment of the cost-effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. London J Prim Care 7: 31-35.
- Senel E, Demir E, Artuz RF (2018) Bibliometric Evaluation of Global Productivity of Teledermatology Publications between 1975 and 2017 with a 3-Year Update. Indian J Dermatol 63: 437-439.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences