Successful Approaches to Common Urinary Problems in Postmenopausal Women
Emad E Shoukry*
Division of Geriatrics, University of North Texas, TX, USA
- *Corresponding Author:
- Emad E Shoukry
Assistant Professor of Medicine
Division of Geriatrics
University of North Texas
Fort Worth, TX, USA
Tel: 817735 2660
E-mail: Emad.Shoukry@unthsc.edu
Received Date: August 08, 2017; Accepted Date: August 22, 2017; Published Date: August 29, 2017
Citation: Shoukry EE (2017) Successful Approaches to Common Urinary Problems in Postmenopausal Women. J Clin Med Ther. 2:21.
Commentary
Urological problems are common in postmenopausal women. In this article we will discuss successful interventions for some of them, including Urgency Incontinence (UI), Stress Incontinence (SI), recurrent Urinary Tract Infections (UTIs) and neurogenic (atonic) bladder.
Urinary incontinence is the involuntary leakage of urine. In a study of postmenopausal women, about 56% reported this problem at least weekly [1]. There are 6 different subtypes of urinary incontinence: stress incontinence (most common type in postmenopausal women), urgency incontinence, mixed incontinence combining features of the aforementioned 2 types, overflow incontinence, functional incontinence and lastly true incontinence usually related to a postoperative vesicovaginal or ureterovaginal fistula.
Urgency Incontinence
UI is a common and potentially disabling condition affecting 15-30% of those aged 65 years and older.
Therapeutic options for UI include behavioral therapy, pharmacologic treatment (antimuscarinic agents, Beta 3 agonist), neuromodulation and chemodenervation. Weight loss and exercise is recommended in obese patients with urgency incontinence.
Behavioral therapy consists of a voiding diary, limiting fluid intake, avoiding caffeinated beverages, scheduled toileting every 2 hrs during the day and urge suppression (also referred to as bladder training). When the patient feels the urge to void, she should keep still, squeeze pelvic muscles quickly 5 times, relaxation techniques should be attempted while the patient is trying to distract herself and wait till the urge subsides then she can go to the bathroom. Urge suppression may not be successful in frail elderly women and is difficult to implement in those with cognitive impairment. Low quality evidence showed that bladder training improved UI compared with no active treatment.
There is some evidence that pharmacologic treatment with antimuscarinic agents, e.g. Darifenacin, Fesoterodine, Oxybutynin, Solifenacin, Tolterodine, Trospium, improved UI compared to placebo with NNT (Number needed to treat) to improve symptoms ranging from 6 to 10 patients. They may achieve continence and improve quality of life. Side effects of antimuscarinic agents include urinary retention, dry mouth, constipation, nausea, blurred vision, tachycardia, confusion. They are contraindicated in patients with narrow angle glaucoma. Agents that do not cross the blood brain barrier, e.g. Trospium, are preferred in the elderly. Moderate quality evidence showed that the B3 Agonist, Mirabegron achieved continence and improved UI more than placebo. B3 Agonists are associated with hypertension, arrhythmias.
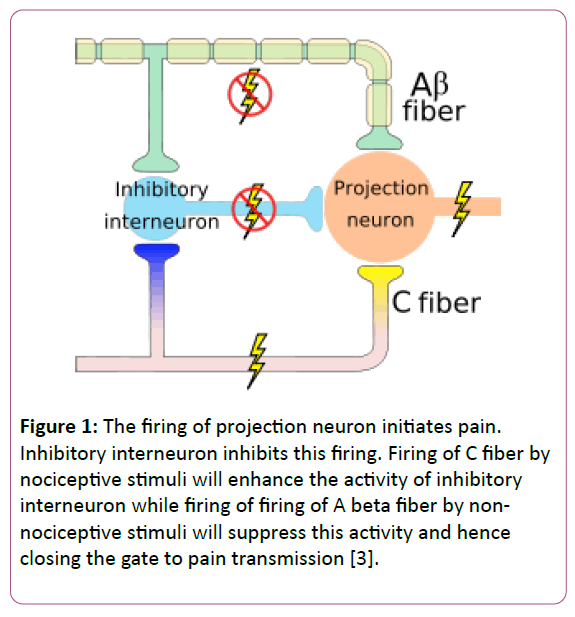
Neuromodulation is based on the pain gate control theory published for the first time in 1965 [2]. This theory asserts that stimulation of thick myelinated fibers, e.g. A beta fibers, is able to suppress painful stimuli conveyed by smaller unmyelinated fibers, e.g. C fibers (Figure 1).
Figure 1: The firing of projection neuron initiates pain. Inhibitory interneuron inhibits this firing. Firing of C fiber by nociceptive stimuli will enhance the activity of inhibitory interneuron while firing of firing of A beta fiber by non-nociceptive stimuli will suppress this activity and hence closing the gate to pain transmission [3].
It is postulated that Neuromodulation of sacral nerves at a specific frequency can inhibit afferent nociceptive fibers from the urinary bladder and hence suppress the urgency. Modalities to treat UI include sacral neuromodulation and percutaneous tibial nerve stimulation.
Sacral neuromodulation was approved by the FDA to treat urgency incontinence. After ruling out treatable causes of UI, e.g. stones, interstitial cystitis, tumor…, the patient receives a temporary external pulse generator connected via wire leads to S3.
After 1-2 weeks, if the patient symptoms improve by >50%, a permanent stimulator is implanted in the hip area in the subcutaneous tissue. The programming of the stimulator can be adjusted to improve symptoms. Age doesn’t appear to affect efficacy of the procedure.
Percutaneous tibial nerve stimulation is an office procedure where a needle electrode is inserted 5 cm above the medial malleolus for 30 min weekly for a total of 12 weeks. According to some studies, response rate is about 54% [4] in patients with UI who failed antimuscarinic drug and complete recovery was maintained in 42% of those patients at 1 year.
Chemodenervation using intravesical injection of Botulinum toxin acts by inhibiting presynaptic release of Acetylcholine. A recent study [5] showed that Chemodenervation was superior to sacral neuromodulation in decreasing the number of daily incontinence episodes and in complete symptom resolution at 6 months. However, the Botulinum toxin group has higher rate of UTI compared to neuromodulation group at 6 months (35% vs. 11%) and a greater need for self-catheterization (8% of patients in chemodenervation group at 1 month, 4% at 3 month and 2% at 6 month). Intravesical injection of the toxin usually needs to be repeated every 9 months.
Stress Incontinence
Stress incontinence affects about 25 million American women. Therapeutic options include behavioral therapy, Kegel exercise, alpha agonists, e.g. pseudoephedrine, midodrine, and surgery. Duloxetine, a Serotonin Norepinephrine Uptake Inhibitor (SNRI) has been approved by European regulatory authorities, but not the FDA, for treatment of stress incontinence. Onuf’s nucleus is a group of motoneurons located in the anterior horn of the sacral region and is the origin of the pudendal nerve. Pudendal nerve is involved in the control of external urethral sphincter. Onuf’s nucleus is rich in Norepinephrine and Serotonin receptors. A small RCT demonstrated promising results with 24% of patients on Duloxetine declining their planned procedure for SI. Of note 48% of the patients didn’t tolerate the dose of 40 mg orally twice daily [6].
Recurrent UTI
Recurrent UTI is the most common bacterial infection in postmenopausal women. At least 2 RCT showed that intravaginal Estrogen reduces the incidence of UTI in this patient group by one third to three quarters [7]. If topical application is not feasible, women can use Estradiol vaginal ring, which can be replaced every 3 months. Lactobacillus, taken orally [8] or applied as vaginal suppositories [9] showed a trend towards fewer UTI. Cranberry data regarding that indication are mixed.
Neurogenic (Atonic) Bladder
The intraurethral valve pump, marketed as Inflow, is a device that can be used in women with Neurogenic or atonic bladder. A single use urethral insert is inserted initially by a physician, after sizing of the patient’s urethra, using an introducer. Once inside the urinary bladder, fins are deployed and keep the device in place (Figure 2). To void, the patient sits on a toilet holding a remote control over the lower pelvis. Once a button is pushed, an internal pump drains the urine out and when the button is released, a valve is engaged blocking further urine flow. The device needs to be changed every 29 days, typically by a caregiver. The device is easy to remove by the patient herself if needed. The device was approved by FDA in 2014 and is indicated for females 18 years or older. A study of 60 subjects showed an incidence of UTI of 3.3% compared to 12% for clean intermittent catheterization, after 5 years. The abandonment of the prosthesis was noted to be around 50% within the first 15 days [10].
In summary, it is advisable to follow a stepwise approach in treating urinary incontinence in postmenopausal women. Behavioral therapy is initially attempted and if unsuccessful pharmacologic treatment is indicated. If the patient didn’t control her symptoms or did develop side effects related to pharmacotherapy, other approaches as outlined above can be attempted [11-13].
References
- Brown JS, Grady D, Ouslander JG, Herzog AR, Varner RE, et al. (1999) Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Heart & Estrogen/Progestin Replacement Study (HERS) Research Group. Obstet Gynecol 94: 66-70.
- Melzack R, Wall PD (1965) Pain mechanisms: a new theory. Science 150.
- Kandel ER, Schwartz JH, Jessell TM (2000) Principles of neural science (4thedn.). McGraw-Hill, pp: 482-486.
- Nuhoglu B, Fidan V, Ayyıldız A, Ersoy E, Germiyanoğlu C (2006) Stoller afferent nerve stimulation in woman with therapy resistant over active bladder; a 1-year follow up. Int Urogynecol J Pelvic Floor Dysf 17: 204-207.
- Amundsen CL, Richter HE, Menefee SA, Komesu YM, Arya LA, et al. (2016) Onabotulinumtoxin A vs. Sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA 316: 1366-1374.
- Swift S, Morris S, McKinnie V, Freeman R, Petri E, et al. (2006) Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J Pelvic Floor Dysfunct 17: 615-620.
- Perrotta C, Aznar M, Mejia R, Albert X, Ng CW (2008) Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev.
- Beerepoot MA, ter Riet G, Nys S, van der Wal WM, de Borgie CA, et al. (2012) Lactobacilli vs antibiotics to prevent urinary tract infections: a randomized, double-blind, noninferiority trial in postmenopausal women. Arch Inter Med 172: 704-712.
- Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, et al. (2011) Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis 52: 1212-1217.
- Mazouni C, Karsenty G, Bladou F, Serment G (2004) Urethral device in women with chronic urinary retention: an alternative to self-catheterization? Eur J Obstet Gynecol 115: 80-84.
- Gibbs CF, Johnson TM, Ouslander JG (2007) Office management of geriatric urinary incontinence. Am J Med 120: 211-220.
- Reuben DB, Herr KA, Pacala JT, Pollock BG, Potter JF, et al. (2005) Geriatrics at your fingertips (19th edn.). American Geriatrics Society, USA pp: 155-157.
- Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, et al. (2010) Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Ann Inter Med 161: 429-440.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences