ISSN : 2348-1927
Annals of Biological Sciences
Serum Nitric Oxide Levels and Acid-Base Status of Preeclamptic Wister Rats Exposed to Methanolic Leaf Extracts of Selected Plants
Kenneth Atoe1,2,3* Beckley Ikhajiagbe2,3 and Macdonald Idu3
1Department of Chemical Pathology, Edo State University Uzairue, Edo State, Nigeria
2Department of Microbiology, University of Benin, Benin, Nigeria
3Department of Plant Biology and Biotechnology, University of Benin, Benin, Nigeria
- *Corresponding Author:
- Kenneth Atoe
Department of Chemical Pathology,
Edo State University Uzairue, Edo State,
Nigeria,
E-mail: atoe.kenneth@edouniversity.edu.ng
Received date: July 11, 2022, Manuscript No. ABS-22-14114; Editor assigned date: July 13, 2022, PreQC No. ABS-22-14114 (PQ); Reviewed date: July 25, 2022, QC No. ABS-22-14114; Revised date: August 04, 2022, Manuscript No. ABS-22-14114 (R); Published date: August 11, 2022, DOI: 10.36648/ 2348-1927.10.8.37
Citation: Atoe K, Idu M, Ikhajiagbe B (2022) Serum Nitric Oxide Levels and Acid-Base Status of Preeclamptic Wister Rats Exposed to Methanolic Leaf Extracts of Selected Plants. Ann Bio Sci Vol.10 No.8:37.
Abstract
It has been hypothesized that preeclampsia starts a chain reaction that reduces placental perfusion and causes extensive maternal vascular endothelium dysfunction. Due to low oxygen levels in the placenta, diminished nitric oxide synthase eventually results in low nitric oxide levels and a corresponding rise in lactate levels. The utilization of methanolic extracts of Jatropha curcas, Alchornea cordifolia, and Secamone afzelii were investigated in induced preeclampsia using Wistar rats in an effort to increase oxygenation. The animals received oral plant extract doses of 50, 100, and 200 mg/kg once daily while being handled in compliance with international standards for the care and management of laboratory animals. Methyldopa, 100 mg/kg, was the typical medication. A model BT-500 plus Automatic Electrolyte Analyzer was used to assess the bicarbonate content, while lactate and nitric oxide levels were measured using a colorimetric approach. The results revealed that although nitric oxide levels in preeclamptic rats were lower during the third trimester (12.4 units) and the postpartum period (10.4 units) compared to the control group (10.7-12.5 unit), the administration of 100 mg/kg of Alchornea cordifolia enhanced nitric oxide levels. When preeclamptic rats were given 100 mg/kg of S. alfzelii, significantly elevated lactate levels (40.7-55.9 units) in preeclampsia were reduced to as low as 25.5 units.
Keywords
Preeclampsia; Jatropha curcas; Alchornea cordifolia; Secamone afzelii; Nitric oxide; Lactate; Bicarbonate
Introduction
During pregnancy, numerous changes in the cardiovascular system occur to reduce maternal vascular resistance thereby increasing maternal oxygen delivery which is necessary to meet the increased metabolic demand and higher oxygen consumption during pregnancy [1]. It has been proposed that nitric oxide as the physiological agent involved in this mechanism as it regulates feto-placental, vascular permeability and resistance and platelet aggregation in the placenta [2,3]. Conrad et al. shown that maturation and development of the placenta is affected significantly by epigenetics and therefore an epigenetic molecule such as nitric oxide has been postulated to affect foetal programming [4] and foetal survival [5]. Nitric oxide is synthesized from l-arginine oxygen and tetrahydrobiopterin as a cofactor [6]. Endothelial nitric oxide produces vascular smooth muscle relaxation via its action through cyclic guanosine monophosphate dependent pathway [7]. In abnormal fetomaternal vascular adaption such as preeclampsia and gestation diabetes mellitus, nitric oxide has also been implicated [8]. However, some researchers have shown that endothelial derived nitric oxide has a significant role in cardiovascular alterations in pregnancy [9]. Some researchers demonstrated that nitric oxide level increase with gestation during normal pregnancy returning to non-pregnant level dome time postpartum [10].
During the second and third trimester of pregnancy in relation to control non pregnant subject, serum nitric oxide concentration of the healthy pregnant women was significantly higher [11]. The endothelium contributes to the hemodynamic changes associated with normal pregnancy due to increased production of nitric oxide. However, a reduction in nitric oxide signaling has been observed in preeclampsia and in several forms of chronic hypertension [12]. Preeclampsia is deemed to be one of the most significant health problems in pregnancy, complicating 6-10% of all gestation over 20 weeks, 14-20% of multiple chronic hypertension [13,14]. Preeclampsia has been postulated to initiate activity resulting in reduced placental perfusion that leads to widespread dysfunction of the maternal vascular endothelium [15]. There is reduced nitric oxide synthase which eventually leads to low nitric oxide levels and a concomitant increase in lactate levels due to poor oxygen levels in the placenta [16]. Nitric oxide is a potent vasodilator released by endothelial cells; it inhibits platelet aggregation and adhesion to vascular endothelial surfaces. Because endothelial cell damage is considered pivotal in the pathogenesis of preeclampsia, a study by Seligman et al. was initiated to determine whether nitric oxide production is decreased in patients with preeclampsia. The researchers reported that circulating levels of nitrite are decreased in patients with preeclampsia. This data support the concept that diminished nitric oxide synthesis contributes to the pathophysiologic changes seen in preeclampsia.
The role of nitric oxide on fetal cardiovascular development is only partially known. Furthermore, children are at greater risk of developing cardiovascular disease later in life in women who had preeclampsia [17]. Nitric oxide likely contribute to the transformation of epithelium mesenchyme in the areas of the endocardial cushion, myocardial and angiogenesis and myocardial remodeling impaired production of nitric oxide in the heart lead to structural congenital abnormalities, resulting in heart failure and increased mortality [18].
Studies had shown that normal fetal metabolism results in the production of acids (carbonic and organic), due to efficient buffer mechanisms of the blood system, the extracellular pH is kept within a critical range. The functions of the various fetal organ systems, such as central nervous system and the cardiovascular system may be significantly affected by very small changes in pH [19].
Plasma bicarbonate and hemoglobin is the major buffer utilized by the fetus for neutralizing hydrogen ion production. Erythrocytes bicarbonate and inorganic phosphate are also potential buffers, although they play a lesser role in fetal acidbase hemostasis [20]. The respiratory component of the maternal acid-base system shown a progressive fall in arterial CO2 tension and a rise in oxygen tension and in the metabolic elements during pregnancy, there is a parallel reduction in plasma bicarbonate [21]. Experimental studies in animals have shown that excessive hyperventilation causes spasm of placental vessels and slowing of the umbilical circulation with fetal acidosis. Studies has been demonstrated that in cases of obstruction to uteroplacental flow and fetal circulation, maternal oxygen is unlikely to be of value, and in some cases there is increased acidosis.
A number of challenges are associated with the management of preeclampsia through the use of conventional treatment methods; antihypertensives treatment may improve maternal outcome but has potential to be deleterious for the foetus. In most cases, immediate delivery is indicated even if foetus is immature to save the mother’s life. The use of alternatives, including dependence on phytomedicinal preparations have been reported [22]. The aim of this study is to investigate the possibility for improvement of foeto-maternal blood blow. The matrix to be used in accessing success of this intervention is lactate, bicarbonate and nitric oxide levels.
Materials and Methods
Collection and preparation of plant samples
The leaves of the plants were collected, in January of 2019, from First Generation Farms, Iguosula, Uhunmwonde Local Government Area, Edo State. They were identified and verified at Phytomedicine Unit, Department of Plant Biology and Biotechnology, University of Benin. Using a Panasonic® medium kitchen blender, model MX-GX1021WTZ, the plant samples were ground, having been with distilled water, dried for two weeks in the air, and then crushed into powder. Each powder sample weighed 100 g, and the extracts were filtered using whatman filter paper No 42 after being thoroughly extracted for 12 hours by maceration in 200 mL of methanol (125 mm).
Study design
Wistar rats weighing 220-256 g were employed in the study. In the month of May 2019, the animals were housed in the animal house at the department of biochemistry, University of Benin, Benin City. The animals had unrestricted access to a standard meal (20 g of protein, 0.35 g of sodium chloride, and 1.17 g of arginine per 100 g of food), as well as unlimited access to tap water. Before the experiment started, they had a 2 week acclimatization phase.
Induction of preeclampsia
Preeclampsia was induced using the Adriamycin Model, which was employed by Podjarny et al., [23]. Adriamycin (Adriablastina, Abic) was administered to rats at a dose of 3.5 mg/kg IV into the femoral vein while they were under a light ether anesthetic. For four days, the rats were partnered with a reproductive male. On the first day of pregnancy, spermatozoa were discovered in the vaginal smear. Elevated blood pressure and substantial proteinuria confirmed preeclampsia (Table 1).
| Treatments | Parameter | Control | Induced |
|---|---|---|---|
| Blood pressure | |||
| Third trimester | Systolic (mmHg) | 124 | 177 |
| Diastolic (mmHg) | 98 | 121 | |
| Post-partum | Systolic (mmHg) | 121 | 160 |
| Diastolic (mmHg) | 96 | 125 | |
| Proteinuria | |||
| Third trimester | Proteinuria | Negative | +++ |
| Post-partum | Proteinuria | Negative | + |
Table 1: Confirmation of preeclampsia.
The Wistar rat's blood pressure was measured using the CODA® High Throughput System with 2 Activated Channels (CODA-HT2) by Kent Scientific Corporation, USA, according to the non-invasive techniques described by Feng M et al. [24]. A restrainer (CODA System) was used to gently restrain the rats, and the back hatch was changed out to keep the rodents inside. The Wistar rats were placed in their restrainers and allowed five minutes to become used to them before the blood pressure measurement routine started. All of the Wistar rats were going to be tested on the identical CODA system. The Wistar rats benefit from this period of relaxation and warming up, which permits blood flow to the tail. After a 5-minute acclimatization period, the blood pressure-taking procedure is started. The dipstick (combi2) method was used to determine the presence of proteinuria.
Experimental animals
The animals were cared for in accordance with international laboratory animal care and use guidelines. The Wistar rats were divided into fifteen (15) groups of ten (10) rats each, with Group 1 acting as the positive control and Groups 2, 3, and 4 acting as negative controls. There were 5 to 15 preeclamptic groups. Animals in Group 5 received no treatment. Animals in Group 6 were given the standard drug, 100 mg/kg methyl DOPA (Aldomet), while those in Groups 7-15 were given 50, 100, and 200 mg/kg plant extracts. These drugs were administered until the rats received their pops. The extracts were administered once daily.
Twenty four hours after administration of the last dose of the standard drug (100 mg/kg methyldopa) and the extracts to the respective groups, the animals were anaesthetized with chloroform [25].
Processing blood for plasma
Blood sample was collected by cardiac puncture into heparinized bottles. The sample was then centrifuged at 3000 rpm for 5 minutes to obtain clear slightly yellow supernatant plasma.
Determination of lactate, bicarbonate and nitric oxide levels
Lactate was estimated using the colorimetric method using standard kits from fortress diagnostric kits, and following the methods of Buttery JE et al., [26]. Nitric oxide was determined via colorimetry as described by Saad B et al., [27] using the nonenzymatic nitric oxide assay kit. This kit enables users to quantify the total Nitric Oxide (NO) generated for in vitro experimental settings after metallic cadmium converts nitrate to nitrite. This kit is appropriate for measuring total nitric oxide quantitatively in samples with high protein contents. Bicarbonate concentration was estimated using an Automatic Electrolyte Analyzer, model BT-500 Plus. The principle of this instrument is based on the application of a selective membrane of the ion selective electrode, which only allows the desired ion to go in and out.
Ethical issues
The research and ethics committee of the faculty of life sciences, University of Benin, Benin City, granted ethical approval for this study on March 7, 2019, with reference LS19017.
Statistical analysis
Data were analyzed using SPSS version 20 software, and means were separated using least significant differences at 95% probability.
Results
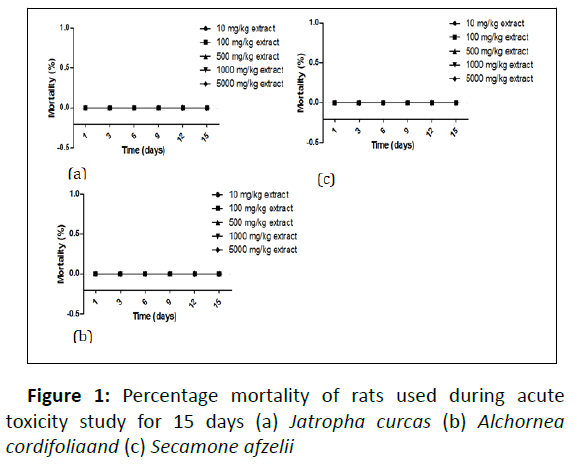
Result as presented in Figure 1 shown percentage mortality of rats used during acute toxicity study for 15 days, this was necessary in other to established that the extracts were not toxic but the extracts were safe to used even at the higher concentrations which was 5000 mg/kg, as presented in Figure 1 no mortality was observed when all extracts were administered to the rats for 15 days.
Results show that for the control nitric oxide was 10.7 units during 3rd trimester this did not significantly deferred from the nitric oxide level during post-partum because the p value was 0.129. However, when the rats where induced with Adriamycin to cause preeclampsia nitric oxide level reduced to 7.5 at 3rd trimester and also reduced to 8.0 in post-partum. Result show that the differences in reduction was significant (p<0.001). However, with the administration of drugs there was a gradual improvement in the nitric oxide level for example when plant were administered with 50 mg/kg of J. curcas, nitric oxide level was 9.4 units at trimester and 9.5 at post-partum but the higher nitric oxide level was obtained when A. cordifolia was administered at the concentration of 100 mg/kg were nitric oxide level was 12.4 at trimester and 10.8 at post-partum.
The effects of extracts on bicarbonate levels during the third trimester and after delivery are shown in Table 2. Both in the third trimester (16.0) and postpartum (15.9), the bicarbonate levels in the control group did not differ significantly from one another (p=0.144). However, the findings demonstrate that preeclampsia episodes considerably decreased bicarbonate levels to 12.9 units in the third trimester and 11.5 units in the postpartum period. However, there were differences in the bicarbonate levels when the induced whister rats were given different doses of plant extracts as compared to when they weren't. For instance, at the third trimester, the bicarbonate level increased to 15.8 units when 50 mg/kg of A. cordifolia were given to preeclampsia rats and 18.3 when 200 mg/kg of the same A. cordifolia were given to preeclampsia rats. However, compared to untreated preeclampsia rats, postpartum increases in bicarbonate level were such that bicarbonate level increased to 12.5 units when 50 mg/kg of J. curcas was administered, 15.7 units when 50 mg/kg of A. cordifolia was administered, and 16.2 units when 200 mg/kg of A. cordifolia was administered. Generally, the result show that the administration of 200 mg/kg extracts B was most effective in enhancing bicarbonate level that was either to reduced preeclampsia. Generally, there were no differences in bicarbonate level taken during 3rd trimester as compared to value taken during post-partum (p>0.5) except in preeclamptic rats treated with 50 mg/kg S. afzelii were bicarbonate level significantly lower at post-partum compared to 3rd trimester even after treatment. Table 3 shows the effects of administering plant extracts on lactate levels during the third trimester and after delivery.
| Treatments | 3rd-trimester | Post-partum | p-value |
|---|---|---|---|
| Control | 10.7 | 12.5 | 0.129 |
| Only Ext-A (No induced PreEc) | 17.3 | 8.2 | <0.001 |
| Only Ext-B (No induced PreEc) | 13.8 | 9.2 | <0.001 |
| Only Ext-C (No induced PreEc) | 15.2 | 14.7 | 0.102 |
| Induced PreEc, no treatment provided | 7.5 | 8 | <0.001 |
| Induced PreEc+100 mg/kg StdD | 7.6 | 11.3 | 0.131 |
| Induced PreEc+50 mg/kg Ext-A | 9.4 | 9.5 | 0.724 |
| Induced PreEc+100 mg/kg Ext-A | 8.5 | 13.6 | <0.001 |
| Induced PreEc+200 mg/kg Ext-A | 7.4 | 10.2 | 0.035 |
| Induced PreEc+50 mg/kg Ext-B | 7.2 | 11.2 | <0.001 |
| Induced PreEc+100 mg/kg Ext-B | 12.4 | 10.8 | 0.238 |
| Induced PreEc+200 mg/kg Ext-B | 11.7 | 9.7 | 0.092 |
| Induced PreEc+50 mg/kg Ext-C | 10.1 | 7.5 | 0.229 |
| Induced PreEc+100 mg/kg Ext-C | 7.8 | 7.9 | 0.628 |
| Induced PreEc+200 mg/kg Ext-C | 8 | 18.7 | <0.001 |
| F-test | 2.456 | 3.393 | - |
| p-value | 0.019 | 0.002 | - |
Table 2: Nitric oxide status at 3rd trimester and post-partum.
| Treatments | Period | p-value | |
|---|---|---|---|
| 3rd trimester | Post-partum | ||
| Control | 16 | 15.9 | 0.144 |
| Only Ext-A (No induced PreEc) | 10.2 | 14.1 | 0.061 |
| Only Ext-B (No induced PreEc) | 16.5 | 12.7 | 0.003 |
| Only Ext-C (No induced PreEc) | 17.1 | 14.6 | 0.026 |
| Induced PreEc, no treatment provided | 12.9 | 11.5 | 0.101 |
| Induced PreEc+100 mg/kg StdD | 13.3 | 13 | 0.525 |
| Induced PreEc+50 mg/kg Ext-A | 14.9 | 12.5 | 0.203 |
| Induced PreEc+100 mg/kg Ext-A | 10.3 | 13.5 | 0.136 |
| Induced PreEc+200 mg/kg Ext-A | 13.5 | 14.2 | 0.322 |
| Induced PreEc+50 mg/kg Ext-B | 15.8 | 15.7 | 0.668 |
| Induced PreEc+100 mg/kg Ext-B | 12.8 | 11.2 | 0.273 |
| Induced PreEc+200 mg/kg Ext-B | 18.3 | 16.2 | 0.098 |
| Induced PreEc+50 mg/kg Ext-C | 16 | 11.4 | 0.032 |
| Induced PreEc+100 mg/kg Ext-C | 14.5 | 13.2 | 0.144 |
| Induced PreEc+200 mg/kg Ext-C | 10.3 | 15.2 | 0.049 |
| F-test | 9.943 | 1.578 | - |
| LSD(0.05) | 2.2 | 3.8 | - |
| p-value | <0.001 | 0.144 | - |
Table 3: Effects of extracts on bicarbonate levels at 3rd trimester and post-partum.
According to Table 3, the lactate level was 34.8 at the third trimester and 35.7 at the postpartum period (p>0.05). Except for when A. cordifolia was supplied to control rats, the administration of the three plant extracts did not result in a significant rise or decrease in lactate level at either the postpartum or third trimester (lactate level decreased from 35.7 to 26.3 units; P=0.015). The delivery of Adriamycin generally resulted in preeclampsia episodes, which significantly raised the lactate level. Generally, the administration of plant extracts irrespective of the concentration caused a reduction in lactate level comparable with the control level, at 3rd trimester (25.5 to 36.4 units) and post-partum (25.9 to 36.0 units). An attempt was made to establish associations between nitric oxide level and bicarbonate level in preeclampsia (Table 4) as well as lactate level (Table 5).
| Treatments | Period | p-value | |
|---|---|---|---|
| 3rd trimester | Post-partum | ||
| Control | 34.8 | 35.7 | 0.132 |
| Only Ext-A (No induced PreEc) | 36.7 | 37.2 | 0.322 |
| Only Ext-B (No induced PreEc) | 35.7 | 26.3 | 0.015 |
| Only Ext-C (No induced PreEc) | 32.2 | 32.8 | 0.726 |
| Induced PreEc, no treatment provided | 55.9 | 40.7 | <0.001 |
| Induced PreEc+100 mg/kg StdD | 35.2 | 32.9 | 0.042 |
| Induced PreEc+50 mg/kg Ext-A | 31.3 | 32 | 0.083 |
| Induced PreEc+100 mg/kg Ext-A | 32.1 | 32.7 | 0.881 |
| Induced PreEc+200 mg/kg Ext-A | 25.6 | 28.9 | 0.138 |
| Induced PreEc+50 mg/kg Ext-B | 34.8 | 31.2 | 0.046 |
| Induced PreEc+100 mg/kg Ext-B | 34.9 | 33.2 | 0.332 |
| Induced PreEc+200 mg/kg Ext-B | 31.1 | 30.4 | 0.715 |
| Induced PreEc+50 mg/kg Ext-C | 34 | 25.9 | <0.001 |
| Induced PreEc+100 mg/kg Ext-C | 25.5 | 28.9 | 0.483 |
| Induced PreEc+200 mg/kg Ext-C | 36.4 | 36 | 0.602 |
| F-test | 3.245 | 0.847 | - |
| LSD(0.05) | 6.4 | 7.3 | - |
| p-value | 0.005 | 0.618 | - |
Table 4: Effects of extracts on lactate levels at 3rd trimester and post-partum.
| Crosstab: 3rd trimester | |||||
|---|---|---|---|---|---|
| Nitric acid | Total | ||||
| Increase | Decrease | ||||
| Lactate | Increase | Count | 1 | 3 | 4 |
| % within lactate | 25.00% | 75.00% | 100.00% | ||
| Decrease | Count | 1 | 6 | 7 | |
| % within lactate | 14.30% | 85.70% | 100.00% | ||
| Total | Count | 2 | 9 | 11 | |
| % within lactate | 18.20% | 81.80% | 100.00% | ||
| Crosstab: Post-partum | |||||
| Nitric acid | Total | ||||
| Increase | Decrease | ||||
| Lactate | Increase | Count | 2 | 0 | 2 |
| % within lactate | 100.00% | 0.00% | 100.00% | ||
| Decrease | Count | 1 | 8 | 9 | |
| % within lactate | 11.10% | 88.90% | 100.00% | ||
| Total | Count | 3 | 8 | 11 | |
| % within lactate | 27.30% | 72.70% | 100.00% | ||
| 3rd trimester, X2=0.196, p=0.038; post-partum; X2=6.519, p=0.011 | |||||
Table 5: Crosstab Nitric oxide levels versus bicarbonate in preeclampsia at 3rd trimester.
In the third trimester, 25% of Wistar rats with rising nitric oxide levels also had rising lactate levels (Table 4). However,during postpartum, all Wistar rats had rising lactate levels in addition to higher nitric oxide levels. However, nitric oxide has a considerable impact on lactate levels both during the third trimester and after delivery, as seen in Table 6.
| Crosstab: 3rd trimester | |||||
|---|---|---|---|---|---|
| Nitric acid | Total | ||||
| Increase | Decrease | ||||
| HCO3 | Increase | Count | 1 | 0 | 1 |
| % within HCO3 | 100.00% | 0.00% | 100.00% | ||
| Decrease | Count | 1 | 9 | 10 | |
| % within HCO3 | 10.00% | 90.00% | 100.00% | ||
| Total | Count | 2 | 9 | 11 | |
| % within HCO3 | 18.20% | 81.80% | 100.00% | ||
| Crosstab: Post-partum | |||||
| Nitric acid | Total | ||||
| Increase | Decrease | ||||
| HCO3 | Increase | Count | 0 | 1 | 1 |
| % within HCO3 | 0.00% | 100.00% | 100.00% | ||
| Decrease | Count | 3 | 7 | 10 | |
| % within HCO3 | 30.00% | 70.00% | 100.00% | ||
| Total | Count | 3 | 8 | 11 | |
| % within HCO3 | 27.30% | 72.70% | 100.00% | ||
| 3rd trimester, X2=4.950, p=0.026; Post-partum; X2=413, p=0.521 | |||||
Table 6: Crosstab Nitric acid levels versus lactate in preeclampsia at 3rd trimester.
Eighty-one percent of wister rats at the third trimester who had lower nitric oxide levels also had lower lactate levels. Similar to this, 72.9 percent of the whister rats that exhibited large drops in nitric oxide levels during postpartum also had significant drops in lactate levels (chi-squared=6.519, p value=0.011).
Discussion
Because of the perception that using medicinal plants to cure illnesses is safe and has no adverse effects, interest in doing so has surged recently. In order to reduce the number of individuals who consume medical plants and the absence of data, it is necessary to undertake toxicity studies on herbal products due to the safety of many medicinal plants. Studies revealed that the acute oral toxicity test is typically the first test to be conducted in order to determine the toxicity of any plants. This is done to determine the adverse effects of either a single dose or an excessive amount of the drugs. Results show that the methanolic plant extracts at 5000 mg/kg body weight were non-toxic because they did not cause any death at that dose. White blood cell count, hemoglobin, packed cell volume, and platelet count are blood parameters that can be used to assess the physiological and pathological status of a person or an animal. The typical range of these parameters may change if poisonous plants are consumed. After 15 days of oral administration of all plant extracts, acute toxicity assessment results showed no significant differences in these parameters were reported compared to control, thus indicating that the extract had no toxic effects. In this study, Jatropha curcas Alchornea cordifolia and Secamone afzelii did not produce any significant changes in biochemical parameters after 15 days of treatment. Previous studied showed that evaluation of liver function is very important when analysis toxicity of drugs on plant extracts because of its relevance for the survival of the organisms.
This study indicates that preeclampsia significantly decreased nitric oxide levels and also decreased bicarbonate levels (Table 1 and 2). One of the first signs of endothelial dysfunction is decreased bioavailability of endothelium-derived nitric oxide, which has been associated with severe vascular diseases. Although there are conflicting reports about nitric oxide levels and preeclampsia, the lower nitric oxide levels seen in whister rats with preeclampsia in our investigation are consistent with the results of some other studies of a similar nature. Contrarily, some studies found preeclampsia to have much higher levels of nitric oxide than normal pregnancy, while others found no difference in nitric oxide levels between preeclampsia and regular pregnancy. Nitric oxide levels were tested in our current investigation, but we also looked at potential variables that might have an impact on nitric oxide generation. Contrarily, the diverse findings of the other studies may be explained by differences in the estimation methodologies for nitric oxide, the gestational age at which nitric oxide was assessed, and the severity of the condition in different study groups. In preeclampsia, the content of cyclic GMP is consistently lower, which suggests that the condition has diminished nitric oxide bioactivity. Nitric oxide levels in preeclampsia were found to be lower. One of the theories for the development of preeclampsia is maternal oxidative stress. However, in the current investigation, nitric oxide levels in the rats that were given Adriamycin to induce preeclampsia decreased to 7.5 at the third trimester and likewise decreased to 8.0 in the postpartum period.
To more easily induce a preeclampsia-like illness in rats and mice, nitric oxide production must be blocked by giving them a nitric oxide synthesis inhibitor. However, in the animal model, this causes nearly all of the preeclampsia symptoms, indicating a direct link between nitric oxide production and the vascular alteration in a normal pregnancy. As shown by our finding, this will indicate a potential decrease in nitric oxide production and nitric oxide synthesis activity in the etiology of preeclampsia.
Nitric oxide generation in humans has been the subject of conflicting study, nevertheless. By examining the concentrations of the two main nitric oxide metabolites, nitrite and nitrate, in the serum or plasma of preeclampsia patients, many studies have attempted to estimate nitric oxide production. According to Mutlu-Turkoglu, preeclamptic patients had lower nitrate levels than pregnant controls.
Conclusion
In general, our study demonstrated that the injection of Adriamycin induced a considerable rise in lactate levels as a result of preeclampsia occurrence. The findings of, which showed that lactate elevation may be caused by increased production, increased clearance, or a combination of both, were correlated with the results. It is known that preeclamptic placentas have higher levels of lactates produced and secreted than other placentas. Additionally, it is well recognized that the liver (which accounts for 70% of lactate clearance) and the kidneys are the main organs involved, and that severe lactate clearance may be compromised in the event that one of these organs is dysfunctional.
References
- Gant NF, Whalley PJ, Everett RB, Worley RJ, MacDonald PC (1987) Control of vascular reactivity in pregnancy. Am J Kidney Dis 9: 303–307.
[crossref], [Google Scholar], [Indexed]
- Myatt L (2006) Placental adaptive responses and fetal programming. J Physiol 572: 25–30.
[crossref],[Google Scholar],[Indexed]
- Krause BJ, Hanson MA, Casanello P (2011) Role of nitric oxide in placental vascular development and function. Placenta 32: 797–805.
[crossref],[Google Scholar],[Indexed]
- Illi B, Colussi C, Grasselli A, Farsetti A, Capogrossi MC et al. (2009) NO sparks off chromatin: Tales of a multifaceted epigenetic regulator. PharmacolTher 123: 344–52.
[crossref],[Google Scholar],[Indexed]
- Suzuki T, Mori C, Yoshikawa H (2009) Changes in nitric oxide production levels and expression of nitric oxide synthase isoforms in the rat uterusduring pregnancy. BiosciBiotechnolBiochem 73: 2163–2166.
[crossref],[Google Scholar],[Indexed]
- Giugliano D, Marfella R, Verrazzo G (1997) The vascular effects of L-Arginine in humans.The role of endogenous insulin J Clin Invest 99: 433.
[crossref],[Google Scholar],[Indexed]
- Tain YL, Huang LT (2011) Asymmetric dimethylarginine: clinical applications in pediatric medicine. J Formos Med Assoc 110: 70–77.
[crossref],[Google Scholar],[Indexed]
- Reynolds LP, Caton JS, Redmer DA, (2006) Evidence for altered placental blood flow and vascularity in compromised pregnancies. J Physiol 572: 51–58.
[crossref],[Google Scholar],[Indexed]
- Nobunaga T, Tokugawa Y, Hashimoto K (1996) Plasma nitric oxide levels in pregnant patients with preeclampsia and essential hypertension. GynecolObstet Invest 41: 189–193.
[crossref],[Google Scholar],[Indexed]
- Jo T, Takauchi Y, Nakajima Y, Fukami K, Kosaka H et al. (1998) Maternal or umbilical venous levels of nitrite/nitrate during pregnancy and at delivery. In Vivo 12:523–6.
- Hodzic J, Izetbegovic S, Muracevic B, Iriskic R, Jovic HS (2017) Nitric oxide biosynthesis during normal pregnancy and pregnancy complicated by preeclampsia. MedicinskiGlasnik (Zenica) 14: 211-217.
[crossref],[Google Scholar],[Indexed]
- Phipps E, Prasanna D, Brima W, Jim B (2016) Preeclampsia: Updates inpathogenesis, definitions, and guidelines. Clinical Journal of the American Society of Nephrology 11: 1102-1113.
- Spracklen CN, RyckmanKK, Triche EW, Saftlas AF (2016) Physical activity during pregnancy and subsequentriskof preeclampsia and gestationalhypertension: A case control study. Matern Child Health J 20: 1193-1202.
[crossref],[Google Scholar],[Indexed]
- Oliveira CA, Brito HL, Bastos MG, Oliveira FG, Casali TG et al. (2014) Depressed cardiac autonomic modulation in patients with chronic kidney disease. Jornal Brasileiro de Nefrologia 36: 155-162.
[crossref],[Google Scholar],[Indexed]
- Granger JP, Alexander BT, Llinas MT, Bennett WA, Khalil RA (2001) Pathophysiology of Hypertension During Preeclampsia Linking Placental Ischemia With Endothelial Dysfunction. Hypertension 38: 718–722.
[crossref],[Google Scholar],[Indexed]
- Darkwa EO, Djagbletey R, Essuman R, Sottie D and Dankwah GB et al. (2018) Nitric Oxide and Pre-Eclampsia: A Comparative Study in Ghana. Maced J Med Sci. 6: 1023-1027.
[crossref],[Google Scholar],[Indexed]
- Davis EF, Lazdam M, Lewandowski AJ, Worton SA, Kelly B et al. (2012) Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: A systematic review. Pediatrics 129: 1552-1561.
[crossref],[Google Scholar],[Indexed]
- Nath AK, Madri JA (2006) The roles of nitric oxide in murine cardiovascular development. Developmental Biology 292: 25-33.
[crossref],[Google Scholar],[Indexed]
- Bobrow CS, Soothill PW (1999) Causes and consequences of fetal acidosis. Arch Dis Child Fetal Neonatal Ed 80: 46-49.
[crossref],[Google Scholar],[Indexed]
- Dunlop W (1999) Normal pregnancy: Physiology and endocrinology. In: Edmonds DK, editor. Dewhurst’s Textbook of Obstetrics and Gynecology for Postgraduates. (6th ed), Blackwell Sciences Ltd, London.
- MacRae DJ (1968) Maternal influence on foetal acid-base balance. Proc R Soc Med 61: 490-491.
- Atoe K, Idu M, Ikhajiagbe B, Bakre AG (2021) Lipid Ratios in Adriamycin-induced Pre-eclamptic Wistar Rats Exposed to Methanolic Plant Extracts. J Appl Sci Environ Manage 25: 1617-1623.
[crossref],[Google Scholar],[Indexed]
- Podjarny E, Bernheim JL, Rathaus M, Pomeranz A, Tobvin D et al. (1992) Adriamycin nephropathy: A model to study the effects of pregnancy on renal disease in rat. Am J Physiol 263: F711-5.
[crossref],[Google Scholar],[Indexed]
- Feng M, DiPetrillo K (2009) Non-invasive Blood Pressure Measurement in Mice. Methods Mol Biol 573: 45-55.
[crossref],[Google Scholar],[Indexed]
- Rowell TE (1977) Reproductive cycle of the talapoin monkey (Miopithecus talapoin) Folia Primatol 28: 188-202.
[crossref],[Google Scholar],[Indexed]
- Buttery JE, Pannall PR (1987) Colorimetric measurement of D(-)lactate in plasma. Clinical Biochemistry 20: 237–239.
[crossref],[Google Scholar],[Indexed]
- Saad B, Azaizeh H, Abu-Hijleh G (2006) Safety of traditional Arab herbal medicine. Evid Based Complement Alternat Med 3: 433-439.
[crossref],[Google Scholar],[Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences