ISSN : 2576-3911
Integrative Journal of Global Health
Say Goodbye, Conquering Hypoglycaemia in Diabetes
Mohanty Bijaya*, Moharatha Harapriya and Prasad Satish
Department of Medicine, Tata Main Hospital, Jamshedpur, Jharkhand, India
- *Corresponding Author:
- Mohanty Bijaya
Department of Medicine, Tata Main
Hospital, Jamshedpur, Jharkhand, India.
Tel: +917763807140
E-mail: bijayamohantytmh@gmail.com
Received Date: May 09, 2017; Accepted Date: May 17, 2017; Published Date: May 20, 2017
Citation: Bijaya M, Harapriya M, Satish P. Say Goodbye, Conquering Hypoglycaemia in Diabetes. Integr J Glob Health. 2017, 1:2.
Abstract
Introduction: Hypoglycaemia is a clinical syndrome with diverse aetiology. In diabetes, it is defined as all episodes of low plasma glucose with or without symptoms that expose the individual to harm. Over decades a variety of criteria have been used to define hypoglycaemia. However according to ADA 2016 guidelines it is defined as a blood glucose level less than 70 mg/dl or 3.88 mmol/l. It is a medical emergency that requires prompt recognition and treatment to prevent organ and brain damage. During the course of diabetes, it is reported that 1 out of 4 patients are at risk of developing hypoglycaemia. In the hospital setting, up to 26% of patients have been reported having hypoglycaemic events which not only increases hospital stay but also increases the risk of morbidity and mortality in the face of reduced quality of life and increased cost.
Materials and Methods: This study was conducted in Tata Main Hospital, Jamshedpur to evaluate the clinical spectrum and burden of hypoglycaemia in patients with diabetes mellitus and to implement adequate control and prevention measures. This is a prospective study. 200 cases of hypoglycaemia of both sex was taken in to the study design. Diagnosis is based on history, clinical examination and level of random blood sugar as per ADA guidelines-2016. Hypoglycaemia due to other causes, patients with plasmodium falciparum malaria fulminant hepatitis, sepsis and multi organ failure were excluded from the study. Detailed history was taken in all cases including drug history, dietary habits and history of any recent illnesses like fever, vomiting diarrhoea etc. The clinical presentation, laboratory parameters, precipitating factor for hypoglycaemic event was recorded and analysed in all cases. Corrective measures were taken in each of them and preventive measures designed to decrease the frequency of hypoglycaemia in diabetic patients.
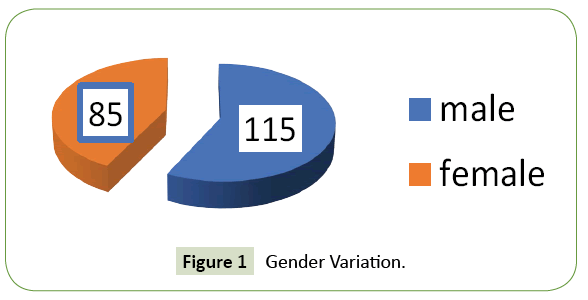
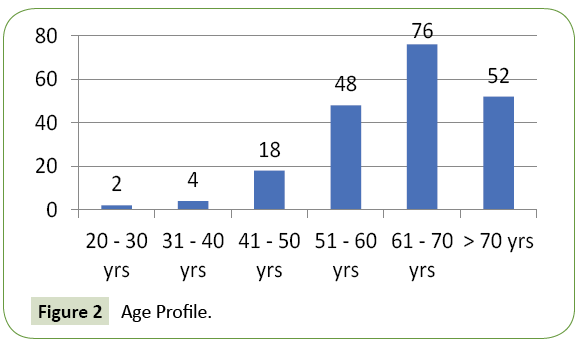
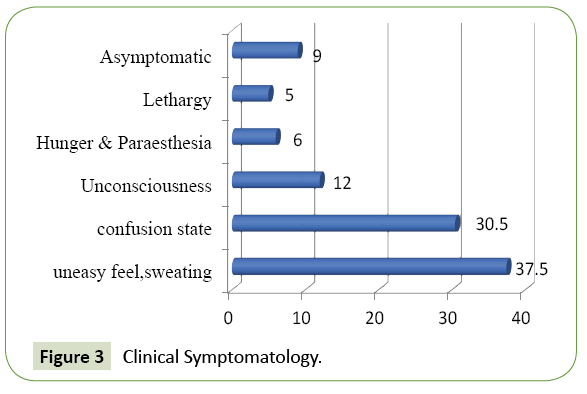
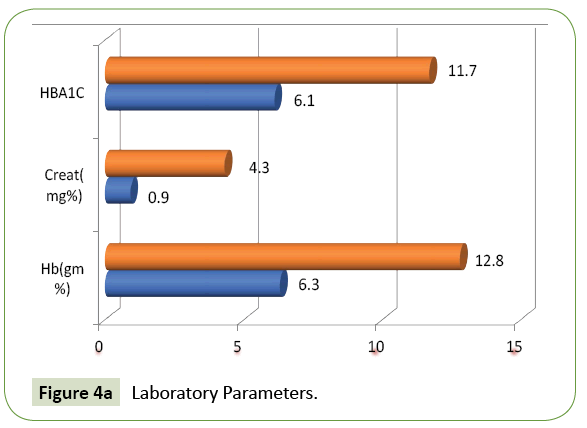
Observation: Out of 780 patients of diabetes mellitus admitted to our hospital during the study period 200 cases had hypoglycaemia on admission. Their age varied from 20 to 83 years. 115 cases were male and 85 were female. The frequency rate of hypoglycaemia in our study was 25.64%. 192 patients had type 2 DM and six patients had type 1 DM. 87.5% of cases presented with feeling of uneasiness and sweating, 30.5% were admitted in a state of confusion. Twenty-four cases were unconscious at the time of admission. 9% of cases were asymptomatic. Glycosylated haemoglobin varied from 6.1 to 11.7% showing that both controlled and uncontrolled cases are at risk of developing hypoglycaemia. Renal insufficiency was found in 48% of patients. Majority (42%) of our cases had their blood sugar between 31-40 mg/dl. Blood sugar level was less than 20 mg/dl in 8 cases. Average plasma glucose at the time of admission was 41 mg/dl the lowest value documented was 17 mg/dl. 39% of cases were on combination therapy with insulin and oral diabetic drugs, 30% were on oral drugs and 28% were only on injection insulin during hypoglycaemic event. 48% of patients had a history of low oral intake prior to hypoglycaemic episode and 9% had history of acute illness before the event. Six patients had history of alcohol intake. Medication error was the key factor causing hypoglycaemia in three patients. Sulfonylurea agents were associated with higher rates of hypoglycaemia than other oral diabetic drugs. All of them were treated with IV dextrose, IV glucagon and oral glucose depending on the case and improved. However, 46 cases (23%) had second episodes of hypoglycaemia and 22 (11%) patients had more than two episodes of hypoglycaemia. Their hospital stay varied between 2-5 days with an average stay of 4.6 days. 99% of cases improved and discharged. But two patients expired probably due to prolonged hypoglycaemic encephalopathy leading to permanent brain damage. Their random blood sugar was less than 20 mg/dl on admission.
Conclusion: Despite limitations of our study we conclude that hypoglycaemia is a common complication in diabetes causing serious harm which needs to be addressed at a war foot basis. It is not only important to identify and treat the condition but also to prevent hypoglycaemic events. We can achieve lowering hypoglycaemic events by individualizing glycemic goals, addressing the risk factors and high risk patients and educating the patients along with their care givers.
Keywords
Diabetes mellitus; Hypoglycaemia; Health education; Risk factors; Oral diabetic drugs; Insulin
Introduction
Hypoglycaemia is one of the most feared complication of diabetes management. Attempts made at intensive glycaemic control increases the risk of hypoglycaemia. A six-fold death due to diabetes is attributed to patients experiencing severe hypoglycaemia in comparison to patients who did not had it. This diabetes related hypoglycaemic episodes precipitate cerebrovascular accidents, acute myocardial infarction and other health related quality of life issues like sleep, travel and employment etc. It is a clinical syndrome with varied aetiology. In diabetes, it is defined as all episodes of low plasma glucose with or without symptoms that expose the individual to harm. Over decades, a variety of criteria have been used to define hypoglycaemia. An early, very practical, and widely accepted definition of hypoglycaemia is the presence of classical Whipple's triad that is decreased plasma glucose concentration, symptoms compatible with hypoglycaemia and rapid attenuation of those symptoms by correction of the low glucose. A single threshold value for plasma glucose concentration that defines hypoglycaemia in diabetes cannot be assigned because glycaemic thresholds for symptoms of hypoglycaemia varies on individual basis. Nonetheless an alert value is defined as random blood sugar concentration ≤ 70 mg/dL (≤ 3.9 mmol/L)) that draws the attention of both patients and caregivers to the potential harm associated with hypoglycaemia. The American Diabetes Association (ADA) work group on hypoglycaemia in June 2004 classified of hypoglycaemia in diabetes in to five categories which are as follows.
Severe hypoglycaemia
Severe hypoglycaemia is an event requiring assistance of another person to actively administer carbohydrates, glucagon, or take other corrective actions. Plasma glucose concentrations may not be available during an event, but neurological recovery following the return of plasma glucose to normal is considered sufficient evidence that the event was induced by a low plasma glucose concentration.
Documented symptomatic hypoglycaemia
Documented symptomatic hypoglycemia is an event during which typical symptoms of hypoglycemia are accompanied by a measured plasma glucose concentration ≤ 70 mg/dL (≤ 3.9 mmol/L).
Asymptomatic hypoglycaemia
Asymptomatic hypoglycaemia is an event not accompanied by typical symptoms of hypoglycaemia but with a measured plasma glucose concentration ≤ 70 mg/dL (≤ 3.9 mmol/L).
Probable symptomatic hypoglycaemia
Probable symptomatic hypoglycaemia is an event during which symptoms typical of hypoglycaemia are not accompanied by a plasma glucose determination but that was presumably caused by a plasma glucose concentration ≤ 70 mg/dL (≤ 3.9 mmol/L).
Pseudo/relative hypoglycaemia
Pseudo-hypoglycaemia is an event during which the person with diabetes reports any of the typical symptoms of hypoglycaemia with a measured plasma glucose concentration >70 mg/dL (>3.9 mmol/L) but approaching that level.
To make it simpler ADA 2016 guidelines define hypoglycaemia as a blood glucose level less than 70 mg/dL or 3.88 mmol/l which is a true medical emergency that requires prompt recognition and treatment to prevent organ and brain damage. During the course of diabetes, it is reported that 1 out of 4 patients are at risk of developing hypoglycaemia. In the hospital setting up to 26% of patients have been reported to experience hypoglycaemia which can increase the hospital stay and the risk of mortality at the face of increasing cost and decrease quality of life. Hypoglycaemia is considered to be a barrier in the optimal control of diabetes for both indoor patient and outpatients. Insulin therapy is frequently used in the management of diabetes for the inpatient population and standard insulin regimens like pre-prandial bolus insulin and basal insulin at night are reported to contribute to iatrogenic hypoglycaemia. Other risk factors that increase the risk of hypoglycaemia among diabetic patients include inadequate food intake secondary to dyspepsia, loss of appetite, in anticipation of surgery or other procedures, use of standard corrective insulin doses, etc. Hypoglycaemia can manifest as neuroglycopenic or the neurogenic/adrenergic manifestations. Neuroglycopenic manifestation are due to direct result of CNS glucose deprivation and the symptoms include weakness, tiredness, dizziness, inappropriate behaviour, difficulty with concentration, confusion, blurred vision and in extreme cases coma and even death occurs if it is severe and prolonged. Adrenergic manifestations are due to CNS mediated sympathoadrenal activation, symptoms of which include sweating, shakiness, palpitation, anxiety, a sensation of hunger and paraesthesia.
Aim of Study
With this back ground, we have undertaken this study in our hospital to examine the clinical spectrum and burden of hypoglycaemia in diabetic patients and to implement adequate control measures.
Materials and Methods
This is a prospective study conducted in Tata Main Hospital, a teaching institute and a secondary care hospital catering to both rural and urban population of Jharkhand, part of Odisha, West Bengal and Bihar for a period of six months from April to December 2016. Written consent was taken from each patient/ relative and studied according to proforma. Approval of Ethics committee of Tata Main Hospital, Jamshedpur was taken. 200 cases of hypoglycaemia of both gender was taken in to the study design. Diagnosis is based on history, clinical examination and level of random blood sugar as per ADA guidelines-2016.
Inclusion criteria
Patients of Diabetes Mellitus admitted with random blood sugar <= 70 mg% (ADA Guideline 2016).
Exclusion criteria
Hypoglycaemia due to other causes like patients with Plasmodium falciparum malaria, Fulminant hepatitis, Sepsis, Multi organ failure were excluded from the study.
Detailed history was taken in all cases. Particular attention was given about the drugs used, type of insulin, the dosage, the diet pattern and history of any recent illnesses like fever, vomiting, diarrhoea etc. Thorough clinical evaluation done. Clinical signs and symptoms were recorded and analysed. Laboratory parameters like complete blood picture, HBA1C (Glycosylated haemoglobin), serum creatinine and electrolyte was recorded in all and analysed. The precipitating factor for hypoglycaemic event was recorded and analysed in different age groups. Corrective measures were taken in each of them. Increased awareness was created among the patients and their relatives including the care givers. An intervention protocol was designed to decrease the frequency of hypoglycaemia in both inpatient and outdoor patients.
Observation
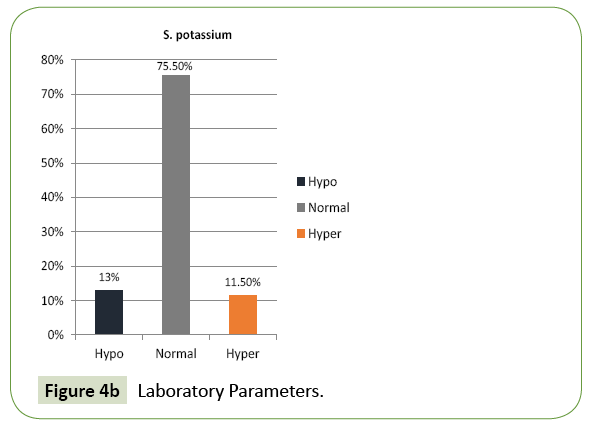
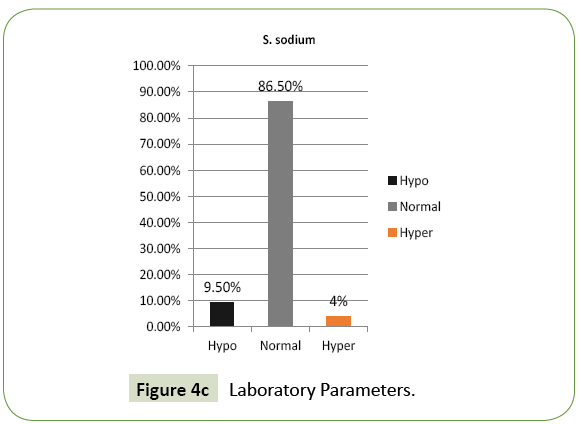
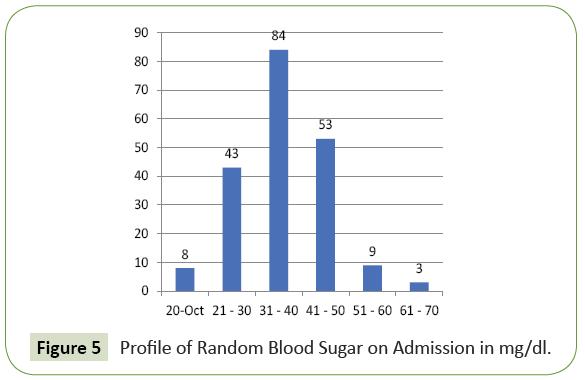
780 patients of diabetes mellitus were admitted to our hospital during the study period out of which 200 cases had hypoglycaemia on admission. Their age varied from 20 to 83 years. 38% of patients were in the age group of 61 to 70 years and 26% of patients were above 70 years. 88% of cases in our study group were above 50 years (Figure 2). 115 were male and 85 were female (Figure 1). The frequency rate of hypoglycaemia among our inpatient was 25.64%. 192 patients had type 2 DM and the rest six patients had type 1 DM. 87.5% of cases presented with feeling of uneasiness and sweating, 30.5% were admitted in a state of confusion. Twenty-four cases were unconscious at the time of admission. 9% of cases were asymptomatic (Figure 3). Severity of symptoms were associated with the degree of hypoglycaemia. Glycosylated haemoglobin varied from 6.1 to 11.7% showing that both controlled and uncontrolled case is at risk of developing hypoglycaemia. Serum creatinine value varied from 0.9 to 4.3 mg% (Figure 4A). Renal insufficiency was found in 48% of patients. 13% of patients presented with hypokalaemia, 11.5% with hyperkalaemia and the rest had normal potassium value. 9.5% of our cases had hyponatremia indicating low oral intake and fluid loss (Figures 4B and 4C). Majority (42%) of our cases had their blood sugar between 31-40 mg/dl. Blood sugar level was less than 20 mg/dl in 8 cases (Figure 5).
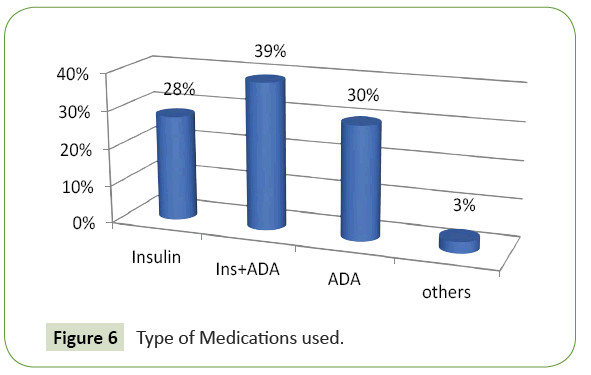
Average plasma glucose at the time of admission was 41 mg/dl, the lowest value documented was 17 mg/dl. 39% of cases were on combination therapy with insulin and oral diabetic drugs, 30% were on oral drugs and 28% were on only injection insulin during hypoglycaemic event (Figure 6). 48% of patients had a history of low oral intake prior to hypoglycaemic episode and 9% had history of acute illness before the event. Six patients had history of alcohol intake. Hypoglycaemia was attributed to medication error in three patients. They had increased the dose of medication without consulting their physician. Out of all sulfonylurea agents were associated with higher rates of hypoglycaemia than other oral diabetic drugs particularly metformin, thiazolidinediones, alpha glucosidase inhibitors and Dipeptidyl peptidase-4 (DPP-4) inhibitors.
All of them were treated with IV dextrose, IV glucagon and oral glucose depending on their clinical presentation. They improved and had documented euglycaemia within two hours of treatment. However, 46 cases (23%) had second episodes of hypoglycaemia and 22 (11%) patients had more than two episodes of hypoglycaemia. Their hospital stay varied between 2-5 days with an average stay of 4.6 days. Out of two hundred cases one hundred ninety-eight patients (99%) improved and got discharged. But two patients expired probably due to hypoglycaemic encephalopathy leading to permanent brain damage. They were admitted in an unconscious state with random blood sugar less than 20 mg/dl and there was a delay in seeking medical help by the family members.
Discussion
Hypoglycaemia is a common cause for hospital admission among diabetic population. According to Mustafa and Choudhary one out of four diabetic inpatients may experience hypoglycemia [1,2], which is reported to be a neglected complication of diabetes with multiple negative implications [3]. These implications include increased sympathoadrenal response, neurocognitive changes, endothelial dysfunction, and blood coagulation abnormalities [3]. These changes underscore the importance of hypoglycemia, as a common complication of diabetes care.
The frequency rate of hypoglycaemia among diabetic patients in our series is 25.64% which is in the range reported in the literature. Two out of three patients (66.6%) who were reported to have hypoglycaemia, have a blood glucose less than 50 mg/ dL (2.77 mmol/l). In our study, we had 94% of cases having blood sugar less than 50 mg/dl. Interplay of relative or absolute insulin excess and compromised glucose counter-regulation in type 1 diabetes and advanced type 2 diabetes results in hypoglycaemia. Several factors put individuals at risk for a hypoglycaemic episode. The conventional risk factors are excessive dosage, ill-timed, or of the wrong type of Insulin, insulin secretagogue or sensitizer. Decreased delivery of exogenous glucose as after missed meals and during overnight fast, decrease endogenous glucose production as occurs after alcohol ingestion. Increased glucose utilization during exercise, in the middle of the night, and after weight loss, or improved glycaemic control, or during treatment with an insulin sensitizer and decrease Insulin clearance as with progressive renal failure are among other conventional risk factors of hypoglycaemia. Discordance between insulin administration and food intake [4] is one of the most important risk factors for drug-induced hypoglycaemia which is responsible for 48% of hypoglycaemic events in our series. 48% of our cases had features of renal insufficiency at the time of presentation and 3% had history of alcohol intake. This is similar to Maynard et al. study, showing that inadequate food intake without adjustment of insulin dosage can be the most important risk factor for iatrogenic hypoglycaemia [5]. Nutritional interruption that we have encountered among our diabetic population are nausea, vomiting and presence of gastroparesis. Gastroparesis or diabetic stomach is particularly common in elderly patients with a long history of diabetes with multiple micro and macrovascular complications. Gastroparesis is known to increase the risk of hypoglycaemia [5-9]. Other risk factors include history of severe hypoglycaemia, hypoglycaemia unawareness, or both. In one study 84% of patients with an episode of severe hypoglycemia (<40 mg/dL [2.2 mmol/L]) had a prior episode of hypoglycemia (<70 mg/dL [3.9 mmol/L]) during the same admission. We had 23% of cases in our series who had second episode of hypoglycaemia and 11% had more than two hypoglycaemic events in the same admission.
Attempting aggressive glycaemic therapy per se as evidenced by lower HbA1C levels lead to more hypoglycaemic events particularly in elderly patients. Concomitant medications with aspirin, sulfonamides, warfarin, fibrates, allopurinol, nonsteroidal anti-inflammatory drugs and angiotensin converting enzyme inhibitors can increase the potential of sulfonylureas to cause hypoglycemia by displacement from albumin-binding sites, by decreasing hepatic metabolism, decreased renal excretion or stimulation of insulin secretion and increase peripheral glucose uptake. Morning administration of basal insulin and the administration of bolus insulin postprandial helps to reduce the inpatient hypoglycemia, particularly for patients who may experience unexpected nutritional interruption/discordance. Maynard showed that use of bolus insulin postprandial was beneficial in preventing hypoglycemia due to nutritional interruption or the discordance between insulin administration and food intake. The decrease in standard doses of corrective insulin may also have a beneficial effect in reducing the risk of hypoglycaemic events. Administration of the shortacting/bolus insulin in the postprandial period was reported to reduce this risk [10-12]. The elimination of the high-dose insulin correction scales from the insulin order sets was reported by Pasala et al. to help decrease the incidence of inpatient hypoglycemia [13]. To manage diabetes safely it is essential to address this preventable complication. There is urgency to recognize it, to treat it, and especially to prevent it. Documentation of hypoglycemia is very important to promote patient safety in the management of diabetes. At our hospital, we document hypoglycemic events and report as errors in indoor patients which represents a voluntary reporting system. This is done by the nursing staff and doctors. Analysis of these events done in a regular basis.
Physicians need to address the issue of hypoglycemia during every patient visit and educating the patient along with the care givers. Frequent Self-Monitoring Blood Glucose (SMBG) is a simple and effective tool that can help achieve the balance between adequate glycemic control and reduced risk of hypoglycaemia is grossly underutilized in India. The proportion of patients with diabetes in India who own a blood glucose testing meter has been reported to be 1.8% Bjork et al. and 0.2% by Mohan et al. [14,15]. Glycemic goals needs to be individualized. ADA now suggests that less-stringent HbA1C goals (such as <8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced micro-vascular or macrovascular complications, extensive co-morbid conditions, and those with longstanding diabetes in whom the general goal is difficult to attain (level of evidence B) [16-20]. Although several newer-generation therapies and treatment strategies for type 2 diabetes have a lower risk of hypoglycemia than established agents, long-term safety data are currently lacking [21-26]. Thus, choice of therapy is important, with hypoglycemic risk varying according to drug selection [27-35].
Conclusion
Hypoglycaemia is a common yet neglected complication in diabetes causing serious harm specially in safety sensitive jobs which needs to be addressed at a war foot basis [36- 42]. Recognition, prevention, and proactive management of hypoglycemia in patients with diabetes must be given top priority. Prevention of hypoglycemia is possible by individualizing the glycemic goals, addressing the risk factors and high risk patients of hypoglycaemia and education of patients along with the care givers [44]. The role of educational programs in preventing hypoglycaemia has been emphasized in several studies [45- 48]. Let us hope that time for a new era begins with the aim to conquer the hypoglycaemic fight and bidding Good Bye to this complication.
References
- Mustafa OG, Choudhary P (2014) Hypoglycaemia in hospital: a preventable killer? Diabet Med 31: 1151-1152.
- Kalra S, Mukherjee JJ, Venkataraman S, Bantwal G, Shaikh S, et al. (2013) Hypoglycemia: The neglected complication. Indian J EndocrinolMetab 17: 819-834.
- Maynard GA, Huynh MP, Renvall M (2008) Iatrogenic Inpatient Hypoglycemia: Risk Factors, Treatment, and Prevention Analysis of Current Practice at an Academic Medical Centerwith Implications for Improvement Efforts. Diabetes Spect 4: 241-247.
- Nirantharakumar K, Marshall T, Kennedy A, Narendran P, Hemming K, et al. (2012) Hypoglycaemia is associated with increased length of stay and mortality in people with diabetes who are hospitalized. Diabet Med 29: e445-448.
- Shafiee G, Mohajeri-Tehrani M, Pajouhi M, Larijani B (2012) The importance of hypoglycemia in diabetic patients. J Diabetes MetabDisord 11: 17.
- Nowak TV, Johnson CP, Kalbfleisch JH, Roza AM, Wood CM, et al. (1995) Highly variable gastric emptying in patients with insulin dependent diabetes mellitus. Gut 37: 23-29.
- Horowitz M, Harding PE, Maddox AF, Wishart JM, Akkermans LM, et al. (1989) Gastric and oesophageal emptying in patients with type 2 (noninsulin- dependent) diabetes mellitus. Diabetologia 32: 151-159.
- Horowitz M, Harding PE, Maddox AF, Wishart JM, Akkermans LM, et al. (1989) Gastric and oesophageal emptying in patients with type 2 (noninsulin- dependent) diabetes mellitus. Diabetologia 32: 151-159.
- Koch KL (1999) Diabetic gastropathy: gastric neuromuscular dysfunction in diabetes mellitus: a review of symptoms, pathophysiology, and treatment. Dig Dis Sci 44: 1061-1075.
- McCall AL (2012) Insulin therapy and hypoglycaemia. EndocrinolMetabClin North Am 41: 57-87.
- Zammitt NN, Frier BM (2005) Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care 28: 2948-2961.
- UK Hypoglycemia Study Group (2007) Risk of hypoglycemia in type 1 and type 2 diabtes; effects of treatment modalities and their duration. Diabetologia 50: 1140-1157.
- Pasala S, Dendy JA, Chockalingam V, Meadows RY (2013) An inpatient hypoglycemia committee: development, successful implementation, and impact on patient safety. Ochsner J 13: 407-412.
- KapurA, KingH, NairJ, RamachandranA (2003) Health policy, 2003-Global policy aspects of diabetes in India Elsevier.
- MohanV, SandeepS, DeepaR(2007) Epidemiology of type 2 diabetes: Indian scenario Indian JMed Res 125:217-230.
- Childs BP, Grothe JM, Greenleaf PJ (2012) Strategies to Limit the Effect of Hypoglycaemia on Diabetes Control: Identifying and Reducing the Risks. Clin Diabetes 30: 28-33.
- Shafiee G, Mohajeri-Tehrani M, Pajouhi M, Larijani B (2012) The importance of hypoglycemia in diabetic patients. J Diabetes MetabDisord 11: 17.
- UK Hypoglycemia Study Group (2007) Risk of hypoglycemia in type 1 and type 2 diabtes; effects of treatment modalities and their duration. Diabetologia 50: 1140-1157.
- Nirantharakumar K, Marshall T, Kennedy A, Narendran P, Hemming K, et al. (2012) Hypoglycaemia is associated with increased length of stay and mortality in people with diabetes who are hospitalized. Diabet Med 29: e445-448.
- McCall AL (2012) Insulin therapy and hypoglycemia. EndocrinolMetabClin North Am 41: 57-87.
- Cryer PE, Davis SN, Shamoon H (2003) Hypoglycemia in diabetes. Diabetes Care 26: 1902-1912.
- Zammitt NN, Frier BM (2005) Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care 28: 2948-2961.
- Tomky D (2005) Detection, Prevention, and Treatment of Hypoglycemia in the Hospital. Diabetes Spectrum 18: 39-44.
- Rajendran R, Rayman G (2014) Serious harm from inpatient hypoglycaemia: a survey of hospitals in the UK. Diabet Med 31: 1218-1221.
- Vue HM, Setter SM (2011) Drug-induced glucose alterations part 1: druginducedhypoglycemia. Diabetes Spect 24: 171-177.
- Shaw SJ, Bughi S (2010) Drug errors involving glucose-lowering agents. EndocrPract 16: 134-135.
- The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 352: 837-853.
- American Diabetes Association (2013) Standards of medical care in diabetes-2013. Diabetes Care 36:S11-66.
- Kim JT, Oh TJ, Lee YA, Bae JH, Kim HJ, et al. (2011) Increasing trend in the number of severe hypoglycemia patients in Korea. Diabetes Metab J 35:166-172.
- Noh RM, Graveling AJ, Frier BM (2011) Medically minimising the impact of hypoglycemia in type 2 diabetes: A review. Expert OpinPharmacother12:2161-2175.
- Akram K, Pedersen-Bjergaard U, Carstensen B, Borch-Johnsen K, Thorsteinsson B (2006) Frequency and risk factors of severe hypoglycaemia in insulin-treated Type 2 diabetes: A cross-sectional survey. Diabet Med 23:750-756.
- Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, et al. (2003) Frequency of severe hypoglycaemia requiring emergency treatment in type 1 and type 2 diabetes: A population based study of health service resource use. Diabetes Care 26:1176-1180.
- Pedersen-Bjergaard U, Pramming S, Heller SR, Wallace TM, Rasmussen AK, et al. (2004) Severe hypoglycaemia in 1076 adult patients with type 1 diabetes: Influence of risk markers and selection. Diabetes Metab Res Rev 20:479-486.
- Pramming S, Thorsteinsson B, Bendtson I, Binder C (1991) Symptomatic hypoglycaemia in 411 type 1 diabetic patients. Diabet Med8:217-222.
- Lundkvist J, Berne C, Bolinder B, Jonsson L (2005) The economic and quality of life impact of hypoglycemia. Eur J Health Econ 6: 197-202.
- Jonsson L, Bolinder B, Lundkvist J (2006) Cost of hypoglycemia in patients with type 2 diabetes in Sweden. Value Health 9:193-198.
- Allicar MP, Megas F, Houzard S, Baroux A, Thai F, et al. (2000) Frequency and costs of hospital stays for hypoglycemia in France in 1995. In French.Presse Med 29:657-661.
- Holstein A, Plaschke A, Egberts EH (2002) Incidence and costs of severe hypoglycemia. Diabetes Care25:2109-2110.
- American Diabetes Association Workgroup on Hypoglycemia (2005) Defining and reporting hypoglycemia in diabetes. Diabetes Care 28:1245-1249.
- Shafiee G, Mohajeri-Tehrani M, Pajouhi M, Larijani B (2012) The importance of hypoglycemia in diabetic patients. J Diabetes MetabDisord 11:17.
- Kalra S (2013) Geriatric diabetes. J Pak Med Assoc 63:403-405.
- McAulay V, Deary IJ, Frier BM (2001) Symptoms of hypoglycemia in people with diabetes. Diabet Med 18:690-705.
- Williams SA, Pollack MF, Dibonaventura M (2011) Effects of hypoglycemia on health-related quality of life, treatment satisfaction and healthcare resource utilization in patients with type 2 diabetes mellitus. Diabetes Res ClinPract 91:363-370.
- Unger J, Parkin C (2011) Recognition, prevention, and proactive management of hypoglycemia in patients with type 1 diabetes mellitus. Postgrad Med 123:71-80.
- Lee SM, Koh D, Chui WK, Sum CF (2011) Diabetes management and hypoglycemia in safety sensitive jobs. Saf Health Work. 2: 9-16.
- van Staa T, Abenhaim L, Monette J (1997) Rates of hypoglycemia in users of sulfonylureas. J ClinEpidemiol 50:735-741.
- Tomky D (2005) Detection, prevention, and treatment of hypoglycemia in the hospital. Diabetes Spectr 18:39-44.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences