Risk and Readiness Assessment of Border Districts to Respond to Plague in West Nile Region, Uganda, August 2021
Immaculate Atuhaire1*, Doreen N Gonahasa1, Sandra Nabatanzi2, Benon Kwesiga1, Daniel Kadobera1, Bob O Amodan1, Ignatius Wadunde1, Andrew Kwiringira1, Shaban Senyange1, Patience Mwine1, Edirisa J Nsubuga1, Hildah T Nansikombi1, Sherry R Ahirirwe1, Linda Atiku3, Titus Apangu3, John Opolot4, Felix Ocom5, Musa Sekamatte6, Maureen Nabatanzi7, Lilian Bulage1 and Alex R Ario1,4
1Department of Microbiology, National Institute of Public Health, Kampala, Uganda
2Department of Microbiology, US Centre for Disease Control and Prevention, Kampala, Uganda
3Department of Microbiology, Uganda Virus Research Institute, Entebbe, Uganda
4Department of Microbiology, Veterinary Public Health, Ministry of Health, Kampala, Uganda
5Department of Microbiology, National Public Health Emergency Operations Center, Ministry of Health, Kampala, Uganda
6Department of Microbiology, National One Health Platform, Ministry of Health, Kampala, Uganda
7Department of Microbiology, Infectious Diseases Institute, Kampala, Uganda
- *Corresponding Author:
- Immaculate Atuhaire
Department of Microbiology,
National Institute of Public Health,
Kampala,
Uganda,
Tel: 0777816066;
E-mail: atuhaire@musph.ac.ug
Received date: May 16, 2023, Manuscript No. IPJZDPH-23-16664; Editor assigned date: May 19, 2023, PreQC No. IPJZDPH-23-16664 (PQ); Reviewed date: June 02, 2023, QC No. IPJZDPH-23-16664; Revised date: July 17, 2023, Manuscript No. IPJZDPH-23-16664 (R); Published date: July 24, 2023, DOI: 10.36648/IPJZDPH.07.1.002
Citation: Atuhaire I, Gonahasa DN, Nabatanzi S, Kwesiga B, Kadobera D, et al. (2023) Risk and Readiness Assessment of Border Districts to Respond to Plague in West Nile Region, Uganda, August 2021. J Zoonotic Dis Public Health Vol:7 No:1
Abstract
Background: Ituri province in the Democratic Republic of Congo (DRC) is a hotspot for plague, with occasional crossing of case patients into Uganda. As of June 2021, 117 cases of plague were reported in Ituri province, DRC. In August 2021, we evaluated the risk of plague importation into West Nile region of Uganda and assessed the level of preparedness to respond.
Methods: We used the population connectivity across borders toolkit to assess the risk of plague introduction in 6 West Nile districts and one city. We categorized risk in districts based on previous cases, volume of cross border movements and proximity to the outbreak epicenter in DRC. We assessed districts preparedness to respond using an adapted WHO checklist and Ready score criteria (scores <40%=not prepared). We assessed 47 health facilities across the study area for response readiness in terms of healthcare worker training, availability of standard operating procedures, and training of village health teams.
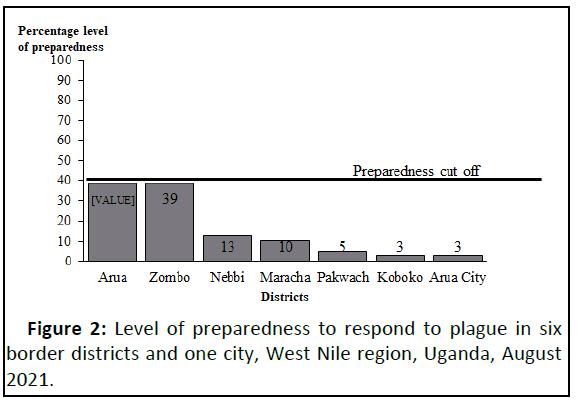
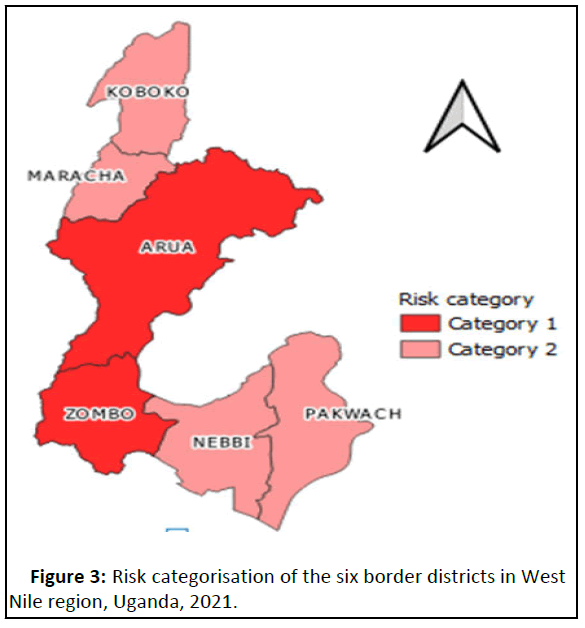
Results: Two districts (Arua and Zombo) in West Nile were in the highest risk category for plague importation. All districts scored as ‘not prepared’, although Zombo and Arua scored higher (both 39%) than other districts. Of 47 health facilities assessed, 21 were ‘not ready’, and no facility was ‘prepared’. Only ten health facilities had staff who had been trained in plague related activities.
Conclusion: No district or health facilities in the area assessed were prepared to respond to potential plague importation. The risk of importation was high, especially in Arua and Zombo districts. Arua and Zombo districts should be prioritized for preparedness activities for a potential plague outbreak. This study emphasizes the need for continued efforts to improve preparedness and response to plague outbreaks in Uganda, particularly in border districts with high population movement.
Keywords
Plague; Cross border; Preparedness; Uganda; Emphasizes
Abbreviations:
FGDs: Focus Group Discussions; KII: Key Informant Interviews; IEC: Information Education and Communication; POBCAB: Population Connectivity Across Borders; DHT: District Health Team
Introduction
Focusing on communicable disease preparedness and response in districts with international borders and population connectivity across these borders is important in halting international disease spread. Plague has become endemic in the West Nile Region of Uganda particularly in Arua and Zombo districts. Seventy eight (78) plague cases were identified during 2008-2016 and this is partially attributed to porous borders that have made it possible for importation of communicable diseases from the Democratic Republic of Congo (DRC) [1]. The last incidence of plague in the region occurred in 2019 when two human plague cases including one fatality occurred following importation from neighbouring DRC were reported [2].
Fataki health zone in DRC, which had been last affected by plague at least 10 years before experienced a re-emergence in April 2021. Fataki health zone registered at least 37 suspected pneumonic plague cases, including 12 deaths between 22nd April-13th June 2021. Due to the proximity of the Fataki health zone to the Ugandan border (80 km from Zombo border which is the nearest) and history of plague importation from DRC in the past, the risk of plague importation in the West Nile was highly likely [3].
While there have been efforts to ensure prompt detection and management of plague cases including setting up a plague laboratory in Arua district and distributing plague test kits in the facilities serving the border population, the threat of occurrence remains eminent. We assessed the risk in the West Nile border districts for plague importation, determined the level of preparedness of individual districts to respond to the event of an outbreak and assessed community knowledge and practices about plague to inform planning.
Materials and Methods
Study setting and design
We conducted the assessment in the six West Nile districts (Koboko, Maracha, Arua, Zombo, Packwach, Nebbi) and Arua city.
This assessment was conducted during August 1st-23rd, 2021, by a multi sectoral national rapid response team. We assessed the population movement patterns across borders using the Population Connectivity Across Borders (POPCAB) toolkit to understand risks of plague associated with population movement across borders in the six border districts and city. We adapted the World Health Organization (WHO) plague readiness checklist to assess readiness and capacity of districts and healthy facilities to respond to a plague outbreak. We conducted community assessments using a semi-structured interview guide to assess the community knowledge and practices about plague.
Sample size, sampling considerations, study variables and data collection population connectivity across borders assessment
Using the POBCAB tool kit, we conducted 16 Key Informant Interviews (KIIs) and reached saturation. We asked about the category of travelers crossing border points, probed for the main reasons why they cross the border, the duration of their stay and districts most visited after crossing the border and points of entry commonly used. Findings from the key informant interviews informed the selection of category and grouping of the Focus Group Discussions (FGDs) and the appropriate locations for these FGDs to further assess the variables explored first using the KIIs.
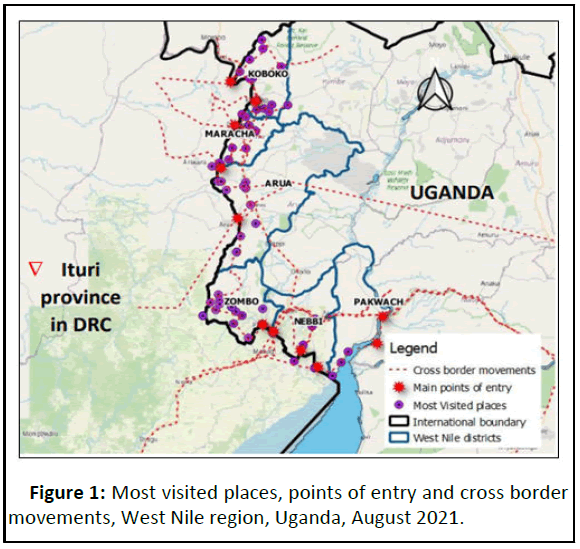
We conducted 21 FGDs and reached saturation. Each FGD was composed of an average of six participants (Border health staff, village health team member, transportation official, an informal trader in markets, and a community leader). We characterized cross border movements using participatory mapping while conducting the KIIs and FGDs through annotating points of interest, assessing travel routes and Points of Entry (PoEs), types of travellers coming from DRC to Uganda, reasons for travel and places frequently visited showing areas with high influx between the two countries.
District and health facility preparedness assessment
We collected data from the district health team on readiness to respond to a plague outbreak using an adapted WHO plague readiness checklist under the broad categories of coordination mechanisms, surveillance including points of entry, laboratory capacities, risk communication and community engagement, vector management, logistics and patient management to assess readiness and capacity of districts to respond.
We assessed 47 health facilities serving border communities and those most visited by travellers as identified during KII and FGD interviews. We carried out interviews with health facility incharges about their readiness or preparedness in terms of healthcare worker training, availability of standard operating procedures, and training of village health teams.
Community knowledge and practices assessment
To determine the level of knowledge and practices about plague by community members, we enrolled 120 participants from FDGs with community members from spot areas of border populations, markets, and congested areas. We interviewed these individuals using a semi structured interviewing guide with 10 questions about general knowledge on plague disease, mode of transmission, prevention and rat/rodent mortalities in the community. Those who answered correctly ≥ 70% of the questions were categorized as very knowledgeable, 50%-70% of the questions were knowledgeable, and those who answered <50 questions were not knowledgeable.
Data analysis
We assessed districts’ preparedness to respond to plague using the adapted WHO checklist and readiness score criteria [4,5]. The adapted checklist had 38 questions to assess the readiness and preparedness and every positive answer (desired answer) was awarded 1 and the negative answers (undesired answers) were scored with 0 (scores less than 40% indicated ‘not prepared’ while 41%-80% as prepared and above 80% indicated very prepared). We categorized districts’ risk of plague importation into two categories based on previous cases, the volume of cross-border movements, and proximity to the plague outbreak epi center Ituri province.
To assess the healthy facilities level of readiness to respond to a plague outbreak, we created composite scores using principal component analysis. We used readiness scores that were derived using Principal Component Analysis (PCA) to categorise the level of readiness of the health facilities to respond to plague. Scores were assigned to readiness variables with a scale of 1-5 and those that scored <2 were “not prepared”, those that scored 2-3.9 were in “partially prepared” and those health facilities that scored 4-5 were categorised as “very prepared” [6].
We calculated composite scores to determine the community level of knowledge about plague and its transmission. We calculated percentages of those with experience of recent rat die off places in their community to describe practices related to plague prevention.
Results
Population connectivity across boarders
Frequent travelers across the border were mainly traders, school-going children and patients seeking healthcare, visitors, refugees due to insecurity in DRC and those going/coming for leisure activities. Travellers mainly used bicycles, tricycles (tukutukus), and trucks carrying other goods and boats. These travellers visited particular districts within the region; health facilities (20 health facilities); trading centres (markets and towns); schools (11 schools); mainly used 11 PoEs (Figure 1).
District and health facility preparedness
At district level, all 6 districts and Arua city scored <40%. Zombo and Arua districts had the highest scores (39%) in comparison to other border districts (Figure 2). Arua city and Zombo district were in category one of risk (highest risk) of importation of plague while the others were in category two (Figure 3).
Of 47 health facilities assessed, none was adequately prepared to respond to the plague outbreak in the event it occurred. Among partially prepared health facilities (25; 53%), Zombo district had the highest number (8; 32%) followed by Arua (5; 20%) while Koboko had none. All 6 facilities assessed in Koboko District were not prepared (Table 1).
| District | Number of health facilities not prepared | Number of health facilities partially prepared | Number of health facilities prepared |
|---|---|---|---|
| Zombo | 0 | 8 | 0 |
| Arua | 3 | 5 | 0 |
| Maracha | 3 | 4 | 0 |
| Nebbi | 6 | 5 | 0 |
| Arua city | 0 | 1 | 0 |
| Pakwach | 3 | 2 | 0 |
| Koboko | 7 | 0 | 0 |
Table 1: Level of preparedness of health facilities to respond to plague outbreak, West Nile districts and Arua city, Uganda, August 2021.
Community knowledge and practices
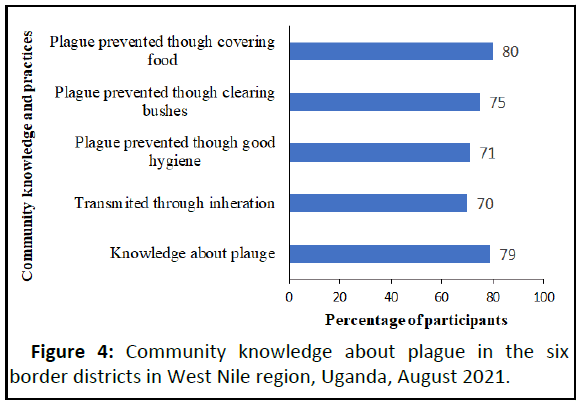
Of the 120 participants interviewed, 95 participants (79%) were very knowledgeable about how plague by mentioning right answers on how plague can be spread, right signs and symptoms of plague and how it can be prevented (Figure 4). Only 30 participants (25%) had seen the dead rats in their communities and of these participants through further probing (28; 93%) said these rats had died due to poisoning and 2 participants (7%) said they didn’t know what had killed the rats they saw in their communities.
Discussion
We highlight the potential risk of importation and spread of plague through population connectivity across borders, particularly among frequent travelers who engaged in various activities such as trade, education, healthcare seeking and leisure. The risk for spread was likely worsened by low preparedness levels of west Nile border districts and health facilities to respond to a potential outbreak. Our findings are consistent with previous studies conducted in Uganda, which have shown that human plague cases are often associated with exposure to rodents and their fleas, which are commonly found in trading centers and other areas of high human activity [7]. Also a study conducted in the West African region following the Ebola outbreak in 2014-2016 identified cross border movement as a key driver of the epidemic [8]. Another study conducted in East Africa found that cross border traders played a crucial role in facilitating the spread of malaria [9]. These studies highlight the importance of understanding the patterns of cross border travel and designing effective interventions to mitigate the risks of disease transmission. Low levels of preparedness to respond increases the risk of disease outbreaks and this has also been highlighted by a study conducted across the border region between Ethiopia and Somalia [10].
Strong population connectivity across borders is perpetuated by business, search for health and medical services and social activities and insecurity in DRC which forced people to seek refuge in Uganda.
The mapping of routes established high cross border movements. Access to Uganda from DRC were through both legal and illegal routes which made it even more difficult to have controlled population movements just like it was highlighted in an earlier study conducted in southwestern Uganda [11]. These findings are also in agreement with a 2018 assessment report which stated that there are high cross border movements between Uganda and DRC and these movements were mainly facilitated by trade, healthcare services, insecurity, and social amenities in both countries. Likely, proximity to the epi center in DRC and high cross border movements between Uganda and DRC contribute to the risk of plague importation in West Nile’s border districts.
No district or health facility (among the assessed ones) was prepared to respond to the plague in case an introduction occurred. Health workers had not been trained in the last two years and also health facilities serving these border populations didn’t have plague test kits. The inadequate preparedness of districts and health facilities in response to a potential outbreak of plague is a major concern, as highlighted in this study. Similarly, previous studies have also identified the need for improved surveillance and response systems to prevent and control plague outbreaks. A 2018 assessment of Ebola virus disease infection prevention and control capacity in border districts of Bundibugyo, Kabarole and Kasese districts, also established that preparedness in health facilities was lacking. Another study on the preparedness of health care systems for Ebola outbreak response in Kasese and Rubirizi districts found that all health facilities assessed were unprepared to respond to the emergency in case it occurred. Enhancing disease preparedness and response strategies is vital especially when population movement patterns between an outbreak area and neighboring countries have been established.
The communities were very knowledgeable about plague, its transmission, and prevention. Community knowledge and practices regarding plague are important in preventing the spread of the disease. A high percentage of participants had good knowledge about how plague is spread, its signs and symptoms and how it can be prevented. This is consistent with a previous study conducted in Uganda, which also found that knowledge about the disease was relatively high among the general population. However, the study also found that few participants had seen dead rats in their communities, and of those who did, many attributed the deaths to poisoning. This suggests a potential lack of awareness regarding the role of rodents in transmitting the disease.
Study limitations
This study relied on self-reported data from key informants, FGD participants, and health facility in-charges. There was a possibility of response bias, where participants provided socially desirable answers or withheld information due to fear or mistrust. Additionally, the accuracy of the information provided might have been limited by the participants' memory or understanding of the questions.
Public health actions
Uganda ministry of health used these findings to generate a rapid response plan for the six districts and Arua city which were considered to be at risk of plague importation. We carried out continuous medical education at three health facilities in Nebbi where health workers had not been trained at all in plague related activities. We distributed information education and communication materials in form of flyers about plague at two district headquarters and five health facilities and drafted a poster about plague, which was used in commissioning the Arua regional emergency operations centre hence creating more publicity about the disease.
Conclusion
The risk of plague importation from DRC to West Nile was found to be high due to high connectivity across borders using both legal and illegal routes in all the six districts and Arua city. No health facility or district was prepared to respond to the outbreak/importation of plague in case it occurred. Community members exhibited high knowledge about plague, its modes of transmission and prevention.
We recommended orientation/training of district health teams in plague related activities in the high risk districts of Arua and Zombo, reactivating and equipping border health teams to do screening of plague at POEs. This study emphasizes the need for continued efforts to improve preparedness and response to plague outbreaks in Uganda, particularly in border districts with high population connectivity.
Ethical Considerations
The ministry of health of Uganda directed and permitted us to carry out this assessment. Also, the US Centers for disease control and prevention determined and approved that this activity was not research and that its primary intent was disease control and prevention. We explained the procedures and intention of this assessment before this study commenced to the study participants. We obtained both verbal and written informed consent from participants aged ≥ 18 years who were interviewed and recorded.
Acknowledgment
We acknowledge the district local government for all the six districts and Arua city for assessment. We appreciate the infectious diseases institute, baylor college of medicine children's foundation Uganda, Uganda virus research institute and US centers for disease control and prevention for the support in designing tools and for the technical advice rendered during the assessment.
Competing Interests
The author declares that there was no competing/conflict of interest.
Authors Contribution
IA, took lead in execution of this assessment. She wrote the drafts of the manuscript and revised the paper for substantial intellectual content. DNG, and SN, participated in developing the protocol, and designed methodology and tools; ARA, OF, LA, MS and JO gave technical support to the author by editing the tools and the protocol; BOA and IW trained the participants in the methodology. GE, AK, BK, LB and DK gave supervisory assistance; TA, JFO, GC, AK, SS, PM, EJN, HTN, SRA, MN participated in the data collection process. All authors approved the manuscript for publication.
References
- Apangu T, Acayo S, Atiku LA, Apio H, Candini G, et al. (2020) Intervention to stop transmission of imported pneumonic plague, Uganda, 2019. MMWR Morb Mortal Wkly Rep 69:241-244
[Crossref] [Google Scholar] [PubMed]
- Gonahasa DN (2019) Prompt response to a cross border plague outbreak in Zombo district, minimized spread, Uganda, March 2019. J Interval Epidemiol Public Health 5:6
- Outbreak News Today (2021) Plague in DRC: 1st cases reported in Fataki health zone in a decade. July 13
- Forrester JD, Apangu T, Griffith K, Acayo S, Yockey B, et al. (2017) Patterns of human plague in Uganda, 2008–2016. Emerg Infect Dis 23:1517-1521
[Crossref] [Google Scholar] [PubMed]
- National academies of sciences E, division H and M, health B on G, threats F on M. The outbreak (2016). In: The Ebola epidemic in West Africa: Proceedings of a workshop. National Academies Press, US
- Wangdi K, Gatton ML, Kelly GC, Clements ACA (2015) Chapter two cross border malaria: A major obstacle for malaria elimination. In: Rollinson D, Stothard JR, editors. Advances in parasitology. Academic Press.
- Arale A, Lutukai M, Mohamed S, Bologna L, Stamidis KV (2019) Preventing importation of poliovirus in the horn of Africa: The success of the cross-border health initiative in Kenya and Somalia. Am J Trop Med Hyg 101:100-106
[Crossref] [Google Scholar] [PubMed]
- Nakiire L, Mwanja H, Pillai SK, Gasanani J, Ntungire D, et al. (2020) Population movement patterns among the democratic republic of the Congo, Rwanda, and Uganda during an outbreak of Ebola virus disease: Results from community engagement in two districts Uganda, March 2019. MMWR Morb Mortal Wkly Rep 69:10-13
[Crossref] [Google Scholar] [PubMed]
- Biedron C (2018) Evaluation of infection prevention and control readiness at frontline health care facilities in high risk districts bordering ebola virus disease. Affected areas in the democratic republic of the Congo Uganda.
- Kibuule M, Sekimpi D, Agaba A, Halage AA, Jonga M, et al. (2021) Preparedness of health care systems for Ebola outbreak response in Kasese and Rubirizi districts, Western Uganda. BMC Public Health 21:1-6
[Crossref] [Google Scholar] [PubMed]
- Kugeler KJ, Apangu T, Forrester JD, Griffith KS, Candini G, et al. (2017) Knowledge and practices related to plague in an endemic area of Uganda. Int J Infect Dis 64:80-84
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences