Review on Trauma Care in Hong Kong
Diane Tai Hei-Yan*
Department of Orthopaedics and Traumatology, Queen Elizabeth Hospital, Hong Kong
- *Corresponding Author:
- Diane Tai Hei-yan
Queen Elizabeth Hospital, Hong Kong
Tel: (852) 29582162
E-mail: dianetai510@yahoo.com
Received date: November 09, 2016; Accepted date: December 01, 2016; Published date: December 10, 2016
Citation: Hei-Yan DT. Review on trauma care in Hong Kong. J Emerg Trauma Care 2016; 1:2
Abstract
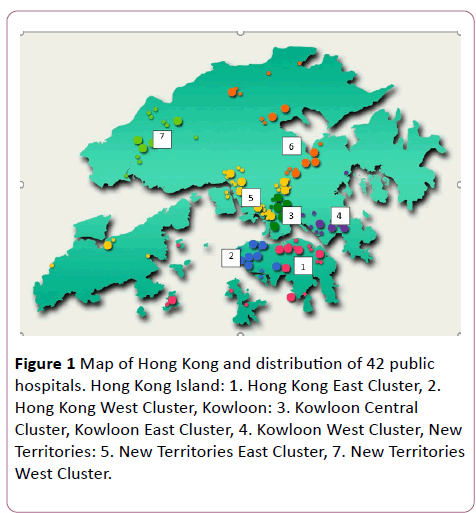
Trauma is the third leading cause of death worldwide and is the fifth leading cause of death categorized as "injury, poisoning and certain other consequences of external causes" by the Department of Health in Hong Kong in 2015. The annual incidence of trauma increased progressively in the 1970s, reached a peak in the mid-1980s, and then fell despite the population growth. The population of Hong Kong is 7.32 million in 2015, with an area of 1098 kilometer square. All public hospitals in Hong Kong are managed by an independent body called the hospital authority (HA). Currently, 17 major public hospitals out of 42 provide accident and emergency (A&E) services. These hospitals are organized into seven hospital clusters based on their locations. This article is to review the current trauma care system in Hong Kong and make some suggestions on the future development.
Keywords
Trauma; Diversion; Pelvic fracture
Background
Trauma is the third leading cause of death worldwide and is the fifth leading cause of death categorized as “injury, poisoning and certain other consequences of external causes” by the department of health in Hong Kong in 2015 [1]. The annual incidence of trauma increased progressively in the 1970s, reached a peak in the mid-1980s, and then fell despite the population growth [2] Rainer et al reported that the patterns of severe trauma in Hong Kong primarily affect male adults, and 55% of them resulted from road traffic accidents [3]. Blunt injury accounted for 92.6% and penetrating injury accounted for 7.4% of these patients.
The population of Hong Kong is 7.32 million in 2015, with an area of 1098-kilometre square. All public hospitals in Hong Kong are managed by an independent body called the hospital authority (HA). Currently, 17 major public hospitals out of 42 provide accident and emergency (A&E) services [4]. These hospitals are organized into seven hospital clusters based on their locations
Before the 1990s, there were no dedicated trauma centers. Patients were taken to the nearest hospitals regardless of the severity and complexity of the injury. The clinical outcomes were unsatisfactory. Kam et al. reported in 1998 that 94 significantly injured patients over a 24-month period, who were managed by the Hospital Trauma Team in one general hospital, had a mortality rate of 39%, and up to 24% of these deaths were potentially preventable [5]. The probable causes for the potentially preventable deaths include delay owing to inter-hospital transfer, delay in activation of the trauma team, unidentified intra-peritoneal haemorrhage, failure to control haemorrhage and delayed or inadequate definitive operation Figure 1.
Figure 1: Map of Hong Kong and distribution of 42 public hospitals. Hong Kong Island: 1. Hong Kong East Cluster, 2. Hong Kong West Cluster, Kowloon: 3. Kowloon Central Cluster, Kowloon East Cluster, 4. Kowloon West Cluster, New Territories: 5. New Territories East Cluster, 7. New Territories West Cluster.
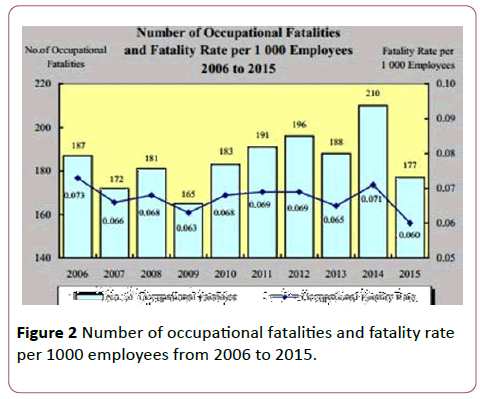
In 1994, Professor Donald Turkey recommended the HA on the development of a coordinated trauma system and designation of trauma centres. In 2000, the HA identified several deficiencies in trauma care [6]. A panel consisting of overseas experts advised the establishment of two to three level I trauma centres in Hong Kong. Subsequently, five trauma centres were designated. These trauma centres were managed under the HA central committee on trauma service (HACCTS). It coordinates trauma care at multi-disciplinary level and consists of representatives from Anaesthesiology, Emergency Medicine, Intensive Care, Neurosurgery, Orthopaedics and Traumatology, Radiology, and Surgery. It is an integration of pre-hospital care, inter-hospital transfer, trauma centres, rehabilitation, prevention, education, and research. Leung [7], reported that trauma registries at the five trauma centres captured just over 2000 patients annually in total. Over 70% of these were men. The highest rate of admission was in the 21-30 years age group. Head injuries occurred in 50% and severe injury, defined as an injury severity score greater than 15, occurred in 30% of patients. From the statistics by the Labour Department, the occupational fatality rate in 2015 was 0.60 per 1000 employees Figure 2.
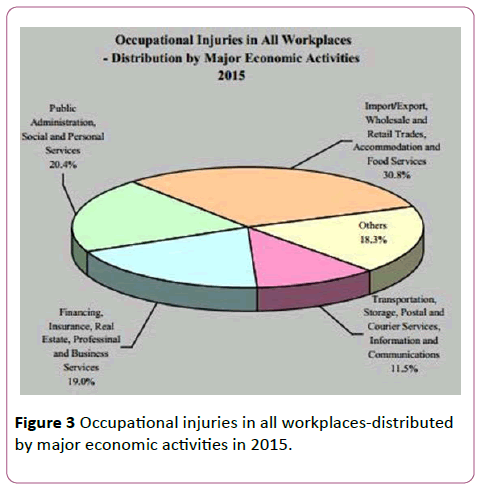
Of the 35852 occupational injuries in 2015, over 80% occurred in the major economic sectors presented in Figure 3.
Current System
Hong Kong is a small and densely populated city with well-established transport system and highways. The HA suggested primary trauma diversion (PTD) in Hong Kong. Patients who fulfil any one of the criteria for PTD are transported directly from the scene to the local trauma center Table 1.
| Anatomical criteria |
| Flail chest |
| Lower limb fracture involving two long bones |
| Amputation proximal to wrist or ankle |
| All penetrating injuries to head, neck, or torso |
| Limb paralysis |
| Pelvic fracture |
| Combined trauma and burns (>2nd degree or >20%) |
| Physiological criteria |
| GCS<14 |
| Systolic blood pressure <90 mmHg |
| Respiratory rate <10 or >29 per minute |
Table 1: Anatomical and physiological criteria for primary trauma diversion in Hong Kong
A pilot prospective study was conducted in 2003 in the new territories east cluster (NTEC) involving two major public hospitals [8]. It was found that the median injury severity score (ISS) of these diverted patients was 9% and 52% of them had been involved in road traffic accidents. Among these patients, 76% of them were diverted correctly according to the protocol, and that primary trauma diversion patients reached definitive care 97 minutes faster than patients undergoing secondary diversion Table 2.
| Primary Trauma Diversion (n=60) | |
|---|---|
| Mean age | 39 |
| Gender (M:F) | 38:22 |
| Causes of injury | |
| Motor vehicle crash | 24 (40%) |
| Bicycle crash | 7 (11.7%) |
| Fall >1metre | (21.7%) |
| Fall <1metre | (6.7%) |
| Struck by object | 3 (5%) |
| Penetrating assault | (6.7%) |
| Burn / scald | (3.3%) |
| Others | 3 (5%) |
| Injury Severity Score | |
| 1-8 | 21 |
| 9-15 | 25 |
| >15 | 14 |
Table 2: Part of the basic data for diverted cases.
Suen, et al [9]. reported in 2011 that the mean ISS under PTD in the Kowloon Central Cluster (KCC) was 11.7 in 163 diverted patients; and 125 out of these 163 patients (76.7%) were diverted correctly; 38 out of these 163 patients (23.3%) who did not fulfil the PTD criteria were considered as “over-diverted” Table 3.
| Total PTD Patients (n=163) | |
| Fulfil diversion criteria (n=125) 76% correctly diverted |
Not fulfil diversion criteria (n=38) 23.3% over-diverted |
Table 3: Results of primary trauma diversion.
The compliance rate of PTD was 74% compared with 39.9% to 56.4% in the United States [10,11]. However, there were five cases of pelvic fractures not suspected in the field until further assessment and imaging was done in the nearest regional hospitals. These cases required secondary transfer to trauma centre for definitive treatment.
In recent years, there has been a major change in the clinical management of pelvic fracture among trauma patients in Hong Kong. In the 1990s, patients admitted to the AED with obvious pelvic fracture on X-rays would be treated with external fixation if indicated. Later, angiography and embolization became available and remained a treatment option for patients with unstable blood pressure despite on external fixation. Until recent years, a clinical protocol was established in Queen Elizabeth Hospital, one of the trauma centres in Hong Kong Ip et al reported a significant improvement in the survival rate of trauma patients with pelvic fracture from 31% to 66% [12]. The protocol recommended that patients should be given pelvic binder on the scene upon suspicion of pelvic fracture. Focused assessment with sonography for trauma (FAST) scan is performed at AED, if there is any positive finding, patients would be sent to the operation theatre for laparotomy followed by external fixation, pelvic packing, and angiography. If there is no positive finding on FAST scan and patients are unstable hemodynamically, they would be sent to the operation theatre and treated with external fixation, pelvic packing, and angiography. This timely multi-disciplinary approach aimed at preventing bleeding and reducing mortality.
The Future
Trauma centres and trauma systems were introduced in the United States in the mid-1970s, and it has been accompanied by the development of trauma registries [13]. Trauma registries have been demonstrated to describe the pattern of trauma, outcome of trauma patients and workload of healthcare providers; and to provide data for clinical research purposes. In Hong Kong, there is no centralized system for trauma registries. Trauma centres in Hong Kong have their own registry systems in different formats and with different parameters. It would be very useful to have collective data to evaluate the performance of not just one hospital but that in the whole region. It could be institution-based or central registry on voluntary basis.
Prevention is better than cure. It is one of the key elements in trauma care system. As mentioned before, about half of the severely injured trauma patients are due to motor vehicle accidents. Hong Kong has a very low motor vehicle death rate (2.4 per 100,000). But the rate is much higher related to motor vehicle registrations (33 per 100,000). Elderly patients were predominant, 37% of the mortality cases reported by Cameron et al. involved individuals older than 60 years of age [14]. Among these cases, 59% were pedestrians. Alcohol was isolated to the group 20 to 40 years of age. From the statistics by the Centre for Health Protection of the Hong Kong Government in 2008, 90.9% of the youth aged 10 to 19 would not wear a helmet when riding a bicycle; and 91.5% of the youth aged 10 to 19 would comply with the traffic lights most of the time when crossing a road [1]. Better public education in terms of road traffic safety is crucial in the prevention of severe trauma cases in Hong Kong, e.g. use of helmets when riding bicycles, complying with traffic lights, etc. A community outreach prevention program would be useful to help people reduce the risk of injury, like Think First programs in the US, especially in high risk groups like children, youth, and young adults [15].
References
- Centre for Health Protection (2001) Department of health, the government of the Hong Kong special administrative region.
- Census and Statistics Department (1994) Hong Kong annual digest of statistics. Hong Kong: Government Printer, 1994.
- Rainer TH, Chan SY, Wok WW, Suen DTK, Lam W (2000) Severe trauma presenting to the resuscitation room of a Hong Kong emergency department. Hong Kong J Emerg Med 7 :129-135.
- Information services department, Hong Kong special administrative region government.
- Kam CW, Kitchell AK, Yau HH, Kan CH (1985) Outcome of major trauma patients in a Hong Kong general hospital. Eur J Emerg Med 5: 297-306.
- Medical services development committee, hospital authority, Hong Kong. Organisation and development of trauma care in HA. Hong Kong SAR, 2001.
- Leung GKK (2010) Trauma system in Hong Kong. Surgical practice 14: 38-43.
- Cheung NK, Yeung JHH, Chan JTS, Cameron PA, Graham CA, et al. (2006) Primary trauma diversion: Initial experience in Hong Kong. J Trauma 61: 954-960.
- Suen KW, Chang AML, Au CKH (2011) A regional study on primary trauma diversion in Hong Kong. Hong Kong J Emerg Med 18: 92-100.
- Ma MH, MacKenzie EJ, Alcorta R, Kelen GD (1999) Compliance with prehospital triage protocols for major trauma patients. J Trauma 46:168-175.
- Baez AA, Lane PL, Sorondo B (2003) System compliance with out-of-hospital trauma triage criteria. J Trauma 54: 344-351.
- Ip KC, Lee KB (2014) Standardized multidisciplinary protocol for haemodynamically unstable pelvic fractures. J Orthop Surg 22: 177-180.
- Cameron PA, Gabbe BJ, McNeil JJ, Finch CF, Smith KL, et al. (2005) The trauma registry as a statewide quality improvement tool. J Trauma 59: 1469-1476.
- Cameron PA, Rainer TH, Mak P (2004) Motor vehicle deaths in Hong Kong: Opportunities for improvement. J Trauma 56: 890-893.
- Think First, National Injury Prevention Foundation.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences