Retroperitoneal Lymph Node Metastasis from a Low Rectal Cancer Treated with Chemoradiation Therapy and Surgery with Complete Pathological and Image Response: A Case Report
Luis Bayardo-López1, Adriana Alvarado-Zermeño2, Luis Salazar-Muñoz2, Carlos Mariscal-Ramirez2, Enrique Gutierrez-Valencia3* and Adrian Valles-Quintanilla3
1Department of Radiation Oncology, Centro Medico Nacional de Occidente, Guadalajara, Mexico
2Department of Radiotherapy, Centro Medico Nacional de Occidente, Guadalajara, Mexico
3Radiation Oncology, Centro Medico Nacional de Occidente, Guadalajara, Mexico
- *Corresponding Author:
- Enrique Gutiérrez-Valencia
Resident of Radiation Oncology
Centro Medico Nacional de Occidente
Guadalajara, Mexico
Tel: 01 33 1341 6402
E-mail: jeguval@hotmail.com
Received Date: February 04, 2017; Accepted Date: February 27, 2017; Published Date: March 06, 2017
Citation: Bayardo-López L, Alvarado-Zermeño A, Salazar-Muñoz L, et al. Retroperitoneal Lymph Node Metastasis from a Low Rectal Cancer Treated with Chemoradiation Therapy and Surgery with Complete Pathological and Image Response: A Case Report. J Clin Med Ther. 2017, 2:2.
Copyright: © 2017 Bayardo-López L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Colorectal cancer is one of the most common cancers in gastrointestinal tract. It represents the third most common malignancy in the United States, currently the treatment options for colorectal cancer in advanced stages IV A (metastasic disease in one organ) are controversial and there is not strong evidence about how these patient should be treated, here, we present the case of a 58 year old woman with colorectal cancer staged IVA (retroperitoneal lymph nodes metastasic disease at diagnosis) who was treated with neoadjuvant chemoradiotherapy and subsequent surgery with complete pathological response and image response.
Keywords
Retroperitoneal; Lymph node; Low rectal cancer; Chemoradiation therapy; Metastasic disease
Introduction
In the United States, Colorectal Cancer represents the third most common malignancy and the third most common cause of cancer death in both sexes [1]. The stage at diagnosis is a powerful indicator of prognosis.
Rectal cancer in advanced-stage represents 20% of all newly diagnosed cancers, and 5 year survival rate is only 8%. The incidence of retroperitoneal lymph node metastases is 1-2%.
The optimal management of retroperitoneal lymph node metastases is controversial, but several studies have suggested surgery as a good option with 5 years overall survival rate of 15-53% vs. 0-12% in patients who did not undergo surgery. Radiation therapy could be an option in patients who will not undergo surgery.
Case Report
A 58 Year-old woman from Guadalajara, Jalisco with no significant past medical history presented to our hospital in October 2015 with an 8 month history of intermittent abdominal pain and change in bowel habits, physical examination was unremarkable [1].
Colonoscopy was performed with the following findings: a rectum tumor was observed at 5 cm from anal margin, the tumor had 4 cm length with polypoid and exophytic shape. A biopsy of the tumor was made with a histopathology report of a high grade adenocarcinoma.
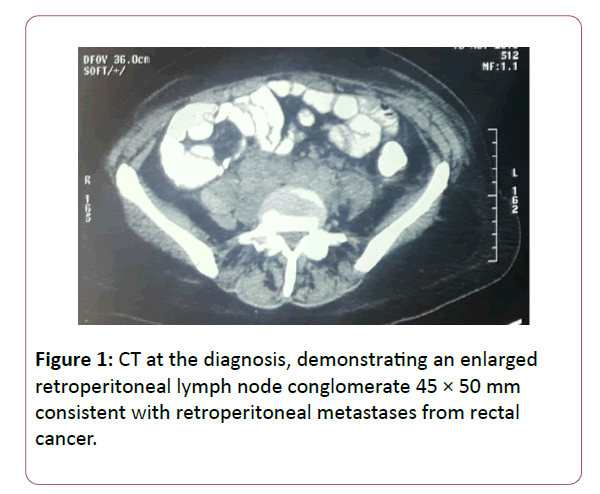
Computed tomography scan of the chest, abdomen and pelvis demonstrated retro peritoneal lymphadenopathy 4 × 5 cm consistent with lymph nodes metastasic disease, no metastases disease was observed in other organs (Figure 1). The disease was staged using the American Joint Commission on Cancer Tumor, Node and Metastasis Staging system stage T3 N0 M1 Stage IV A. The patient was referred to Radiation Oncology and Medical Oncology for neoadjuvant treatment with chemoradiation.
The patient received induction chemotherapy for 3 cycles with XELOX (capecitabine plus Oxalinplatino) in 3 week treatment cycles intravenous oxaliplatin 130 mg/m2 (day 1) followed by oral capecitabine 1,000 mg/m2 twice daily and by bevacizumab (BEV) (7.5 mg/kg) on day 1 of the 3 week cycle.
After the induction chemotherapy the patient was treated with linear accelerator Three-Dimensional (3D) conformal radiation therapy using Monaco Treatment Planning System with Extended-field radiation therapy to para-aortic lymph node metastasis and pelvis. A total of 5040 cGy was given in 28 fractions From June 15 to July 28, 2016 with concomitant capecitabine. The treatment was well tolerated only with grade 2 toxicity in skin reported according to RTGO scale toxicity [2].
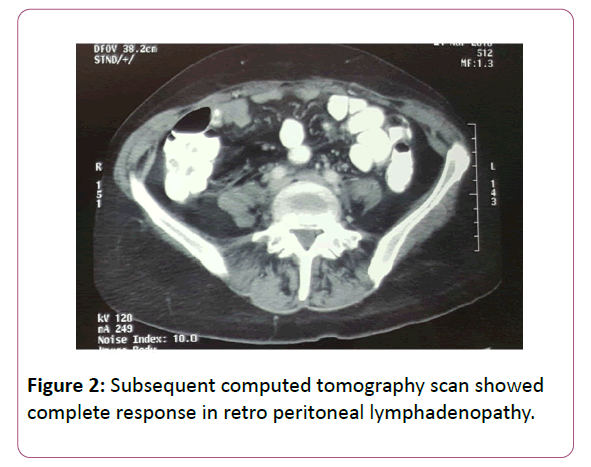
After the chemoradio therapy treatment, a subsequent computed tomography scan showed complete response in retro peritoneal lymphadenopathy (Figure 2). In October 2016, the patient underwent surgery with low anterior resection with primary anastomosis and retroperitoneal exploration, no retroperitoneal lymph nodes were observed during the surgery [3,4].
Figure 2: Subsequent computed tomography scan showed complete response in retro peritoneal lymphadenopathy.
The histopathology reported a pathological complete response in rectum as well negative lymphnode metastases and peritoneal liquid. After the surgery the patient received capecitabine 1,000 mg/m2 as adjuvant treatment with no side effects reported.
The patient continued close follow up, after 1 year a colonoscopy and CT were performed and demonstrated no tumor activity [5].
Conclusion
We present a case of metastasic rectum cancer with complete clinical and pathologic response despite the diseases IVA (retroperitoneal lymph nodes metastases) stage. The patient was treated with radical treatment with tri-modal treatment (chemotherapy, radiation therapy and surgery. In previous studies, patients with metastasic rectal cancer in one organ (stage IVA) the overall survival to 5 years has been 20% [6]. There is no clear evidence about how these patients should be treated. The NCCN 2017 recommends the individualization of treatment in this scenario.
References
- Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65: 5-29.
- Veronese N, Nottegar A, Pea A, Solmi M, Stubbs B, et al. (2016) Prognosis impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol 27: 42-48.
- Stillwell P, Ho YH, Veitch C (2011) Systematic Review of Prognostic Factors Related to Overall Survival in Patients with Stage IV Colorectal Cancer and Unresectable Metastases. World J Surg 35: 684-692.
- Yun HR, Lee WY, Lee WS, Cho YB, Yun SH, et al. (2007) The prognostic factors of stage IV colorectal cancer and assessment of proper treatment according to the patient’s status. Int J Colorectal Dis 22: 1301-1310.
- Hino H, Kagawa H, Kinugasa Y, Shiomi A, Yamaguchi T, et al. (2016) Long-term survival with surgery for metachronous retroperitoneal lymph node and pancreatic metastases after curative resection of rectal cancer: a case report. Surg Case Rep 2: 49.
- Gagnière J, Dupré A, Chabaud S, Peyrat P, Meeus P, et al. (2015) Retroperitoneal nodal metastases from colorectal cancer: Curable metastases with radical retroperitoneal lymphadenectomy in selected patients. Eur J Surg Oncol 41: 731-737.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences