Renal Squamous Cell Carcinoma: Rare and Aggressive Variant of Renal Cancers
El Hachem G1*, Choueiry C2, Al Hajj Obeid W3 and Chamseddine N1
1Department of Medical Oncology, Saint Georges Hospital, University of Balamand, Beirut, Lebanon
2Department of Pathology, Saint Georges Hospital, University of Balamand, Beirut, Lebanon
3Department of Urology, Saint Georges Hospital, University of Balamand, Beirut, Lebanon
- *Corresponding Author:
- El Hachem G
MD, Department of Medical Oncology
- Saint Georges Hospital
- University of Balamand
Beirut, Lebanon
Tel: +961 3 076875
E-mail: george.el.hashem@hotmail.com
Received Date: October 03, 2017; Accepted Date: October 09, 2017; Published Date: October 15, 2017
Citation: El Hachem G, Choueiry C, Al Hajj Obeid W, Chamseddine N (2017) Renal Squamous Cell Carcinoma: Rare and Aggressive Variant of Renal Cancers. Cancer Biol Ther Oncol. Vol.1 No. 2:6.
Abstract
Squamous cell carcinoma (SCC) of the kidney is a rare and fatal clinical entity. It is usually aggressive with generalized disseminated disease upon presentation. Here we report the case of 61 years old male patient, with no previous history of kidney stones or other medical problems, who presented for dyspnea, hemoptysis, left flank pain and hematuria. He was diagnosed with stage IV undifferentiated SCC of the left kidney. He had a dramatic clinical evolution, with rapid progression, leading to deterioration and death. Renal squamous cell carcinoma remains an unusual, unsuspected diagnosis of kidney tumors with a poor prognosis.
Keywords
Kidney; Squamous cell carcinoma
Introduction
Squamous cell carcinoma (SCC) of the kidney is exceptional and constitutes less than 1% of all urinary tract neoplasms [1]. The SCC is more frequently reported in urinary bladder and urethra rather than the kidney. This pathologic subtype is very aggressive, usually high grade, and presents at an advanced stage. Thus, it is associated with a poor prognosis [2].
Case Presentation
Our patient is a 61 years old gentleman, non-smoker, previously healthy, who was admitted to our institution for gross hematuria, hemoptysis and shortness of breath. History goes back to 4 months prior to his presentation, when he started complaining of intermittent gross hematuria, associated with left flank pain without fever or chills. Few weeks later, he had a new onset dry cough associated with dyspnea on exertion. Then, he started suffering from hemoptysis with persistent intermittent hematuria and flank pain. He also reported a decreased appetite and a weight loss of 8 kg over the last 2 months. Upon admission, he was hypoxic (oxygen saturation 88%), normotensive, tachycardic to 120 bpm and diaphoretic. There were no palpable cervical, supraclavicular, axillary or inguinal lymphadenopathies. He had diffuse wheezing on auscultation, distended abdomen with a left side bulging and a tender hepatomegaly. He was irritable, not confused without any neurological deficit. Urine analysis showed 250,000 red blood cells /high power field (HPF) and 1500 white blood cells (WBC)/(HPF). Laboratory tests revealed a leucocytosis (WBC 38000/mm3 with 90% neutrophils, absence of abnormal or immature cells), grade IV anemia (normocytic, normochromic with a hemoglobin of 6.8 g/dL), thrombocytosis (platelet count of 585000/mm3). The transaminases were 3 times the upper limit of normal (ULN), GGT was 7 times the ULN, alkaline phosphatase was 9 times the ULN, but the bilirubin was normal. There was also a hypercalcemia of 16.5 mg/dL (normal value less than 10 mg/dL) and an elevated LDH of 5870 U/L (normal value less than 225 U/L). His creatinine was 0.85 mg/dL. Chest Xray revealed diffuse bilateral macronodules with interstial infiltrates. He was stabilized with oxygen, pain killers, aggressive hydration, and we started blood transfusion.
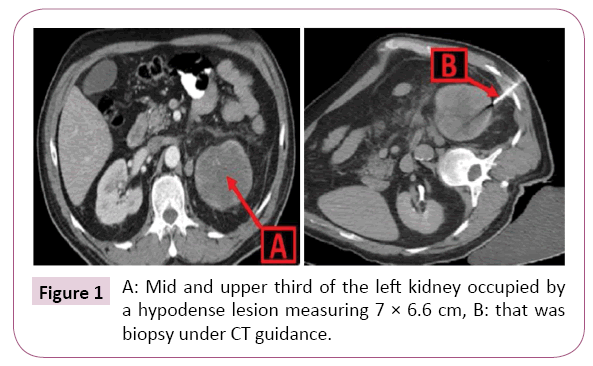
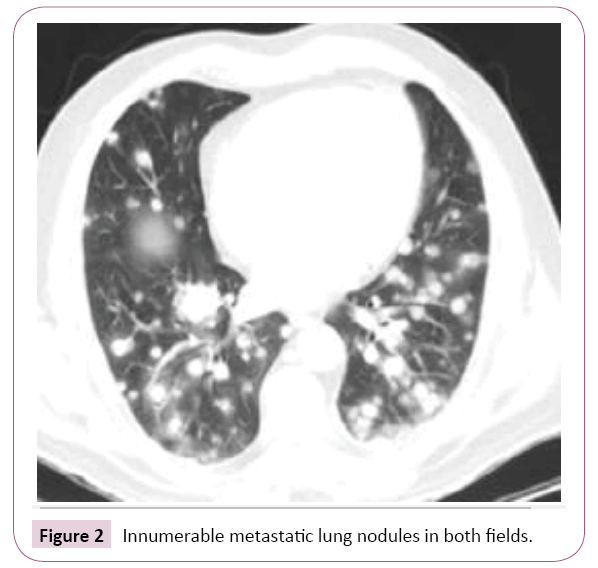
He underwent a chest abdomen and pelvis CT scan that showed innumerable bilateral macronodules in both lung fields, associated with paraseptal thickening suggestive of lymphangitic carcinomatosis, mediastinal and retro-peritoneal lymph nodes, a necrotic mass of 7 × 6.6 cm occupying the upper pole of the left kidney, associated with renal vein thrombosis and a hepatomegaly with 4 liver metastatic lesions (Figures 1 and 2). There were no kidney stones. Bone scan didn’t reveal any bone metastasis. No brain secondary deposits were detected on brain MRI. The patient also received Denosumab 120 mg sub-cutaneously.
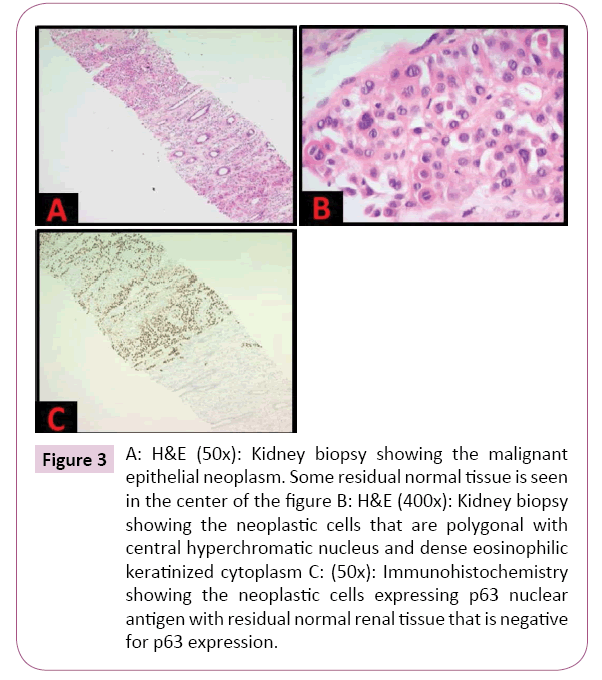
Due to his bad clinical condition, He wasn’t able to undergo a diagnostic and symptomatic left nephrectomy. A CT guided biopsy of the left kidney mass was done. Pathologic evaluation revealed a residual renal cortex that is infiltrated by an undifferentiated malignant epithelial neoplasm, composed of polygonal cells exhibiting a moderate amount of dense keratinized cytoplasm and a central hyperchromatic nucleus (Figures 3a and 3b). Immunohistochemistry revealed a diffuse expression of the p63 antigen (Figure 3c).
Figure 3: A: H&E (50x): Kidney biopsy showing the malignant epithelial neoplasm. Some residual normal tissue is seen in the center of the figure. B: H&E (400x): Kidney biopsy showing the neoplastic cells that are polygonal with central hyperchromatic nucleus and dense eosinophilic keratinized cytoplasm. C: (50x): Immunohistochemistry showing the neoplastic cells expressing p63 nuclear antigen with residual normal renal tissue that is negative for p63 expression.
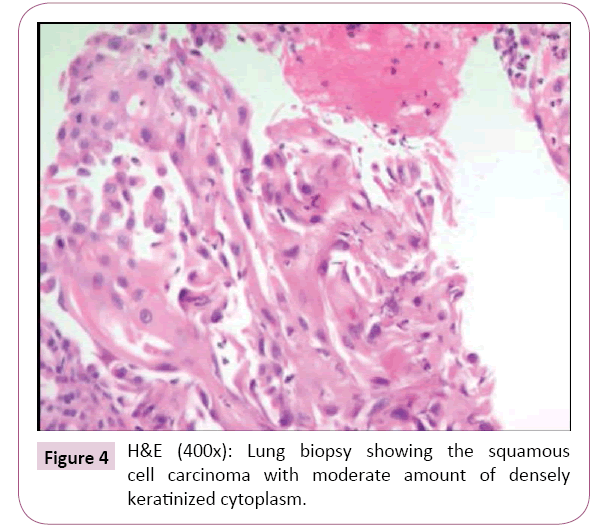
Furthermore, he underwent a cysto-ureteroscopy without evidence of any tumoral growth in the bladder or ureteras including the pyelocalyceal junctions. Multiple random biopsies were taken from the bladder, ureteral mucosa and renal pelvis, and didn’t show any dysplastic changes or malignancy. We also did a bronchoscopy with bronchoalveolar lavage and transbronchial biopsies. The pathology was positive for squamous cell carcinoma, and all microbiologic studies were negative. The features of cellular keratinization were more obvious than those in the kidney biopsy (Figure 4). The leucocyte count kept rising and reached, on day 4, a value of 95000/mm3 with predominant left shift and the anemia was corrected with blood transfusion. The calcium dropped to 10.2 mg/dL four days after he received the Denosumab with the aggressive hydration. To note that the Parathormone was undetectable, and bone marrow biopsy didn't reveal any bone marrow metastasis. We were dealing with an aggressive stage IV undifferentiated squamous cell carcinoma of the kidney metastatic to the lungs, lymph-nodes and liver, associated with paraneoplastic hypercalcemia and hyperleucocytosis. A palliative chemotherapy consisting of Cisplatin and Paclitaxel was started. He finished the first cycle, and his condition was almost stable. Before the initiation of the second cycle, he had deterioration of his clinical status, imminent gross hematuria, massive hemoptysis, worsening hypoxia, followed by respiratory failure and death.
Discussion
The most common histologic type of renal malignancies is clear cell carcinoma followed by papillary carcinoma and chromophobe carcinoma [3]. SCC in the kidney is exceptional because it usually arises from the collecting system [4]. Squamous cell carcinoma of the kidney develops after occurrence of squamous metaplasia that may progress to dysplasia then carcinoma in some patients. The primary etiologies associated with the genesis of squamous metaplasia are usually related to irritations, inflammation or infectious processes. Kidney stones are the main carcinogenic risk factor. Other predisposing factors include: chronic phenacetin and other analgesics consumption, pyelonephritis and chronic renal infectious processes, radiation therapy, vitamin A deficiency, exogenous and endogenous chemicals (Arsenic) [5].
Unfortunately, our knowledge in renal squamous cell carcinoma remain limited because it is based on case reports. SCC of the kidney usually presents with dull, atypical flank pain, associated with hematuria, and is usually suspected in context of recurrent stones or xanthogranulomatous pyelonephritis. They may be associated with paraneoplastic fever and leucocytosis secondary to cytokine storm and severe systemic inflammatory reaction. Hypercalcemia may be seen, and is secondary to bone metastasis or secretion of parathormone related peptide (PTHrp) [5]. They are usually locally advanced or metastatic on presentation due to the insidious onset of the disease and lack of any pathognomonic sign or symptom. The delay in diagnosis will result in the invasion of the renal parenchyma. Radical nephro-ureterectomy with excision of the bladder cuff is the treatment of choice for patients with loco-regional disease without distant metastases [6,7]. Local invasion of the tumor into renal parenchyma, perirenal fat, psoas muscle or vascular invasion are common pathologic findings. Unfortunately, most of the cases present initially with metastatic disease. However, nephrectomy with or without ureterectomy is recommended [6-9]. It is necessary even in the presence of metastases in order to establish a histological diagnosis, for control of symptoms such as pain, fever and hematuria or to eliminate the source of infection before systemic chemotherapy can be instituted [7,8]. Palliative chemotherapy consisting of Cisplatin based regimen and palliative radiotherapy are usually adopted for the palliative control of the metastatic disease, but they didn’t show any survival benefit [9-11]. Tyrosine kinase inhibitors with anti EGFR were tried in tumors with positive receptors without major benefit, and it still needs a larger number of case studies [12]. The prognosis of renal SCC remains very poor with a median survival of 3.5 months in cases of metastatic dissemination. This poor outcome is attributed for the advanced stage at diagnosis.
Conclusion
To conclude, renal squamous cell carcinoma is a rare entity, with an aggressive behavior. Clinicians must be aware of this pathologic variant while evaluating kidney tumors, with careful history taking, a clue about the risk factors for SCC of the kidney. Nephrectomy with lymph nodes dissection is the mainstay treatment, even in metastatic disease. There are no established guidelines, nor is shown a benefit from chemotherapy in renal SCC. The management is case by case and is still depending on case reports. Overall prognosis remains dismal.
References
- Jain A, Mittal D, Jindal A, Solanki R, Khatri S, et al. (2011) Incidentally detected squamous cell carcinoma of renal pelvis in patients with staghorn calculi: Case series with review of the literature. ISRN Oncol 2011: 620574.
- Karabulut A, Emir L, Gonultas M, Incel N, Germiyanoğlu C, et al. (2002) Squamous cell carcinoma located in the renal caliceal system. A case report and review of the literature. Turkish J of Cancer 32: 20-24.
- Talwar N, Dargan P, Arora MP, Sharma A, Sen AK(2006) Primary squamous cell carcinoma of the renal pelvis masquerading as pyonephrosis: a case report. Indian Journal of Pathology and Microbiology 49: 418–420.
- Odabas O, Karakök M, Yılmaz Y, Atilla MK, Akman E,et al. (2000) Squamouscell carcinoma of the kidney. Eastern J of Medicine5:35-36.
- Bandyopadhyay R, Biswas S, Nag D, Ghosh AK (2010) Squamous cell carcinoma of the renal pelvis presenting as hydronephrosis. J Cancer ResTher6:537-e539.
- Holmang S, Lele SM, Johansson SL (2007) Squamous cell carcinoma of the renal pelvis and ureter: incidence, symptoms, treatment and outcome. J Urol 178: 51-56.
- Johansson S, Wahlqvist L (1979) A prognostic study of urothelial renal pelvic tumors: comparison between theprognosis of patients treated with intrafascial nephrectomy andperifascialnephrouretrectomy. Cancer 43: 2525-2531.
- Holmang S, Johansson SL (2006)Impact of diagnostic and treatment delay on survival in patients with renal pelvis and ureteral cancer. Scand J UrolNephrol 40: 479-484.
- Kimura T, Kiyota H, Asano K, Madarame J, Yoshino Y, et al. (2000) Squamous cell carcinoma of the renal pelviswith inferior vena caval extension. Int J Urol7:316-320.
- Blacher EJ, Johnson DE, Abdul-Karim FW, Ayala AG (1985) Squamous cell carcinoma of renal pelvis. Urology 25:124-126.
- Booth CM, Cameron KM, Pugh RC (1980) Urothelial carcinoma of the kidney and ureter. Br J Urol 52: 430-435.
- Sahoo TK, Das SK, Mishra C, Dhal I, Ali I, et al.(2015) Squamous cell carcinoma of kidney and its prognosis: a case report and review of theliterature. Case Rep Urol2015: 469327.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences