ISSN : 2576-3938
Journal of Emergency and Internal Medicine
Rapid Response System with Organized Response Team and Non-organized First Responders Using In-hospital Whole Paging
Department of Critical Care and Emergency center, Yokohama City University Medical Center, Japan
- *Corresponding Author:
- Yoshihiro Moriwaki
MD, PhD, Department of Surgery, Unnan City Hospital
96-1 Daito-Cho Iida, Unnan 699-1221, Japan.
Tel: 0854-47-7500
Fax: 0854-47-7501
E-mail: yoshimoriwaki@gmail.com
Received Date: July 07, 2018; Accepted Date: July 31, 2018; Published Date: August 05, 2018
Citation: Moriwaki Y, Sugiyama M, Tahara Y, Iwashita M, Arata S, et al. (2018) Rapid Response System with Organized Response Team and Non-organized First Responders Using In-hospital Whole Paging. J Emerg Intern Med. Vol.2:No.2:22.
Abstract
Our unique rapid response system (RRS) includes a systematically organized structure by rapid response teams (RRT) and a nonorganized, nonsystematic structure for gathering hospital staffs in the scene. We examined the records of 54 patients described in this RRS. Our RRS is as follows; a medical/non-medical hospital staff who finds a victim, asks other staffs to activate the RRS by using inhospital whole paging system; predefined staffs bring predefined equipments; a standard educational course and e-learning system and a simple recording form. The mean interval between the event and the arrival of staff at the scene was 1.81 minutes. Hospital death rate per total discharged patients tended to decrease after RRS. Our unique RRS work well. The death rate among discharged patients decreased after this system was implemented.
Keywords
Emergency medical service; Diagnostic and treatment
Introduction
Although many countries have established well-organized out-ofhospital emergency medical service (EMS) systems [1], it is well known that hospitals do not have comparable systems set up for emergencies involving inpatients in hospitals. The International Liaison Committee on Resuscitation (ILCOR), the European Resuscitation Council, the American Heart Association, and other associations have recommended guidelines for monitoring, reporting, and conducting research on medical emergency teams (MET), critical care outreach teams (CCOT), and rapid response teams (RRT) as well on systems that include such teams [2]. They emphasized not only the importance of establishing such special organized teams, but also the importance of the appropriate composition and availability of these teams, the criteria for their use, education and awareness of hospital employees, and methods of activating or contacting these teams under the "rapid response system" (RRS) label. However, it is often difficult to apply these standard RRSs because hospitals have varying characteristics and capabilities. Each hospital therefore needs to construct its own individual RRS. We have established a unique and original RRS, constructed from two different systems, using an in-hospital whole paging system. This RRS is comprised of an organized and systematic structure for activating RRT members, and a non-organized and nonsystematic structure to assemble doctors and nurses at the scene who are trained in providing only basic life support (BLS). This BLS training is provided as part of the standard educational course in the hospital. The objective of this study is to clarify the usefulness and problems of this unique RSS.
Materials and Methods
We examined the records for the past 2.5 years of all patients who were treated by our RRS and, if they were admitted, their medical records including their background, witness and firstresponder staff information (name and medical training), staff who were aware of the event and who called RRT, the area where the event occurred, and the definitive diagnosis and prognosis. We also compared the death rate among discharged patients as a whole before and after the establishment of the RRS.
Rapid Response System (RRS)
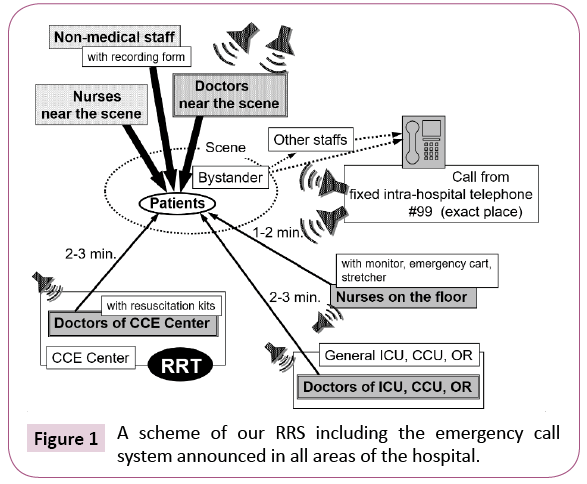
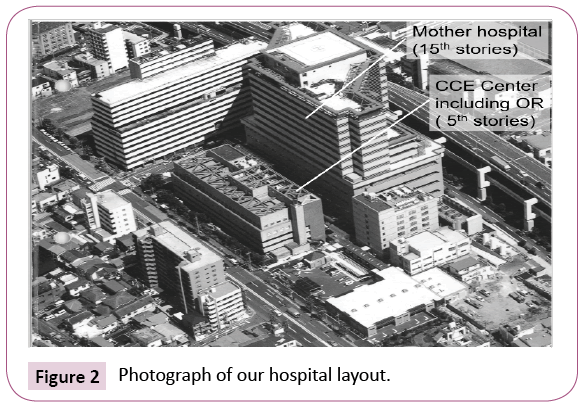
This RRS works as follows. A member of the hospital staff (medical or non-medical) who finds a collapsed patient or visitor or a patient or visitor requiring urgent medical support asks another staff member to activate the RRS by using the nearest fixed hospital phone to dial the in-hospital whole paging system. An emergency call is then announced in all areas of the hospital (Figure 1). The staff of the Critical Care and Emergency Center (CCE Center) then bring an Automated External Defibrillator (AED) and a standard bag usually brought to emergencies whether in or out of hospital, which contains the minimum necessary instruments to treat one critically injured person. Other staff members near the scene, usually nurses, bring monitors, oxygen, an emergency cart and a stretcher. Our hospital is so small (Figure 2) that the CCE Center staff individually go to the scene directly from wherever they are in the hospital working or preparing, rather than assembling as a team and then going together.
In 1990, our hospital established a preliminary emergency call system using in-hospital whole paging, which allowed hospital staff and medical doctors to be quickly assembled. Under this system, the CCE Center staff, as well as the staff members of the general ICU and CCU, went to the emergency scene as a voluntary and non-organized RRT in response to an emergency call. However, when we first implemented this call system, we were not aware of the importance of establishing an organized RRT, the composition and availability of this team, calling criteria, and education and awareness of hospital staff for BLS and basic resuscitation skills. In 2005, our committee for an in-hospital EMS system implemented this emergency call system as a regular and organized RSS, and the committee wrote a practical manual to use this unique and original call system.
Before this emergency call system was established, the physician in charge of the patient or the ward was the first staff person called by a fixed telephone when the critical event occurred, followed by anesthetists in the operating room, and finally the staff members of the general ICU. Because doctors did not then have mobile in-hospital telephones, it sometimes took several minutes for them to learn about a critical event. Additionally, it was impossible to inform more than one doctor about the event simultaneously. Moreover, due to reasons having to do with Japanese culture, we were embarrassed or even ashamed to ask for help and activate a help call.
When we started using this hospital emergency call system, the system had no recording capability. We documented the event, findings, and interventions in the medical records only if the patient was admitted to the hospital’s CCE Center. We could not document this information for patients who were already patients in our hospital when the emergency call system was activated, and could not start a medical record for a patient if the patient did not want any medical consults. We therefore could not evaluate and analyze our system during that period. The recording form still in use includes the date and time of team activation, patient category, the location of the event, the primary reason for team activation, and the patient's clinical status (free description) at the time of team activation as preevent data (Table 1). Non-medical office workers go to the scene and complete the form with information from medical staffs on the scene. We have established a standard educational course for BLS and basic resuscitation skills, and hold these courses regularly once or twice a month under management of the committee for the in-hospital EMS system. Since 2007, we have also been using an e-learning system for self-education, as a supplement to the standard educational classes.
| Date, time of the event |
| Place of the event |
| Witness of the event |
| Time of emergency call and caller of emergency call |
| Patient data; |
| I. Name, age, sex |
| II. Inpatients or not, ID and department he/she consulting |
| Type of the event and condition of the patient (Free description) |
| Time of arrival of the first responding doctor (Department) |
| Area where the patient was transferred |
| Clinical course including monitoring and interventional process |
| Outcomes |
| Comments (Free description) |
Table 1: Headings of our A4-sized recording form.
Results
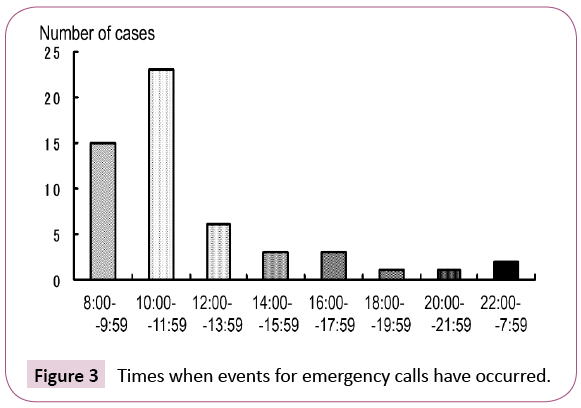
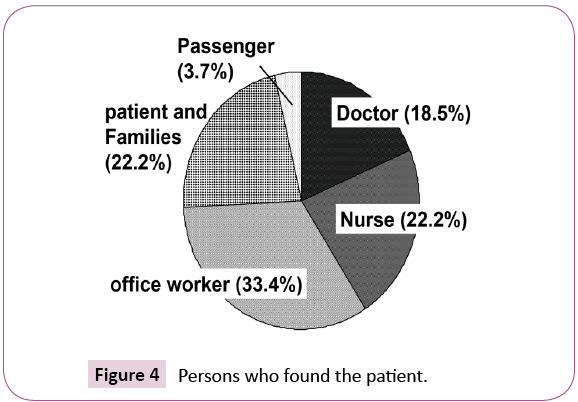
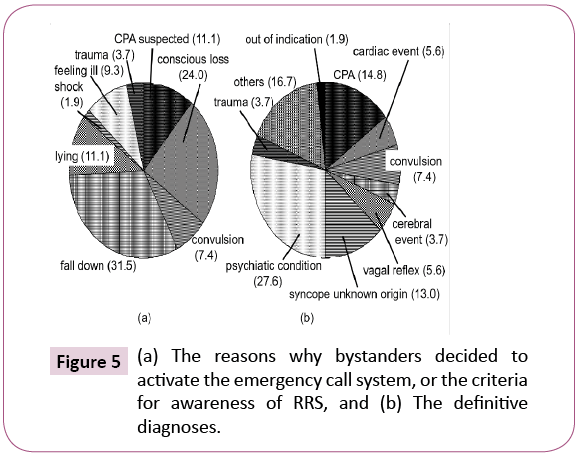
The data on 54 cases were reviewed. Many events requiring emergency calls occurred in the morning (Figure 3). The events mainly occurred in diagnostic and treatment rooms, waiting areas, examination rooms for blood sampling or x-ray examination in the outpatient department (55%), or in other non-medical areas such as waiting halls, corridors, and shops, (22%); 5% of the events occurred in the laboratory. Events seldom occurred in the critical care area (2%). Seventy-four percent of patients were found by hospital staff such as doctors and nurses, and 22% by patients and visitors. At the time of the emergency calls, 19% of these patients were being managed at the time by a doctor standing by (Figure 4). The reasons why bystanders decided to activate the emergency call system, or the criteria for awareness of RRS, were suspected cardiac arrest in 11% of patients, loss of consciousness in 24%, witnessing a fall in 31%, and lying on the ground in 11% (Figure 5a). The mean interval between the event and emergency call was 0.94 minutes, and that between the event and arrival of responding staff at the scene was 1.81 minutes.
The definitive diagnoses were cardiopulmonary arrest (CPA) in 15% of the patients, a cardiac event in 6%, a psychiatric condition in 28%, and out of indication such as simple requests from families in 2% (Figure 5b). In eight CPA cases, 38% survived-todischarge. One was identified as out of indication for resuscitation because of DNAR during activity, 1 case died of acute aortic dissection with cardiac tamponade in the outpatient department of cardiovascular surgery, and 2 of acute myocardiac infarction in the waiting room of the orthopedic outpatient department.
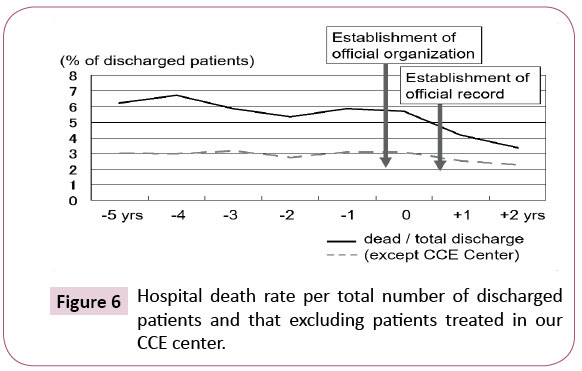
CCE Center staff (RRT) responding to the emergency call managed 50% of the patients within 1.1 minutes and, and the RRT arrived within 3 minutes for 93% of the them and then took over their management. Doctors in departments other than the CCE Center, such as the coronary care unit (CCU) and general intensive care unit (ICU), managed 37% of the patients. Both the hospital death rate per total discharged patients and that excluding patients treated in our CCE Center tended to decrease after this system was officially organized in the hospital (Figure 6).
Discussion
ILCOR's guidelines for resuscitation recommend the introduction of a RRS [3], with the intent to improve the quality of care of critically ill inpatients and to prevent adverse outcomes among them [4-9]. ILCOR also stated the importance of appropriate monitoring and accurate documentation of abnormal physiology of patients before, during, and after RRT activity [2]. They established a consensus on documentation similar to the Utstein-Style guidelines. However, many authors have reported that these physiological measurements are usually not made or recorded during this critical time of clinical deterioration [7,10- 12]. Hospital setups and medical infrastructures vary in different countries or regions [1,13]. In Japan, for example, hospitals are very small and compact, usually occupying just one or few buildings. The hospital staff spends much of their workday managing the outpatient departments, and there are many outpatients and visitors during the day. The members of the RRT do not need to meet together at a specific location to go as a team to the scene of the emergency, but instead proceed directly there, which saves precious time. Throughout the day, there are doctors usually working in critical care areas, and these doctors can quickly and adequately respond to critical events in these areas, forming a self-RRT. Thus, doctors and nurses in the critical care area do not usually need to call other RRTs. The RRS we use was established based on these conditions. We should consider the conditions specific to each country in order to improve the system of recording emergency events.
Our RRS is unique because it is composed of two different systems. One system is well organized and is comprised of the systematic gathering of doctors, nurses, and non-medical staff with predefined roles and instruments to carry, who are well trained in BLS, critical care and resuscitation skills and they are trained in a dynamic team approach. The other is a non-organized system in which any doctor and nurse near the scene, who do not have predefined roles or instruments to carry, and who are only trained in BLS in the hospital's standard educational course, respond to the emergency call. This concept behind this system is the same as that used by out-of-hospital emergency responders.
The advantages of having a non-organized component of a RRS are: 1) treatment by non-medical and medical staff is begun earlier; 2) more people are available not only to treat the patient, but also to transfer the patient, to communicate with family members and/or other staff, and to disperse a crowd, and 3) joint efforts by nonspecialists are implemented. In terms of effectiveness, we consider the non-organized part of this RRS to be more effective than the response by a layperson in out-of-hospital medical emergency events, but less effective than a response by an organized EMS. There are few reports on the interval in RRT from the event to the start of evaluation and care (BLS). Unfortunately, it is not possible to evaluate the effectiveness of our RRS from the standpoint of this interval because the structural conditions of our hospital and our RRS are unique [14-16]. Although some authors have reported that the time interval from the alert to the arrival of intensivist was longer than the interval in our data, our hospital is much smaller in size, and number of buildings, than the hospitals in these studies.
Because the first evaluation and care in this system are performed by non-organized individuals who are not well trained, the quality of the evaluation and care they perform is questionable. We have been trying to educate both our medical and non-medical staff in BLS and resuscitation skills via the monthly standard educational course and the e-learning system mentioned above. We have found that nurses and non-medical staff have been willing to participate in these educational courses, but that very few doctors have taken an interest. We need to encourage doctors to learn BLS using the e-learning system, because they can study on their own time. We have also encouraged them during several in-hospital meetings for the doctors on such subjects as risk management, safety management, and management of emergency department. However, we are not yet able to discuss how effective these educational plans have been.
Other disadvantages of the non-organized component of our RRS are as follows: 1) non-organized doctors and nurses may become passive crowd, and think that someone else will perform BLS; 2) there may be no leader and no command system; 3) too many persons on the scene may get in the way or obstruct care; 4) we currently have no way to provide first responders with adequate feedback on the effectiveness of this system, and 5) non-organized responders must stop their routine clinical work when the doctors they are working with, particularly the specialists, respond to an emergency call. We are attempting to teach the importance of leadership and of command systems in the monthly standard educational course and e-learning system, and plan to communicate adequately and for a long time with non-organized responders after the event.
We encountered some resistance by physicians in the course of establishing this RRS. Some specialist physicians felt that they had insufficient resuscitation skills and that emergency calls should therefore go directly to the RRT. They felt that they could not perform effectively at the scene before the RRT arrived, and that other patients might be disturbed by the whole in-hospital paging system, particularly at night. We reached a compromise with them in a meeting of the committee for the in-hospital EMS system. Emergency calls would be announced from speakers in all parts of the hospital except patients' bedrooms and hallways in the wards at night. However, because of this compromise, doctors attending to patients in their bedrooms are not alerted to emergencies by the call system.
Conclusion
Although a tendency toward a decreasing hospital death rate per discharged patient was demonstrated in this study, many factors besides RRS strongly affect this endpoint. ILCOR guidelines state that outcome information is one of the core data elements, and defined it as the absolute minimum required for continuous quality improvement, vital for accurately tracking process and outcome variables. However, it is sometimes difficult to differentiate between expected and unexpected deaths, and between preventable and non-preventable deaths. The expectation of death or the existence of an unrecoverable condition affect the treatment strategy and may increase mortality. Additionally, the RRT must sometimes attend a patient for whom CPR has been ruled out. These are limitations on the evaluation of the effect of RRS using the death rate. We need to identify more appropriate parameters indicating the effect of RRS.
References
- Moriwaki Y, Sugiyama M, Hayashi H, Mosiello G, Cremonese F, et al. (2001) Emergency medical service system in Yokohama, Japan. Annali Degli Ospedali San Camilloe Forlanini 3: 344-356.
- Peberdy MA, Cretikos M, Abella BS, DeVita M, Goldhill D, et al. (2007) Recommended guidelines for monitoring, reporting, and conducting research on medical emergency team, outreach, and rapid response systems. Resuscitation 75: 412-433, Circulation 116: 2481-2500.
- International Liaison Committee on Resuscitation (2005) Part 4: Advanced life support. Resuscitation. 67: 213-247.
- Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, et al. (2002) Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ 324: 387-390.
- Braithwaite RS, DeVita MA, Mahidhara R, Simmons RL, Stuart S, et al. (2004) Medical Emergency Response Improvement Team (MERIT) Use of medical emergency team (MET) responses to detect medical errors. Qual Saf Health Care 13: 255-259.
- DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, et al. (2004) Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care 13: 251-254.
- MERIT Study Investigators (2005) Introduction of the Medical Emergency Team (MET) system: A cluster-randomised controlled trial. The Lancet. 365(9477): 2091-2097.
- Jones D, Opdam H, Egi M, Goldsmith D, Bates S, et al. (2007) Long-term effect of a Medical Emergency Team on mortality in a teaching hospital. Resuscitation 74: 235-241.
- Buist M, Harrison J, Abaloz E, Van Dyke S (2007) Six years audit of cardiac arrests and medical emergency team calls in an Australian outer metropolitan teaching hospital. BMJ 335: 1210-1212.
- Hall S, Williams E, Richards S, Subbe C, Gemmell L (2003) Waiting to exhale: critical care outreach and recording of ventilatory frequency, Br J Anaesth 90: 570-571.
- Hodgetts TJ, Kenward G, Vlachonikolis LG, Payne S, Castle N (2002) The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation 54: 125-131.
- McBride J, Knight D, Piper J, Smith GB (2005) Long-term effect of introducing an early warning score on respiratory rate charting on general wards. Resuscitation 65: 41-44.
- Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE (2004) International Liason Committee on Resusitation.. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa), Resuscitation 63: 233-249.
- Tee A, Calzavacca P, Licari E, Goldsmith D, Bellomo R (2008) Bench-to-bedside review: The MET syndrome - the challenges of researching and adopting medical emergency teams. Crit Care 12: 205.
- Young L, Donald M, Parr M, Hillman K (2008) The Medical Emergency Team system: A two hospital comparison. Resuscitation 77: 153-154.
- Downey AW, Quach JL, Haase M, Haase-Fielitz A, Jones D, et al. (2008) Characteristics and outcomes of patients receiving a medical emergency team review for acute change in conscious state or arrhythmias. Crit Care Med 36: 477-481.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences