Preventing Alloimmunization in the Trauma Setting: A Case Report and Development of a ultidisciplinary Protocol
Meghan Munisteri*, Rebecca Wong and Veronica Gonzalez Brown
Department of Obstetrics and Gynaecology, Brooke Army Medical Center, San Antonio, USA
- *Corresponding Author:
- Meghan
Munisteri
Department of Obstetrics and Gynaecology,
Brooke Army Medical Center,
San Antonio, USA,
Tel: 6317072725;
E-mail: megmunisteri@gmail.COM
Received Date: November 04, 2021; Accepted Date: November 18, 2021; Published Date: November 23, 2021
Citation: Munisteri M, Wong R, Brown VG (2021) Preventing Alloimmunization in the Trauma Setting: A Case Report and Development of a Multidisciplinary Protocol. J Women’s Health Reprod Med Vol. 5 No. 6:23.
Abstract
Background: Casualties with haemorrhagic shock resuscitated with whole blood showed improved survival compared to individual components. Low Titer Group-O Whole Blood (LTOWB)/preferred fluid resuscitation in combat and trauma in the U.S. LTOWB have potential to sensitize women to RhD antigen, complicating future pregnancies.
Case: Female polytrauma received unit of RhD-positive Low Titer Group-O Whole Blood enroute to hospital. Evaluation confirmed positive pregnancy. Care coordinated by multidisciplinary team consisting of OBGYN, Trauma, Pathology, and Hematology to prevent alloimmunization. Protocol preventing maternal alloimmunization in the setting of trauma developed.
Conclusion: Low Titer Group-O Whole Blood in RhD negative women of reproductive age highlighting importance of utilizing multidisciplinary approach to coordinating care and preventing maternal alloimmunization. Where alloimmunization is unable to be prevented, it’s important to educate about implications of care and risks to future pregnancies.
Keywords
Haemorrhage; Pregnancy; Women; Traumatic injury
Introduction
The first successful transfusion of human blood was in an obstetrical patient for the treatment of postpartum haemorrhage [1]. Haemorrhage has long been the most common cause of maternal death in the United States; haemorrhage is also the most common cause of death after traumatic injury. Whole blood has been the primary resuscitation fluid for the U.S. military in combat settings since World War I, and its popularity has seen a resurgence after a 2009 study of U.S. military combat casualties with haemorrhagic shock found resuscitation with whole blood was associated with improved 30-day survival compared to the use of individual components. Even in the civilian sector, haemorrhage remains the second most common cause of preventative death after traumatic injury, and it is estimated that between 10,000 and 24,000 potentially preventable haemorrhagic trauma deaths occur annually in the United States [2,3]. Early identification of patients at risk of coagulopathy bleeding and prompt initiation of pre-hospital transfusion are critical, as haemorrhagic deaths typically occur within the first 24 hours [2].
In 2018, The Department of Defence Joint Trauma System and Committee on Tactical Combat Casualty Care developed the Advanced Resuscitative Care guidelines. The document emphasizes the concept of the “Golden Hour,” in which a patient should be evacuated to a surgical treatment facility within 60 minutes, as this has been shown to reduce pre-hospital deaths among US combat casualties from 16.0% to 9.9% [4]. The new guidelines also encourage the use of Low Titer Group O Whole Blood (LTOWB) as first-line resuscitation fluid [4,5]. Texas Regional Advisory Council (STRAC) implemented LTOWB as the primary pre-hospital resuscitative fluid in South Texas. LTOWB is unseparated blood with low IgM and/or IgG anti-A and anti-B; however, there are no universal parameters defining “low” titer cut-offs. LTOWB parameters are defined by the as IgM anti-A and anti-B <256 [6].
Of concern is the use of RhD-positive LTOWB, which has the potential to sensitize Rh-negative women of childbearing age to the RhD antigen, complicating future pregnancies. Exposure to the RhD antigen on transfused erythrocytes stimulates the maternal immune system, ultimately producing B lymphocytes with memory of the antigen. If an RhD-negative patient is exposed to the RhD antigen; whether on fetal erythrocytes or on transfused RBCs, maternal plasma cells will proliferate and produce IgG antibodies that cross the placenta, ultimately resulting in fetal anaemia [7]. Antenatal and postpartum use of Rh immune globulin has significantly decreased the incidence of haemolytic disease of the foetus or new-born in industrialized countries. Developing countries without Rh immune globulin prophylaxis programs still have stillbirth rates of 14% in affected pregnancies. Among those infants who survive the pregnancy, 50% either die in the neonatal period or develop cerebral injury [8].
The practice of RhD positive whole blood as the primary prehospital and combat resuscitation fluid will become of increasing importance in the U.S. military as the number of active duty women continues to rise, currently reported at 16.9% [9]. Identification of RhD negative women and prompt utilization of anti-D immune globulin for prevention of D alloimmunization is crucial to avoid complications with any future transfusions, as well as haemolytic disease of the foetus and new-born in women with future childbearing potential. Haemorrhagic deaths typically occur within the first 24 hours [2]. In 2018, The Department of Defense Joint Trauma System and Committee on Tactical Combat Casualty Care developed the Advanced Resuscitative Care guidelines. The document emphasizes the concept of the “Golden Hour,” in which a patient should be evacuated to a surgical treatment facility within 60 minutes, as this has been shown to reduce pre-hospital deaths among US combat casualties from 16.0% to 9.9%. The new guidelines also encourage the use of Low Titer [4].
Case Presentation
A 15-year-old female unrestrained driver involved in a high-speed collision trauma. Enroute to Military Trauma Center, she received one unit of RhD-positive LTOWB and 2 grams of tranexamic acid, and her total transport time to the hospital was approximately 20 minutes. Her trauma evaluation was significant for grade 2 liver lacerations, multiple dissection of the thoracic and abdominal aorta as well as multiple orthopedic injuries. On arrival to the trauma bay, she received an additional two units of RhD-negative RBCs, followed by two units of group A plasma and cryoprecipitate intraoperative. During her evaluation, she was confirmed to have a positive pregnancy test. A type and screen sample was sent to the blood bank returned inconclusive due to the multiple blood transfusions and mixed field. She was typed as 2+ mixed field with anti-A and anti-D reagents, and her reverse typing was positive only with the B reagent RBCs. Given the patient was a female of reproductive age with a positive pregnancy test; OB/ GYN was consulted for guidance regarding the prevention of maternal alloimmunization. The remainder of her resuscitation was completed with O RhD-negative RBCs. Patient’s care was coordinated by a multidisciplinary team consisting of OBGYN, Trauma, Pathology, and Hematology. The team decided to proceed with administration of Rh immunotherapy. The quantity of residual RhD-positive RBCs in circulation was calculated to determine the dose of intravenous (IV) Rhogam. Patient was treated with 3000 IU IV Rhophylac every 8 hours to achieve the dose required to prevent alloimmunization.
Results and Discussion
Whole blood has been the primary resuscitation fluid for the U.S. military in combat settings since World War I; however, its popularity had declined as civilian trauma centres transitioned into component therapy. The popularity of Whole Blood has seen resurgence after the recent conflict in Iraq and Afghanistan yielded literature noting the benefits of Whole Blood resuscitation over component therapy and the importance of early resuscitation [10]. Analysis of the Combat Casualty Care data done by Howard, et al. noted 19.4% of casualties during the conflict in Afghanistan required a blood transfusion [11]. Upon further analysis of the data, approximately 2% of the causalities and wounded from 2001-2017 were females of childbearing age [12]. It can be inferred that future data collection may reflect higher female percentages due to the incorporation of female into combat roles in 2015. The benefits of early resuscitation and prehospital LTOWB transfusion have been well described in the literature, but these benefits are not without associated risks [3-5]. In all patients, regardless of gender, whole blood transfusion can be associated with risk of transfusion related acute lung injury and ABO incompatibility haemolysis. These risks can be mitigated if appropriate steps are taken to screen donor blood for human neutrophilic or leukocytic antibodies, as well as only using male and females that have negative antibody testing.
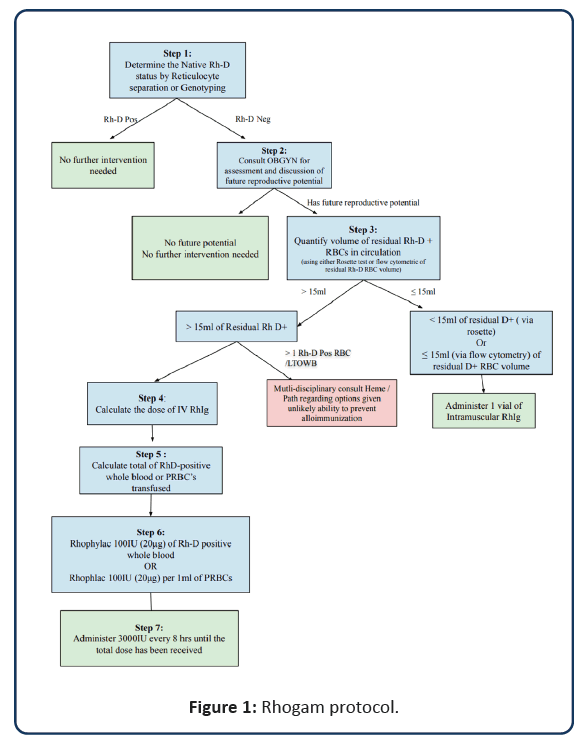
The risk posed by transfusion mismatch in women of reproductive age may lead to the formation of maternal alloimmunization. Undiagnosed and untreated, alloimmunization can lead to significant perinatal morbidity and mortality not only in a current pregnancy but also in all future pregnancies [7,8]. Given the risks associated with transfusing RhD-positive LTOWB to women of childbearing age, it is crucial that facilities have Rh immunoprophylaxis protocols in place to prevent alloimmunization, to include education and follow up for patients in which alloimmunization cannot be prevented. This is of particular importance in military medicine where whole blood is the resuscitation fluid of choice in the combat setting. San Antonio Military Medical Centre is the only Level 1 Trauma Centre in the Department of Defence accepting military and civilian patients from the surrounding areas. Our team set out to develop a protocol involving a multidisciplinary approach to standardize and streamline the care for prevention of maternal alloimmunization in the setting of whole blood transfusion in unknown Rh status (Figure 1). This protocol was designed to improve staff readiness, minimize [10] risks, and streamline care processes when a female patient of reproductive age arrives to our facility and has received Rh mismatch transfusion or Rh status is unknown. This is a suggested protocol which may not be applicable to all health care settings but can be adapted to local resources and limitations of individual facilities.
Conclusion
This case describes the multifactorial complexity of the transfusion of LTOWB in RhD negative or unknown Rh status women of reproductive age and prevention of maternal alloimmunization. This case also highlights the importance of utilizing a multidisciplinary team to expeditiously coordinate care and prevent maternal alloimmunization. Even in cases where alloimmunization 180 is unable to be prevented, we found that it is important to educate patients about the implications 181 of their care and risks to future pregnancies.
References
- Rimar Y (2005) The history of blood transfusions Harefuah 144(4):296-299.
- Gurney JM, Spinella PC (2018) Blood transfusion management in the severely bleeding military patient. Curr Opin Anaesthesiol 31(2):207-214.
- Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB (2009) Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma 66(4):69.
- Butler FK, Holcomb JB, Shackelford S, Barbabella S, Bailey JA, et al. (2018) Advanced resuscitative care in tactical combat casualty care: TCCC guidelines change. Journal of special operations medicine: a peer reviewed J Spec Oper Med 18(4):37-55.
- Bahr M, Cap AP, Dishong D, Yazer MH (2020) Practical considerations for a military whole blood program. Mil Med 185(7):1032-1038.
- Yazer MH, Jackson B, Sperry JL, Alarcon L, Triulzi DJ, et al. (2016) Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. J Trauma Acute Care Surg 81(1):21-26.
- Journal of Trauma and Acute Care Surgery (2016)81(1).
- American College of Obstetricians and Gynecologists (2018) ACOG practice bulletin no. 192: management of alloimmunization during pregnancy. Obs Gyn 31(3):82-90.
- Department of Defence demographics: Profile of the military community.
- Tucker RP (2019) Suicide in transgender veterans: Prevalence, prevention, and implications of current policy. Perspect Psychol Sci 14(3):452-468.
- Spinella PC, Cap AP (2016) Whole blood: Back to the future. Curr Opin Hematol 23(6):536-542.
- Howard JT, Kotwal RS, Stern CA, Janak JC, Mazuchowski EL, et al. (2019) Use of combat casualty care data to assess the US military trauma system during the Afghanistan and Iraq conflicts. JAMA Surg. 154(7):600-608.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences