Premaling Pathology of Esophagus: Esophageal Melanocytosis
Sabahattin Destek1* and Onur Vahit Gul2
1Department of General Surgery, Bezmialem Vakif University, Istanbul, Turkey
2Department of General Surgery, Gülhane Education and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Dr. Sabahattin Destek
Department of General Surgery
Medical Faculty, Bezmialem Vakif University
Istanbul, Turkey
Tel: +902125232288
E-mail: drsdestek@yahoo.com
Received Date: November 22, 2017; Accepted Date: November 29, 2017; Published Date: December 10, 2017
Citation: Destek S, Gul OV (2017) Premaling Pathology of Esophagus: Esophageal Melanocytosis. Gen Surg Rep. Vol.1 No.1:5
Abstract
Esophageal melanocytosis (EM) is caused by melanocytic cell proliferation in the squamous epithelium of the esophagus. Rare and etiology is not fully known. Usually EM is accepted as benign. However, some researchers assume that EM is the pioneer of primary oesophageal melanomas. In this article; After our endoscopic and pathologic evaluations; We aimed to report two female patients aged 55 and 53 years who underwent EM diagnosis and were endoscopically followed for the risk of developing malignancy.
Keywords
Esophageal melanocytosis; Esophagus; Premaling pathology
Introduction
Esophageal melanocytosis (EM) was first described by De la Pava in 1963 [1]. EM is a rare benign disease characterized by melanocytic proliferation of squamous epithelium of the esophagus and melanin deposition in the mucosa. Normally, the esophagus mucosa does not contain melanocytes. However, it is suggested that the melanoctyes result from the differentiation of stem cells in the basal layer due to the chronic inflammative and aberrant melanocyte migration or reflux esophagitis (RE) during embryogenesis [2]. Although EM is accepted as benign in general, some studies report it as the precursor lesion of primary esophageal melanoma and can be found along with esophageal malignancy [1,2]. They are rare and they are determined on 0.07% to 2% of upper gastrointestinal endoscopies. It is more frequently reported in autopsy series (2). In this case report, we review a case of EM with reference to the literature.
Case Presentation
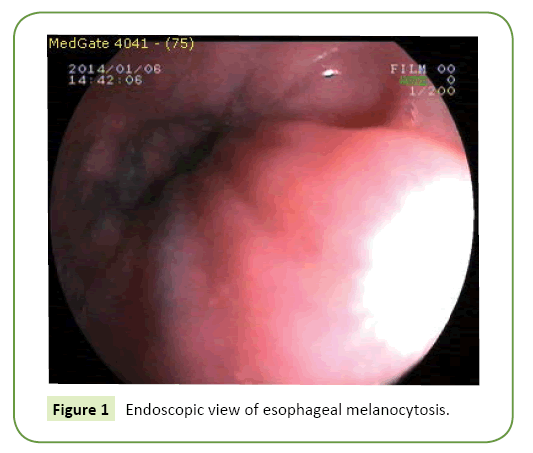
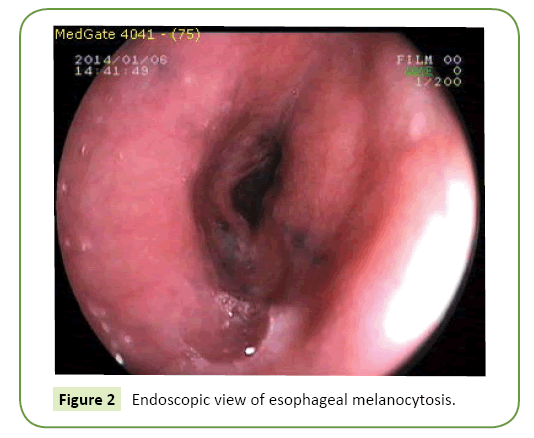
Our first patient 54; Our second patient was 53 years old. Both of our patients presented with intermittent symptoms of water brash, dysphagia, dyspepsia and epigastric pain for approximately 5 years. Both patients had never used alcohol or cigarettes before. They are usually fed with animal nutrients. Endoscopy was not performed in both patients before. At the endoscopy of our first patient, linear melanocytosis regions between 20-30 cm on esophagus, RE (Los Angeles grade B), alkaline reflux pangastritis, duodenitis were determined. At the endoscopy of our second patient, linear multiple melanocytosis regions between 25-30 cm on esophagus, RE (Los Angeles grade B), pangastritis, duodenitis were determined (Figures 1 and 2). EM revealed dark-colored (brown and black), linear, punctuate various shapes, and varying sizes, between 2 and 10 mm, of flat hyper pigmentation focuses. Multiple biopsies were conducted. In both cases, Helicobacter pylori urease test was (+). Biochemical tests were normal. There was no pathology in the radiological examinations such as thorax x-ray and abdominal sonography.
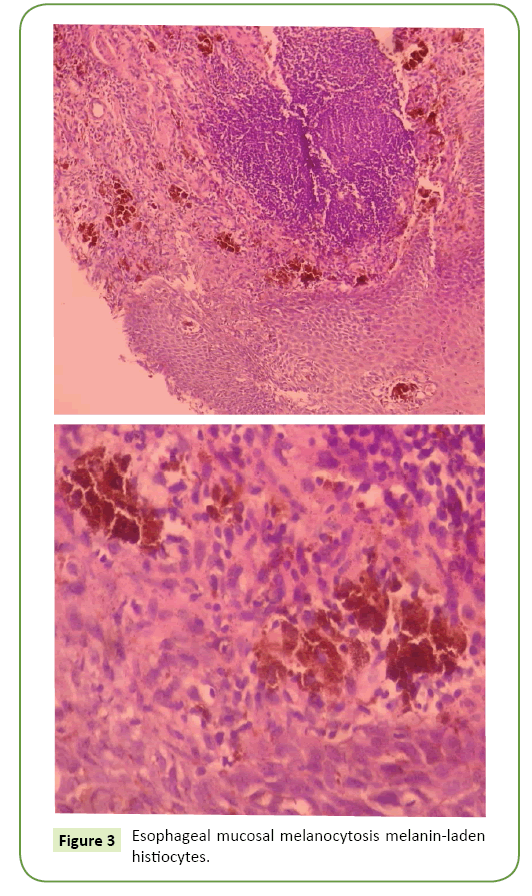
EM was determined in histopathological examination. Condensed lymphocytic infiltration in the supportive tissues belonging to lamina propria located under squamous trait acanthotic and intercellular edemas were observed covering the laminated epithelium. Numerous condensed melanin-laden histiocytes were detected in the histopathologic examination (Figure 3). Few melanocytes were observed in the esophagus basal layer. Chronic esophagitis resembling RE and HP (+) chronic pangastritis was detected. Anti-reflux and HP eradication therapy were provided and the patients were treated. As a maintenance therapy, patients were treated with a proton pump inhibitor and a reflux diet. After one year endoscopy and histopathological examination results were stable. Every year a control endoscopy is planned (That patient's written consent form was obtained).
Discussion
The process of melanocytogenesis in normal skin prevents the damage of intracellular lipids, proteins, and nucleotides by neutralizing reactive oxygen molecules. Melanocytogenesis also functions as an antioxidant defense barrier in the upper GIST [2]. Smoking causes chronic destruction of mucosa in the upper GIST. It is stated that approximately 20% of the smokers in Western and Asian societies have “smoker’s melanocytosis” in their mucosas [3]. Another report from Iran showed the presence of EM in a patient smoking opium [4]. Factors affecting epithelial proliferation causing chronic reflux esophagitis increase melanocytogenesis in the upper GÄ°S. The rate of EM occurrence is 7% in endoscopic findings, which was observed among alcoholic males in Japan [5]. In previous researches; melanocytes were found in the epithelio-stromal junction in 7.7% of normal oesophagus specimens examined at autopsy, and in 29.9% of surgical cases with oesophageal carcinoma [5]. There were no significant differences in incidence between males and females [5]. Multivariate analysis showed that older age, heavy smoking, and alcohol associated with the presence of melanocytosis [2,5]. Keratinocytes, which are reproduced by epithelial proliferation and stimulated by various factors, induce melanocytogenesis through autocrine and paracrine effects. Lifestyle habits such as chronic alcohol consumption, smoking addiction, and nutritional habits and hereditary factors can be related to melanocytogenesis progression because it is associated with neoplastic processes [2-5]. In the present case study, the patient had a nutritional habit mostly consisting of animal-origin foods and rarely vegetables, which could have affected EM.
EM frequently encompasses reactive epithelial changes such as chronic esophagitis, acanthosis, and basal cell hyperplasia upon microscopic examination [1,2]. Chronic esophagitis caused by chronic effects depending on the gastroesophageal reflux primarily increase the bile and gastric liquid reflux, probably causing EM [2]. In our case, Los Angeles grade B RE was detected upon endoscopic examination and esophagitis chronic esophagitis was also identified in the pathological examination. HP also affects EM via influencing esophageal squamous cell carcinoma by cellular destruction in the esophagus mucosa [6]. EM can be observed in combination with systemic diseases such as Laugier–Hunziker syndrome, Addison’s disease, gastroesophageal melanoma, and esophageal squamous cell carcinoma [2,7,8]. Ishida et al. showed that 3.8% of esophageal squamous cell carcinoma cases are implicated in melanocytosis and stated that the cause of melanocytosis could be chronic esophagitis as reported in other studies [2,9]. Primary malignant melanoma generally combines with melanocytosis [10]. Malignant melanoma and melanocytic nevus, in which melanin deposition occurs, should be considered in the differential diagnosis of EM. Primary malignant melanoma of esophagus constitutes only 0.1–0.2% of malignant esophageal tumors, which are frequently observed in the middle and lower esophagus as pigmented or unpigmented polypoid masses during endoscopy [9,10]. As for melanocytic nevus, it is very rare and no case has been reported till date [11].
Pigment deposition of anthracosis, hemosiderosis, or lipofuscin from other pigmented lesions and “black” esophagus combined with necrosis mostly occurs due to systematic reasons, which should be considered in the differential diagnosis [2,12]. Walter et al. detected chronic esophagitis and intraepithelial atypical melanocytic cell transformation in squamous cell in situ carcinoma in a patient who underwent transhiatal esophagectomy, which causes in situ melanoma. They further emphasized that esophageal melanocytosis should be considered in diagnosing the malignancy [13].
With the esophagus to follow the risk of developing malignancy; If there are no neoplastic changes such as metaplasia dysplasia in melanocytes, endoscopic control is sufficient once a year. However, if there is neoplastic change followed by shorter time intervals. According to the researches; routine endoscopic biopsy trauma is insignificant and does not cause harmful transformations [10,13].
Conclusion
EM is a rare disease accepted as benign with hyperpigmented lesions. Recent studies have reported that EM can be a precursor for malignancy. There are no studies supporting the local treatments, such as endoscopic mucosectomy and superficial resection of lesions, for selected endemic cases, which become practicable with recent technological developments in the field of medicine.
Radical esophageal surgery is not recommended because of the rather high rates of mortality and morbidity for a benign disease. Nevertheless, considering the reported cases, patients suffering from EM need to undergo frequent endoscopic and histopathologic examinations due to the suspicion of a potential malignancy precursor.
Conflict of Interest
The authors declare that they have no competing interests and any sources of funding for our publication.
References
- Kumari NS, Srujana S, Sireesha A, Krishna L, Kumar OS (2016) Esophageal melanocytosis-An unusual melanocytic entity. J Assoc Physicians India 64: 75-76.
- Chang F, Deere H (2006) Esophageal melanocytosis, morphological features and review of the literature. Arch Pathol Lab Med 130: 552-557.
- Unsal E, Paksoy C, Soykan E, Elhan AH, Sahin M (2001) Oral melanin pigmentation related to smoking in a Turkish population. Community Dent Oral Epidemiol 29:272-7.
- Geramizadeh B, Asadian F, Taghavi A (2014) Esophageal melanocytosis in oral opium consumption. Iran Red Crescent Med J 16: 7820.
- Yokoyama A, Mizukami T, Omori T, Yokoyama T, Hirota T, et al. (2006) Melanosis and squamous cell neoplasms of the upper aerodigestive tract in Japanese alcoholic men. Cancer Sci 97: 905-911
- Li WS, Tian DP, Guan XY, Yun H, Wang HT, et al. (2014) Esophageal intraepithelial invasion of Helicobacter pylori correlates with atypical hyperplasia. Int J Cancer 134:2626-2632.
- Moore RT, Chae KA, Rhodes AR (2004) Laugier and Hunziker pigmentation: A lentiginous proliferation of melanocytes. J Am Acad Dermatol 50:70-74.
- Jones BH, Fleischer DE, De Petris G, Heigh RI, Shiff AD (2005) Esophageal melanocytosis in the setting of Addison's disease. Gastrointest Endosc 61: 485-487.
- Ishida M, Mochizuki Y, Iwai M, Yoshida K, Kagotani A,et al. (2013) Pigmented squamous intraepithelial neoplasia of the esophagus. Int J Clin Exp Pathol 15: 1868-1873.
- Iwanuma Y, Tomita N, Amano T, Isayama F, Tsurumaru M,et al. (2012) Current status of primary malignant melanoma of the esophagus: clinical features, pathology, management and prognosis. J Gastroenterol 47: 21-28.
- Lam KY, Law S, Chan GSW (2001) Esophageal blue nevus: An isolated endoscopic finding. Head Neck 23: 506-509.
- Destek S, Gul VO, Ahioglu S, Erbil Y (2016) A rare disease of the digestive tract: Esophageal melanosis. Gastroenterol Res 9:56-60.
- Walter A, Van Rees BP, Heijnen BH, Van Lanschot JJ, Offerhaus GJ (2000) Atypical melanocytic proliferation associated with squamous cell carcinoma in situ of the esophagus. Virchows Arch 437: 203-207.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences