Pancreatic Neoplasms: A Diagnostic Dilemma
Sana Quadri, Sujata Patnaik*, Megha Uppin and Phani Chakravarthy
Department of Radiology, Nizam’s Institute of Medical Sciences, Hyderabad, India
- *Corresponding Author:
- Patnaik S
Department of Radiology, Nizam’s Institute of Medical Sciences
Punjagutta, Hyderabad, India
Tel: +91 9490793534
E-mail: sujata_patnaik222@yahoo.co.in
Received date: July 03, 2019; Accepted date: July 29, 2019; Published date: August 20, 2019
Citation: Quadri S, Patnaik S, Uppin M, Chakravarthy P (2019) Pancreatic Neoplasms: A Diagnostic Dilemma. Journal of Clinical Radiology and Case Report Vol.3 No.1:6
Copyright: © 2019, Quadri S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Context: Imaging of pancreas is a challenging situation. However rapid evolution of CT has enhanced the diagnostic accuracy many folds.
Aim: To determine the accuracy of Multi-Detector Computed Tomography (MDCT) in characterization of pancreatic masses and to correlate imaging findings with histopathological diagnosis.
Material and methods: This prospective study was carried out on patients in Nizam's Institute of Medical Sciences, Hyderabad from December 2016 to April 2018. A total of histopathologically proven 35 consecutive cases with primary pancreatic masses were analyzed.
Results: There were 17 males and 18 females with age range from 18 to 83 years. Maximum were in 4th to 6th decade. The final histopathology examination (HPE) diagnosis included adenocarcinoma in 24 (68%), solid pseudopapillary epithelial neoplasm (SPEN)-3 (8.5%),Neuroendocrine tumors (NET)-3 (8.5%), serous cyst adenoma-2 (5.7%), mucinous cyst adenoma-1 (2.8%), Intraductal Papillary Mucinous Neoplasm (IPMN)-1 (2.8%) and Gastrointestinal stromal tumor (GIST)-1(2.8%). There were 5 cases where the radiological diagnosis did not correlate with pathological diagnosis. Mimics of ductal adenocarcinoma are NET and cystic neoplasm in our series. The overall diagnostic accuracy of CT was 85%.
Conclusion: Pancreatic ductal adenocarcinoma is the most common malignancy followed by NET and cystic neoplasms. Though extremely rare, GIST can also occur. Overall, the CT has diagnostic accuracy of 85%. Since feasibility for resection and prognosis are different for each type of the tumors, definite early diagnosis is essential.
Keywords
Pancreatic neoplasms; Pancreas; Cancer; Radiology; Computed tomography
Introduction
Pancreatic cancer is the seventh most common leading cause of global cancer deaths in industrial countries and accounting for 4.5% of all deaths caused by cancer in 2018. It is the third most common cause of cancer death in USA [1]. Based on function, the pancreatic neoplasms are classified as exocrine and endocrine tumors. Exocrine tumors include ductal adenocarcinoma (99%), cystic neoplasms and intra-ductal papillary mucinous neoplasms. Endocrine tumors originate from islet cells. Now it is thought that these tumors arise from pluripotent stem cells in ductal epithelium [2]. The presentation of these tumors can syndromic or non-syndromic. The third type of tumours includes mesenchymal tumors arising from connective tissue, lymphatic vessels, and neuronal tissue of pancreas. Imaging of pancreas is a challenging situation. However rapid evolution of CT has enhanced the diagnostic accuracy many folds. In the recent years, large volume of coverage, multi-planner-reconstructions, and curved planner reconstructions helped in improved diagnosis and staging of tumors. CT scan has a sensitivity and specificity of 89% and 90% [3].
Aim and Objective
To determine the accuracy of Multi-Detector Computed Tomography (MDCT) in characterization of pancreatic masses and to correlate imaging findings with histopathological diagnosis.
Materials and Methods
This prospective study was carried out from December 2016 to April 2018. A total of histopathologically proven 35 consecutive cases with primary pancreatic masses were analyzed. Prior written consent was taken from the patients and their attendants after explaining the procedural aspects of the study to them. Subjects with clinical suspicion or sonological diagnosis of pancreatic tumors underwent CT studies which were performed using a 16 slice multi detector CT. Triple phase CT with oral and IV contrast study was done in all cases.
CT scans were reviewed to detect the pancreatic mass as well as to characterize them. Images were analyzed in terms of site, size, attenuation, enhancement pattern, local spread including vascular invasion and distant spread. Morphology of rest of pancreas, ductal dilatation and rest of the abdominal organs was also evaluated. Finally, radiological diagnosis was compared with histopathological diagnosis.
Results
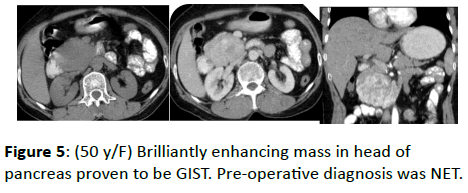
Total 35 HPE proven pancreatic tumors were analyzed. There were 17 males and 18 females with age range from 18 to 83 years. Maximum were in fourth to sixth decade (n=20) followed by second to fourth (n=7) and more than sixth decade (n=7). Only one case was 18-years female (Solid Pseudopapillary Epithelial Neoplasm). The radiological diagnosis was correlated with histo-pathological diagnosis. The final HPE diagnosis included adenocarcinoma in 24(68%), SPEN-3(8.5%), NET-3(8.5%), serous cystadenoma-2 (5.7%), mucinous cystadenoma-1(2.8%), IPMN 1 (2.8%) and Gastrointestinal stromal tumor (GIST) 1(2.8%). There were five cases where the radiological diagnosis did not correlate with pathological diagnosis (Table 1) (Figures 1-5). Mimics of ductal adenocarcinoma are NET and cystic neoplasm in our series. The overall diagnostic accuracy of CT was 85%.
| Case number | Radiological diagnosis | Pathological diagnosis | Figure number |
|---|---|---|---|
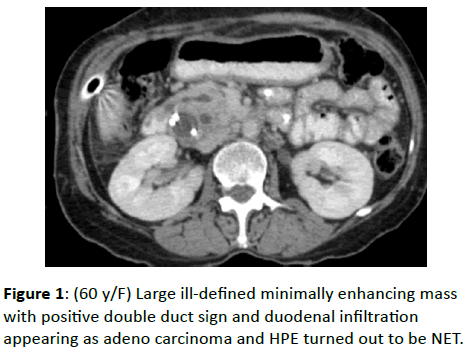
| Case 11 | Adeno ca | NET | Figure 1 |
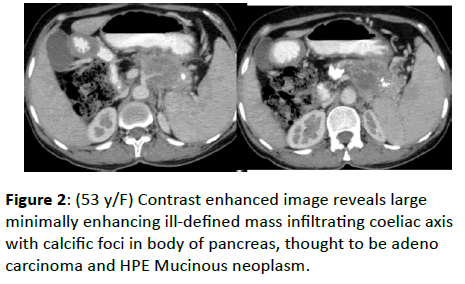
| Case 13 | Adeno ca | Mucinous neoplasm | Figure 2 |
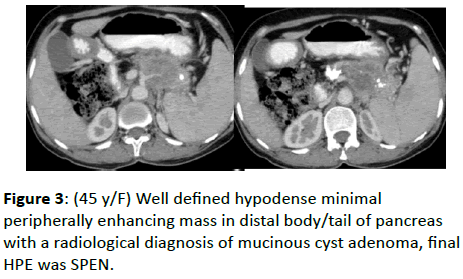
| Case 22 | Mucinous cyst adenoma | SPEN | Figure 3 |
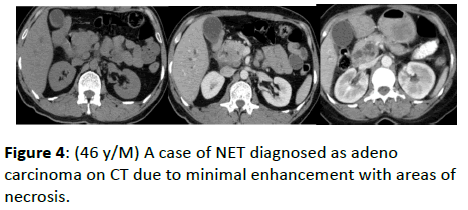
| Case 33 | Adeno ca | NET | Figure 4 |
| Case 34 | NET | GIST | Figure 5 |
Table 1: Cases are showing discrepancy in radiological and histopathological diagnosis.
Discussion
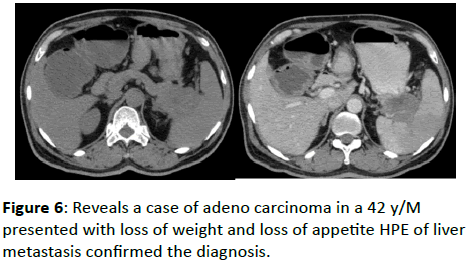
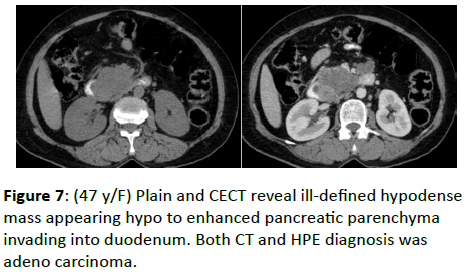
According to WHO 2010 classification, the pancreatic neoplasms are classified as epithelial tumors include benign, premalignant, malignant lesions, NET include non-functioning and functioning, syndromic and non-syndromic neoplasms and miscellaneous neoplasm. Ductal adenocarcinomas account for 90% of all pancreatic neoplasms. Most of patients are over 60 years of age and common in both male and female. They occur in pancreatic head in 62%, 26% in body, and 8% in tail . The tumors are highly invasive and often elicit desmoplastic reaction. Earliest imaging finding is pancreatic ductal dilatation and 60% may not have visible mass. Double duct sign is highly specific of pancreatic head malignancy. These tumors are hypodense on plain scan and appear iso/hypo to rest of enhancing parenchyma on CECT (Figures 6 and 7).
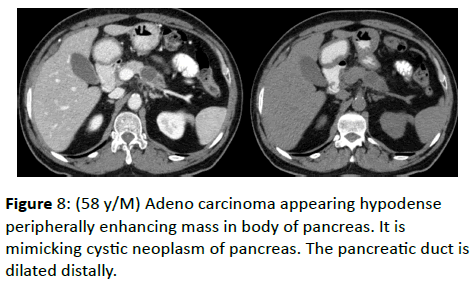
Rarely these tumors may be cystic/necrotic mimicking cystic neoplasm and rarely contain calcification (Figure 8) [5].
About 71% of our series are adenocarcinomas, predominantly situated in head (61%). All 24 cases of ductal adenocarcinomas had correct diagnosis on both CT and HPE. Three cases thought to be adenocarcinoma, but turned out to be NET (2) and mucinous neoplasm (1) (Figures 1, 2 and 4).
Kim SS identified that high grade NET, SPEN, Focal autoimmune pancreatitis and Groove pancreatitis are important mimics of ductal adenocarcinoma [6].
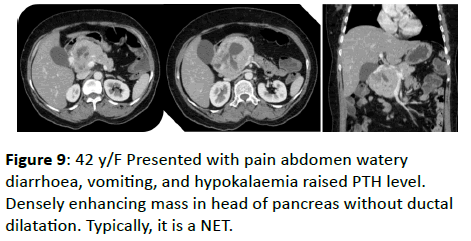
Neuroendocrine Tumors (NET)
NET accounts for 1-5% of pancreatic neoplasms and arise from endocrine part of pancreas [7]. Now it is thought that these tumors arise from pluripotent stem cells in ductal epithelium [2]. It occurs predominantly in male over 50 s. Mostly these tumors are sporadic but may be associated/part of MEN1, VHL, NF1. Non-functional tumors are large and present with mass effect whereas functional tumours are small (less than 3 cms), presenting with functional symptoms. In general, Islet tumors are hyper-enhancing. They may be within the gland or exophytic. Characteristically these lesions lack in desmoplastic reaction as in ductal adenocarcinoma and pancreatic ductal dilatation is rare (Figure 9) [7].
NET characteristically do not show calcification and larger lesion have areas of necrosis. Peripheral arterial phase enhancement is characteristic of these lesions. Out of 3, one had typical CT feature and HPE correlated well. Two cases of NET were misdiagnosed as adenocarcinoma on CT (Figures 1 and 4).
In one of those 2 misdiagnosed cases, due to IHBRD and ductal dilatation, the diagnosis of ductal adenocarcinoma was entertained. Kim et al stated that high grade NETs, small SPT, metastasis, groove pancreatitis may mimic pancreatic ductal adenocarcinoma [6]. Sometimes they may have dilatation of PD as in our case (Figure 1). Because of minimal enhancements, one of our cases was misdiagnosed as adenocarcinoma (Figure 4). But on retrospective analysis the absence of ductal dilatation should have prompted us for correct diagnosis. Absence of dilatation of PD, tumor thrombus and hyper vascularity of liver metastasis are clues to diagnosis of NET. There was a case that showed brilliant enhancement on CT with no ductal dilatation and spread. It was thought to be NET on CT, but it turned out as GIST on HPE, which was a surprise.
Cystic Pancreatic Neoplasms
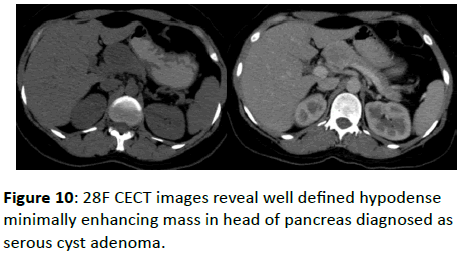
Serous cyst adenoma
Cystic pancreatic neoplasms are relatively uncommon accounting for only 1% of pancreatic tumors [8]. Serous cystadenoma is divided into micro/macrocytic tumors. These tumors occur in females of 7th decade. Hence it is known as grandmother tumor [8]. Despite predilection for females, it can occur in males. The classic appearance of microcystic adenoma is of large hypodense mass composed of conglomeration of small cysts, each one less than 2 cms (Figure 10).
Multiple thin densely enhancing septations due to high vascularity give an appearance of honeycomb pattern. The supplying vessels are frequently enlarged. Another important feature is central hyperdense scar with calcification [9]. Sometimes these tumors may be very large replacing entire parenchyma. The tumor markers are within normal limit. Macrocystic tumors are always benign and characterized by uni or multi locular cysts greater than 2 cms frequently occurring in females over 50 years of age. Sometimes, it is difficult to differentiate them from mucinous cystic neoplasms. Location in the pancreatic head, lobulated contour and lack of septal enhancement are specific for macrocystic serous cyst adenoma. The imaging findings and age of the patient were characteristic in both patients of our series. Hence, CT and HPE diagnosis were correlated in both of them.
Mucinous neoplasms
Mucinous cystic neoplasms are common cystic neoplasms occurring in middle aged women. Hence known as mother tumor and are potentially malignant. Most of them are asymptomatic but may present with nonspecific abdominal symptoms. Typically, they occur in body and tail of pancreas appearing as uni/multilocular cyst having round/lobulated contour. These lesions tend to be large with peripheral calcification in 16% of cases [10]. Multiple enhancing septation and solid mural nodules are typical radiologic findings of mucinous cystic neoplasm. Peripheral calcification is an important feature which differentiates from serus cyst adenoma which is seen at centre. Occasionally communication pancreatic duct and cystic neoplasm is present. There is a spectrum of mucinous cystic neoplasms from benign to malignant, but confident exclusion of malignancy is rarely possible on basis of imaging alone. Cyst fluid may have elevated CEA. Studies have shown that presence of calcification, thick wall>2 mm, septation correlated with 95% of risk of malignancy [11]. The only case of mucinous cyst adenoma had preoperative diagnosis of ductal adenocarcinoma (Figure 2) and another case had preoperative diagnosis of mucinous cyst adenoma was changed to SPEN on HPE (Figure 3).
A 53-year-old female patient had large minimally enhancing hypodense mass with calcific foci in body of pancreas infiltrating coeliac axis, thought to be adenocarcinoma and HPE Mucinous neoplasm. Because of well-defined minimally enhancing mass with small mural nodule in tail of pancreas in a 45 female patient we made the diagnosis of mucinous neoplasm; but it turned out to be SPEN. Age, site and large cystic appearance favoured mucinous neoplasm (Figure 3). In a study by Jonson et al, 47% of serous lesions and 50% of mucinous cystadenocarcinoma were judged atypical on basis of CT findings [12]. More recently a case series from same institute described 10 of 18 primary cystic neoplasms as atypical based on imaging features [13].
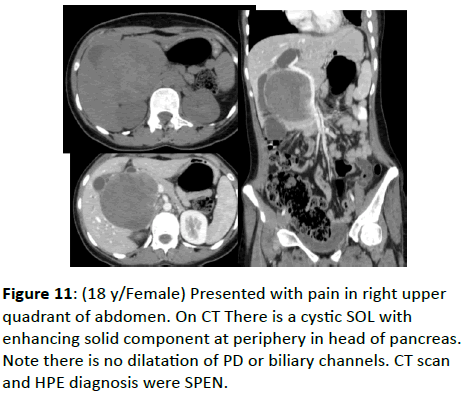
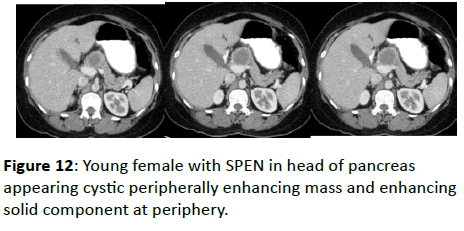
Solid pseudopapillary tumor
These are uncommon neoplasms with low malignancy potentially occurring predominantly in young females second decade (daughter tumor). Calcifications, cystic changes, internal hemorrhage due to weak vessels are characteristic [14]. They appear as a large mixed solid cystic lesion that occurs most commonly in head or tail of pancreas. They tend to be well encapsulated and contain hemorrhage and more solid enhancing component at periphery. The capsule also enhances with contrast. Fluid-fluid level and peripheral calcifications also seen. Biliary or PD dilatation is uncommon. The lesions are of low malignant potential. Even if metastasis or vascular invasions are seen in SPEN, surgery is curative. Hence early recognition is essential.
Two cases of SPEN had typical features and third case was diagnosed as Mucinous neoplasm due to large cyst with small mural nodule and HPE revealed SPEN (Figures 3, 11 and 12).
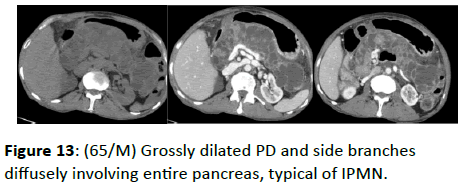
Intraductal Papillary Mucinous Neoplasm (IPMN)
These are tumours of low-grade malignancy, commonly occurring in elderly male. Hence it is known as grandfather tumors. They have predilection for ductal epithelium and may be predominantly cystic or papillary in composition. There is excess mucin production and dilatation of pancreatic duct or cystic dilatation of side branch. Presence of multifocal cysts supports the diagnosis and the demonstration of communications between cystic lesion and pancreatic duct is diagnostic of IPMN. There may be atrophy of parenchyma and can be classified as main duct type, segmental, branch duct type and diffuse variety [15]. In our study there was a single case of IPMN which was typical on CT (Figure 13).
ERCP typically demonstrates mucin secretion from bulging papilla with a dilated MPD. In a study by Kim KW et al, CBD dilatation, MPD dilatation, solid component and pancreatic atrophy were predictors of malignancy [16].
Gastrointestinal Stromal Tumor (GIST)
GIST can occur in GIT from oesophagus to anus. Sometimes omentum, mesentery or retroperitoneum are also involved. Rarely prostate and gall bladder are involved. GIST in pancreas is extremely rare. Only 7 cases are reported in the literature [17].
According to literature tumors are reported in females of 38-70 years. There is great variation in size from 2-20 cms; most occurring in the head of pancreas. EGIST can present as haemorrhagic pancreatic cysts. Typically show a large highly enhancing mass often heterogenous due to necrosis, haemorrhage or cystic degeneration. Our only case of pancreatic GIST was diagnosed on HPE and imaging diagnosis was NET due to intense homogenous enhancement (Figure 5).
Conclusion
Pancreatic ductal adenocarcinoma is the most common malignancy followed by NET and cystic neoplasms. Though extremely rare, GIST can also occur. CT has diagnostic accuracy of 85%. Since feasibility for resection and prognosis are different for each type of the tumors, definite early diagnosis is essential.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) Global Cancer Statisticset, GLOBOCAN estimates of incidence and mortality worldwide foe 36 cancers in 185 countries . CA Cancer J Clin 68: 394-424.
- Lewis RB, Lattin GE, Paal E (2010) Pancreatic endocrine tumours: Radiologic-clinicopathologic correlation. Radiographics 30: 1445-64.
- Treadwell JR, Zafar HM, Mitchell MD, Tipton K, Teitelbaum U, et al. (2016) Imaging tests for the diagnosis and staging of Pancreatic Adenocarcinoma: A meta-analysis. Pancreas 45: 789-795.
- Freeny PC, Marks WM, Ryan JA, Traverso LW (1988) Pancreatic ductal adenocarcinoma: Diagnosis and staging with dynamic CT. Radiol 166: 125-33.
- Callery MP, Chang KJ, Fishman EK, Talamonti MS, William Traverso L, et al.(2009) Pre-treatment assessment of resectable and borderline resectable pancreatic cancer: Expert Consensus statement. Ann Surg Oncol 16: 1727-1733.
- Kim SS, Choi GC, Jou SS (2018) Pancreas ductal adenocarcinoma and its mimics: Review of cross-sectional imaging findings for differential diagnosis. J Belg Soc Radiol 102: 71.
- Lee DS, Jeffrey RB, Kamaya A (2009) Islet cell tumors of pancreas: Spectrum of MDCT findings: A pictorial essay. Appl Radiol 38: 10-28.
- Friedman AC, Lichtenstein JE, Dachman AH (1983) Cystic neoplasm of pancreas. Radiol 149: 45-50.
- Procacci C, Graziani R, Bicego E (1997) Serous cystadenoma of pancreas report of 30 cases with emphasis on imaging findings. J Comput Assist Tomogr 21: 373-382.
- De Lima JE, Javitt MC, Mathur SC (1999) Mucinous cystic neoplasm of pancreas. Radiographics 19: 807-811.
- Procacci C, Bisauitti C, Carbognin G (1999) Characterisation of cystic neoplasms of pancreas: CT accuracy. J Comput Assist Tomogr 23: 906-12.
- Johnson CD, Stephens DH, Charboneau JW, Carpenter HA, Welch TJ, et al. (1988) Cystic pancreatic tumors: CT and sonographic assessment. AJR 151: 1133-1138.
- Carlson SK, Jonson CD, Brandt KR, Batts KP, Salomao DR, et al. (1998) Pancreatic cystic neoplasms: The role and sensitivity of needle aspiration and biopsy. Abdom Imaging 23: 387-393.
- Choi JY, Kim MJ, Kim SH (2006) Solid pseudo-papillary tumor of Pancreas: Typical and atypical manifestations. Am J Roent 187: W178-186.
- Lim JH, Lee G, Oh YL (2001) Radiologic spectrum of intraductal papillary mucinous tumor of pancreas. Radiographics 21: 323-340.
- Kim KW, Park SH, Pyo J, Yoon SH, Byun JH, et al. (2014) Imaging features to distinguish malignant and benign branch duct type intraductal papillary mucinous neoplasm of pancreas: A meta-analysis: Ann 259: 72-81.
- Reith JD, Goldblum GR, Lyles RH, Weiss SW (2000) Extraintestinal (soft tissue) stromal tumors. An analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol 13: 577-585.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences