Perineal Rectosigmoidectomy (Altemeier's Procedure) As a Surgical Treatment of Rectal Prolapse in Elderly People: Case Report and Review of the Literature
Mendoza Moreno F1*, Minaya Bravo A2, Diez Gago MR3, Minguez Garcia J1, Enjuto Martínez DT1, Tallon Iglesias B1, Solana Maono M1 and Arguello de Andres JM1
1Department of General and Digestive Surgery, Sanitas La Moraleja Teaching Hospital, Madrid, Spain
2Department of General and Digestive Surgery, Príncipe de Asturias Teaching Hospital, Madrid, Spain
3Emergency Department, Príncipe de Asturias Teaching Hospital, Madrid, Spain
- *Corresponding Author:
- Fernando Mendoza Moreno
Department of General and Digestive Surgery
Sanitas La Moraleja Teaching Hospital, Madrid, Spain
Tel: +0034917679100
E-mail: khoril@hotmail.com
Received Date: April 02, 2018; Accepted Date: April 07, 2018; Published Date: April 15, 2018
Citation: Moreno FM, Bravo MA, Gago MR D, Garcia JM, Martínez DTE, et al. (2018) Perineal Rectosigmoidectomy (Altemeier's Procedure) As a Surgical Treatment of Rectal Prolapse in Elderly People: Case Report and Review of the Literature. Gen Surg Rep. Vol.2 No.1:5
Abstract
Rectal prolapse is the complete protrusion of the rectum through the anus. It is more common in elderly women and among its symptoms can be observed bleeding, constipation, pain or incontinence. Its treatment is fundamentally surgical. We present the case of an 81-year-old patient with a history of constipation and incontinence secondary to a complete rectal prolapse. A rectosigmoidectomy was performed for perineal repair (Altemeier procedure). Repair of rectal prolapse can be done both, abdominal or perineal way. Traditionally, the perineal time has been reserved for elderly patients with greater comorbidities, presenting a higher rate of recurrence. Currently there is no consensus on the route of rectal prolapse approach, being the choice of the surgeon according to their preference and type of patient.
Keywords
Rectal prolapse; Altemeier proedure; Rectopexy; Rectosigmoidectomy; Levatorplasty
Introduction
Rectal prolapse is the complete protrusion of the rectum through the anal canal [1]. The first reference to this pathology is described in Ebers papyrus (1500 B.C.) [2]. Its etiology is diverse and different hypotheses have been formulated. Among the predisposing factors are anatomical factors (presence of a redundant sigma, laxity or loss of fixation of the rectum to the sacrum or herniation of the puch of Douglas) and extrinsic factors (pregnancy, chronic constipation, history of perineal trauma, etc.) [3]. It can occur less frequently in childhood due to congenital defects of connective tissue or sphincter muscles. Among the symptoms that originates we can find constipation, incontinence for gases or feces and sometimes it can cause bleeding or soaling [1]. We present the case of an 81-year-old woman with a medical history of rectal bleeding and fecal incontinence secondary to a rectal prolapse intervened by perineal rectosigmoidectomy (Altemeier's procedure).
Case Presentation
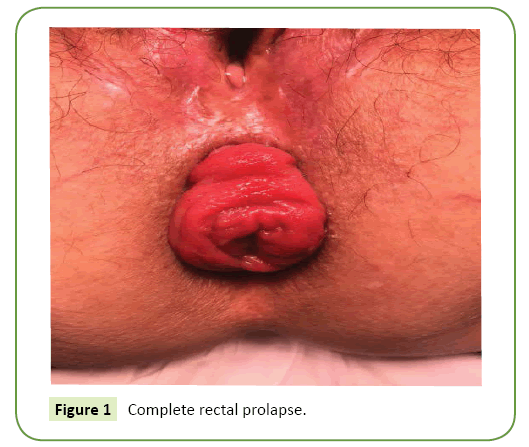
A 81-years-old female with previous medical history of hypertension, dyslipidemia and diabetes mellitus. She refered rectal pain with occasional bleeding that had intensified in recent months along with occasional incontinence. The clinical examination showed a complete rectal prolapse (Figure 1) becoming evident with Valsalva maneuvers (grade II of the Beahrs classification). The study was completed after performing a colonoscopy and a pelvic nuclear magnetic resonance that showed no alterations except a small component of cystocele associated with rectal prolapse. Given the age of the patient and the cardiovascular risk factors, the perineal approach was chosen for the repair of rectal prolapse according to the Altemeier technique (perineal rectosigmoidectomy). By general anesthesia and prophylaxis with amoxicillin was placed in gynecological position. They were administered before the surgery cleaning enemas.
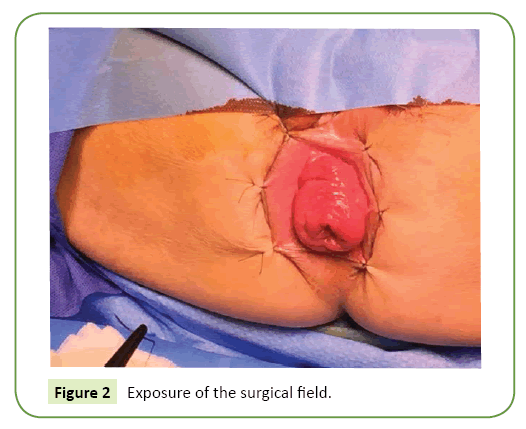
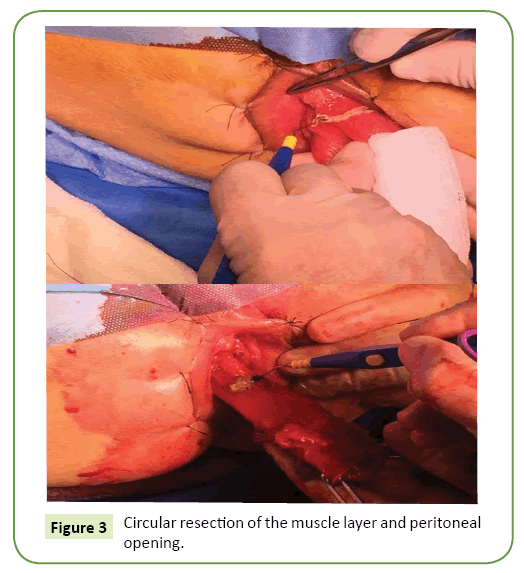
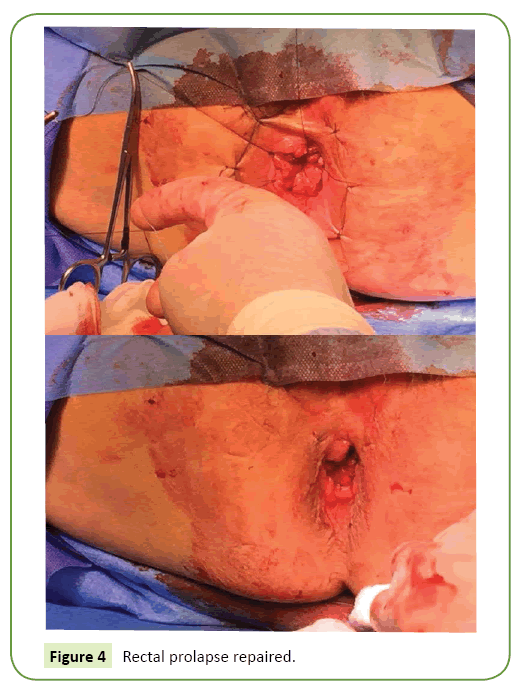
In a first time, in order to expose the surgical field properly, the anal margin to the perineum was sutured in a cardinal manner by loose 2/0 silk points (Figure 2). Subsequently, the prolapse was enucleated by electrical scalpel marking of the resection line approximately 1-2 cm above the pectineal line (Figure 3). Next, a circular resection was made to the muscular layer and the peritoneum of the Douglas pouch was open. Ligature of the sigmoid meso was performed and resection of the sigmoid colon by a sealing device (LigasureTM Small Jaw). It was not made a levatorplasty. Finally, a coloanal anastomosis was performed using 3/0 vicryl (novosyn polyglactin) (Figure 4).
At 24 hours after admission, the patient presented chest pain with elevated cardiac enzymes according with an acute coronary syndrome without elevation of the ST segment, so she was admitted to the Intensive Care Unit for cardiac catheterization. Coronary angiography showed a critical stenosis of the right coronary artery together with a severe stenosis (70%) of the anterior descending artery and a stenosis of 30% of the left main coronary artery, so angioplasty and coronary stent were performed in the right coronary artery. Despite antiplatelet medication, there were no significant episodes of rectal bleeding, sepsis or coloanal dehiscence. The patient was discharged after 7 days of admission. During follow-up, after 12 months, the patient presented improvement in bleeding symptoms and incontinence without recurrence signs.
Discussion
Perineal prolapse is a frequent pathology in postmenopausal and multiparous women [1]. It is 6 times more frequent in women than in men [3]. More than half of patients associate fecal incontinence and constipation [3,4]. It is a chronic disorder that increases the risk of pain and incontinence, and may be cause of incarceration or strangulation [2]. The surgical treatment of rectal prolapse is performed when medical treatment has failured. Its approach can be performed perineally or abdominally (laparoscopically or by open surgery). There is no clear consensus among the different authors and it seems that the choice of technique depends on the experience of the surgeon and the type of patient [5]. The first perineal rectosigmoidectomy was performed by Mikulicz in 1889 and later in 1933 by Miles but the procedure was abandoned due to its high recurrence rate (37%). However, it was not until 1971 that Altemeier and Cuberstson popularized the technique with a lower recurrence rate (10%) [6-9]. It presents a low mortality (0- 5%) and a recurrence between 0-16% [1]. To improve this, some authors have associated a levatorplasty, restoring the anorectal angle. Cirocco in her series does not describe recurrence after more than 3 years of follow-up [10]. Other techniques such as the one described by Delorme in 1900 for the treatment of rectal mucous prolapse have a similar mortality rate (0-4%) but with a higher recurrence rate (4-38%) [1]. Finally the anal encirclement described by Thiersch in 1891 has been abandoned for its high recurrence rate. However, nowadays, the perineal approach is the approach of choice for the treatment of incarcerated rectal prolapse and in young men, since there is no risk of erectile dysfunction because pelvic dissection is not performed.
With respect to the abdominal approach (laparoscopic or open surgery), rectopexy associated or not with sigmoidectomy is the most popular technique for the correction of rectal prolapse in young patients. It requires the mobilization of the rectum from the sacrum to the posterior anorectal junction and the fixation or not to a mesh. Sigmoidectomy seems to help in patients with a history of constipation who have a redundant sigmoid colon. It presents a recurrence rate between 0-95% with a morbidity between 0-20%. D'Hoore and Pennick described recopexy with mesh placement, being since then the preferred technique by surgeons especially in those with more experience in laparoscopic surgery [11]. However, the placement of a mesh can cause the rate of recurrence and morbidity to increase from 2% and 3% up to 10% and 52% respectively [3].
Perineal approach has a higher recurrence rate than the abdominal one, due to the impossibility to fix the rectum to the pelvis. La Greca have described a combined approach during the performance of rectosigramidectomy. In this way, the fixation of the rectal remnant can be performed laparoscopically, improving the tension and mobility of the rectal remnant [12]. However, authors such as Ricciardi or works such as the PROSPER study have found no significant differences between the different approaches, describing a similar rate of reinterventions and recurrences [13,14].
In our experience, from May 2015 to October 2017, 9 patients have undergone surgery for rectal prolapse in our center. A rectopexy was performed in 6 patients with polypropylene mesh placement (5 patients using a laparoscopic approach and 1 through open surgery due to previous surgeries), 2 perineal rectosigmoidectomies (Altemeier's procedure) and a Delorme's procedure. According to the literature, we chose the perineal approach in older patients (mean age of 80.3 years) and with higher comorbidities while rectopexy with mesh placement was performed in younger patients (mean age of 61.2 years) and lower surgical risk. No perineal fistula or local infection complications were described. After a follow-up of 18 months, no patient had signs of recurrence and in all the symptoms of pain, constipation and continence improved.
Conclusion
In conclusion, the repair of rectal prolapse is fundamentally surgical after the failure of medical treatment. The perineal approach generally has lower morbidity and a higher recurrence rate than the abdominal route and is usually performed in elderly patients with high surgical risk.
Conflict of Interest
The authors declare that they have no competing interests and any sources of funding for our publication.
References
- Goldstein SD, Maxwell PJ (2011) Rectalprolapse. Clin Colon Rectal Surg 24:39-45.
- Barfield LR (2017) Perinealapproches to rectal prolapse. Clin Colon Rectal Surg 30:12-15.
- Mik M, Trzcinski R, Kujawski R, Dziki L, Tchorzewski M, et al.(2015) Rectal prolapse in women-outcomes of perineal and abdominal approaches.Indian J Surg 77: 1121-1125.
- Ris F, Colin JF, Chilcott M, Remue C, Jamart J, et al. (2012) Altemeier's procedure for rectal prolapse: analysis of long-term outcome in 60 patients. Colorectal Dis 14: 1106-1111.
- Towliat SM, Mehrvarz S, Mohebbi HA, Sate Bigdeli A (2013) Outcomes of rectal prolapse using the altemeier procedure. Iran Red Crescent Med J 15:620-621.
- Mikulicz J (1889)For the treatment of prolapsus recti et cold invaginati. Arch Klin Chir 38: 74-97.
- Miles WE (1933)Rectosigmoidectomy as a method of treatment for procidentia recti. Proc R Soc Med 26: 1445-1448.
- Altemeier WA (1972)One-stage perineal surgery for complete rectal prolapse. HospPract7: 102-108.
- Altemeier WA, Culbertson WR, Schowengerdt C, Hunt J (1971) Nineteen years’ experience with the one-stage perineal repair of rectal prolapse. Ann Surg 173:993-1006.
- Cirocco WC (2010) The Altemeier procedure for rectal prolapse: an operation for all ages.Dis Colon Rectum 53:1618-1623.
- D’Hoore A, Penninckx F (2006) Laparoscopic ventral recto(colpo)pexy for rectal prolapse: Surgical technique and outcomefor 109 patients. Surg Endosc 20: 1919-1923.
- Greca GL, Sofia M, Primo S, Randazzo V, Lombardo R, et al. (2014) Laparoscopic implementation of the Altemeier procedure for recurrent rectal prolapse. Technical note. Int J Surg Case Rep. 5: 347-349.
- Ricciardi R, Roberts PL, Read TE, Hall JF, Marcello PW, et al. (2014) Which operative repair is associated with a higher likelihood of reoperation after rectal prolapserepair? Am Surg 80:1128-1131.
- Senapati A, Gray RG, Middleton LJ, Harding J, Hills RK, et al. (2013) PROSPER: A randomised comparison of surgical treatments for rectal prolapse. Colorectal Dis 15:858-868.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences