ISSN : 2574-2825
Journal of Nursing and Health Studies
Perceived Clinical Competency and Associated Factors of Basic Life Support (BLS) among Nurses Working in University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2020
Mengistu Abebe1*, Ambaye Dejen2, Bewuket Tadesse2 and Biks Liyew2
1Department of Nursing, Debre Markos University, Region, Ethiopia
2Department of Emergency and Critical Care Nursing, University of Gondar, Gondar, Ethiopia
- *Corresponding Author:
- Mengistu Abebe
Department of Nursing,
Debre Markos University,
Region, Ethiopia,
Tel: 251924531066;
E-mail: abebemengistu7@gmail.com
Received date: September 28, 2022, Manuscript No. IPJNHS-22-14640; Editor assigned date: October 03, 2022, PreQC No. IPJNHS-22-14640 (PQ); Reviewed date: October 18, 2022, QC No. IPJNHS-22-14640; Revised date: February 07, 2023, Manuscript No. IPJNHS-22-14640 (R); Published date: February 14, 2023, DOI: 10.36648/2574-2825.8.2.066
Citation: Abebe M, Dejen A, Tadesse B, Liyew B (2023) Perceived Clinical Competency and Associated Factors of Basic Life Support (BLS) among Nurses Working in University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2020. J Nurs Health Stud Vol:8 No:2
Abstract
Introduction: Competency in nursing is vital to safe patient care. Nurses are usually the first responders in cases of in hospital cardiac arrest. Their competence in Basic Life Support (BLS) is important in improving patient outcomes. Basic Life Support (BLS), a key component of the chain of survival decreases the arrest.
Objective: The study aimed to assess perceived clinical competency towards Basic Life Support (BLS) and associated factors among nurses working at university of Gondar comprehensive specialized hospital in Northwest Ethiopia.
Methods: An institutional based cross-sectional study was conducted from March-May, 2020 among nurses who are working in university of Gondar comprehensive specialized hospital. Systematic random sampling method was used to recruit study participant. A pretested structured selfadministered questionnaire was used for data collection. Data was entered using EPI info version 7.2.1 statistical software and analyzed using SPSS version 20 statistical package. Bivariate and multivariate logistic regressions were also carried out to see the effect of each independent variable on the dependent variable.
Results: More than half of the study participants were male 135 (57.7%), one hundred forty five (62.0%) participants were single. Three fourth of the study participants 172 (73.5%) perceived themselves as highly competent while 62 (26.5%) had low perception towards BLS. Among the 234 nurses, the majority of the study participants 177 (75.6%) had poor knowledge. Based on the multivariate regression to identify associated factors, three variables (clinical work experience, duration of working in the current area and average monthly income) were significantly associated with nurses’ perceived clinical competence towards BLS.
Conclusions: The overall perception of nurses towards BLS was high. Income, clinical work experience and duration of working in current area were factors significantly associated with perception of nurses towards BLS.
Keywords
Basic Life Support (BLS); Clinical Competency; Perception; Clinical work experience
Abbreviations:
AED: Automated External Defibrillator; ACLS: Advanced Cardiac Life Support; BLS: Basic Life Support; BSC: Bachelor of Science; CI: Confidence Interval; CPR: Cardio- Pulmonary Resuscitation; EC: Ethiopian Calendar; ED: Emergency Department; FBAO: Foreign Body Aspiration Obstruction; ICU: Intensive Care Unit; NICU: Neonatal Intensive Care Unit; OPD: Out Patient Department; PACU: Post Anesthesia Recovery Unit; PI: Principal Investigator; SCA: Sudden Cardiac Arrest; SPSS: Statistical Predictive System Software; US: United States; WHO: World Health Organization
Introduction
Clinical competency is critical for nurses to overcome today’s complicated heath care delivery system and to ensure patient safety [1]. Therefore, the dynamic and uncertain nature of healthcare environment requires competent professional nurse to manage the rapidly changing environment [2]. But practically there is shortage of competent experienced nurses globally; as a result, healthcare administrators face challenges to get competent and experienced nurses and are forced to find an option such as hiring newly graduated nurses to function independently and fill the shortage of competent and experienced nurses [3].
Based on healthcare providers’ level of professional education and experience; nursing competence is defined as the persons’ ability to perform nursing duties effectively to integrate cognitive, emotional and psychomotor skills during nursing cares [4].
Nurses are usually the first responders in cases of in hospital cardiac arrest. Their competence in BLS is important in improving patient outcomes. They need to be knowledgeable and skillful regarding BLS because it is a key component of the chain of survival that increases the rate of hospital discharge [5].
BLS refers to maintaining an airway and supporting breathing and circulation without using any equipment. Timely provision of BLS/CPR can save a precious life. BLS includes recognition of signs of Sudden Cardiac Arrest (SCA), heart attack, stroke and Foreign-Body Airway Obstruction (FBAO), as well as performing CPR and defibrillation with an Automated External Defibrillator (AED) [6].
Individuals in the community at least the health care professionals should know how to perform BLS as they encounter such situation very often. Health care professionals are expected to be competent towards BLS. In the United States, BLS training has been recommended for all health care professionals since 1966 especially for those who are involved in resuscitation. Demand for courses of BLS is ever increasing worldwide [7].
However, low confidence among medical students in performing BLS has been reported from Europe. Poor training among undergraduate medical students has also been reported from UK and Poland. Inadequate knowledge of BLS has been reported from Switzerland and Pakistan [8].
The practice of nursing requires good theoretical understanding of nursing knowledge and competence in technical skills, critical thinking, clinical decision making and assessment abilities. However, the definition of competency differs based on health care providers’ level of professional education and educational experience. Nurses in deferent settings and departments have different perception towards their clinical competence [9].
Perceived clinical competency is the reported ability to perform clinical practical skills. However, there is little or no information about how nurses in Ethiopia evaluate their clinical competence. This gap existed despite the evidence in the literature that determination of clinical competency is a central indicator of the quality of the curriculum [10].
However, studies revealed that the clinical competence of nurses in hospitals and other functioning areas is the concern and the center of attention for the managers, professional associations, government and society as a whole. In Ethiopia, lack of nurses’ clinical competence is one of the most important reasons for the change of educational curriculum from a three year program to a four year program [11].
Therefore, this study will be aimed to determine the levels of perceived clinical competency towards BLS reported by nurses and the factors associated with perceived clinical competency regarding BLS among nurses working at university of Gondar comprehensive specialized hospital.
Materials and Methods
Study design and period
An institutional based cross-sectional study design was conducted from March to May 2020 to determine perceived clinical competency towards BLS and associated factors among nurses working at university of Gondar comprehensive specialized hospital in different departments.
Study area
The study was conducted at university of Gondar comprehensive specialized hospital. The hospital is located in Gondar town, Amhara regional state Northwest Ethiopia. Gondar is 740 km from the capital city of Ethiopia, Addis Ababa. The town consisted one comprehensive specialized hospital and five health centers. The hospital was established in 1954 E.C and provides outpatient and inpatient services for more than 5 million peoples living in its catchment area as per three tier health care system of the national policy of Ethiopia. It has about 503 nurses who are working in different departments in the hospital. Among these 29 BSC nurses and one General Practitioner (GP) are working in emergency department. University of Gondar comprehensive specialized hospital ED was initiated in 2000 E.C and now it has more than 35 beds that render services for patients including patients with life threatening condition to average of 75 patients every day. This department also provides pharmacy and laboratory services for patients (unpublished data: University of Gondar comprehensive specialized hospital statistics bureau).
Source population
The source population of this study was all nurses working at university of Gondar comprehensive specialized hospital during the study period.
Study population
The study population of this study was nurses who were on duty in different departments of university of Gondar comprehensive specialized hospital during sample collection period and were participated in our study.
Inclusion and exclusion criteria
Inclusion criteria: All nurses working at university of Gondar comprehensive specialized hospital during the data collection period were included based on their willingness and eligibility to participate in the study.
Exclusion criteria: Those nurses on annual leave, training, seriously ill and nurses who were on managerial position during data collection were excluded from the study.
Sample size estimation
The sample size was determined by using single population proportion formula with the assumption of 50 % proportion, 95 % confidence level and 5 % margin of error. Given that the source population or nurses working in University of Gondar comprehensive specialized hospital is 503 which is less than 10,000 and 10% non-response was added. Based on this, the actual sample size for study was computed by using the following formula.
Where,
n=sample size of population greater than 10,000, Z=critical value of 95% CI=1.96, P=Proportion of clinical competency among nurses (50%)=0.5 because there is no similar previous study in the country, D=precision (marginal error)=0.05.
Then
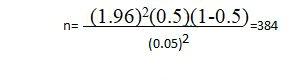
Since the source population or total number of nurses working in the hospital was 503, which was less than 10,000, we used the correction formula to calculate the final sample size.
nf=n/n/N+1
= 384/384/503+1=218
Where,
nf=final sample size, N=source populations
Thus, by adding 10% for possible non-response rate the total sample size was 240.
Sampling techniques
Systematic random sampling technique was used to select the study participants. Where N (the total number of nurses working at university of Gondar comprehensive specialized hospital) and n (minimum required sample size), then K=N/n; 503/240=2.1. So the study participants were recruited by every kth interval till getting the minimum required sample size. The first person was selected by lottery method and then the subjects getting in every second interval were recruited till getting 240 nurses. In case the second individual refrained or not eligible, the next individual was taken.
Data collection techniques and procedures
Data was collected using a structured and pretested selfadministered questionnaire. The questionnaire and the consent form were prepared in English. Participants were asked questions on perceived clinical competency towards BLS. Five principal investigators were collected the data during day and night with close supervision. Data quality was controlled by giving trainings and appropriate supervisions for data collectors. The overall data collection was carried out by the principal investigators. A pre-test was conducted using 5% of the questionnaire on nurses who were working in Bahir Dar referral Hospital. Appropriate modifications were made after analyzing the pretest result before the actual data collection.
Data analysis
The questionnaires filled by the nurses were checked for completeness and entered into EPI info version 7.2.1 statistical software and then exported to SPSS version 20 for further analysis. Descriptive and analytical statistics were used to describe the study population in relation to relevant variables. Both bivariate and multivariate logistic regression models were used to identify associated factors. Odds Rrtios and their 95%confidence intervals were computed and a variable with p-value less than 0.05 was considered as significantly associated with the outcome variable.
Data quality control
Data collectors were trained for 1 day before the study to ensure consistency and to reduce variations between data collectors. Daily communication was made by the principal investigators throughout the data collection. Collected data was checked for completeness and errors were corrected. Written documentation of responses from study participants was done after obtaining written consent to ensure that all feedback was captured for analysis. Data was managed using manually prepared dummy table tally based on the response of the respondents.
Variables
Dependent variable: Perceived clinical competency.
Independent variable: The independent variables of the study
were:
Socio-demographic characteristics
• Age
• Gender
• Marital status
• Religion
• Income
Educational and related factors
• Type of educational preparation (Diploma, Degree, Master).
• Theoretical knowledge of BLS.
• Attitude.
Experience related factors
• Working experience.
• Recent training on BLS.
• Certification on BLS.
• Attendance in case review session.
• Prior experience in BLS.
Environmental (working area) factors
• Working area.
• Duration of clinical experience in current working area.
Operational definitions
High perception: Nurses, who scored mean and above the mean score (≥ from 12) of perception related questions regarding BLS, were considered as having high perception of clinical competency towards basic life support.
Perceived clinical competence: In this study, nurses selfreported score of mean and above the mean score of perceived clinical competency related questions were considered as clinically competent; whereas those nurses who scored below the mean score of perceived clinical competency related questions were considered as clinically incompetent.
Results
Among 240 questionnaires which were distributed to the participants, 234 questionnaires were returned with a response rate of 97.5%.
Socio demographic characteristics of study participants
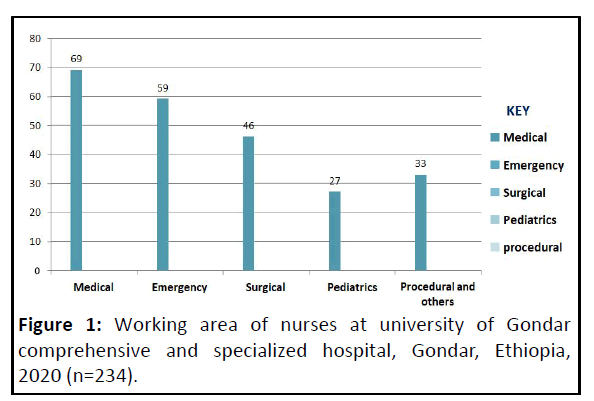
More than half of the study participants were male 135 (57.7%). The mean (± standard deviation) ages of the participants were 27.92 (± 5.072) years. One hundred and fortyfive (62.0%) participants and 87 (37.2%) were single and married in marital status respectively (Figure 1). The majority of the study participants 217 (92.7%) were orthodox by religion. From the total of 234 study participants the average monthly income was 5080.58 Ethiopian birr (Table 1).
| Variables | Category | Frequency N=234 |
Percent |
|---|---|---|---|
| Gender | Male | 135 | 57.7 |
| Female | 99 | 42.3 | |
| Age | 18-25 | 61 | 26.1 |
| 26-33 | 153 | 65.4 | |
| 34-41 | 15 | 6.4 | |
| >/=42 | 5 | 2.1 | |
| Marital status | Married | 87 | 37.1 |
| Divorced | 2 | 0.9 | |
| Single | 145 | 62 | |
| Religion | Orthodox | 217 | 92.7 |
| Muslim | 15 | 6.4 | |
| Protestant | 2 | 0.9 | |
| Monthly income | 2500-3499 | 6 | 2.6 |
| 3500-4499 | 58 | 24.8 | |
| 4500-5499 | 100 | 42.7 | |
| 5500-6499 | 55 | 23.5 | |
| >/=6500 | 15 | 6.4 |
Table 1: Socio-demographic characteristics of the respondents at University of Gondar comprehensive and specialized hospital, Gondar, Ethiopia, 2020.
Experience and related characteristics of the study participants
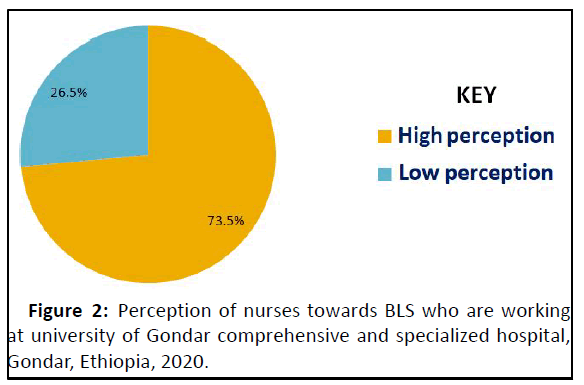
More than half of 142 (60.7%) the study participants had a total work experience of 2-5 years. The duration of clinical work experience was divided into 0 to 1 year, 2-5 years, 6-10 years and >10 years which comprised of 39 (16.7%), 142 (60.7%), 38 (16.2%) and 15 (6.4%) of the participants respectively. Nurses from medical departments comprised 69 (29.5%) and 59 (25.2%), 46 (19.7%), 27 (11.5%) of the participants were from emergency, surgical and pediatrics areas respectively (Figure 2). Regarding training and certification of the respondents on BLS, the majority of the participants 198 (84.6%) didn’t participate in BLS training, 124 (53.0%) attended case review session and 156 (66.7%) participated in the care of patients who needs BLS.
Perception of study participants towards BLS
The overall scores of nurses perceived clinical competency towards BLS ranges from 0 (lowest self-perceived competency) to 12 (highest self-perceived competency) with the mean score of 9.39+/-3.69. Three fourth of the study participants 172 (73.5%) perceived themselves as highly competent while 62 (26.5%) had low perception towards BLS (Table 2).
| No | Perception | Response | Number | Percent |
|---|---|---|---|---|
| 1 | Understand the role of nursing regarding BLS | Yes | 204 | 87.20% |
| No | 30 | 12.80% | ||
| 2 | Have necessary knowledge of BLS as a nurse | Yes | 192 | 82.10% |
| No | 42 | 17.90% | ||
| 3 | Have nursing skill regarding BLS | Yes | 179 | 76.50% |
| No | 55 | 23.50% | ||
| 4 | Can document client care effectively | Yes | 188 | 80.30% |
| No | 46 | 19.70% | ||
| 5 | Can communicate effectively | Yes | 200 | 85.50% |
| No | 34 | 14.50% | ||
| 6 | Knowledgeable on legal and ethical issues | Yes | 165 | 69.50% |
| No | 69 | 29.50% | ||
| 7 | Recognize signs and symptoms of patient deterioration | Yes | 204 | 87.20% |
| No | 30 | 12.80% | ||
| 8 | Can prioritize actions | Yes | 216 | 92.30% |
| No | 18 | 7.70% | ||
| 9 | Can take actions based on patient condition | Yes | 201 | 85.90% |
| No | 33 | 14.10% | ||
| 10 | Understand the rational for action and orders | Yes | 192 | 82.10% |
| No | 42 | 17.90% | ||
| 11 | Can evaluate patients response | Yes | 214 | 91.50% |
| No | 20 | 8.50% | ||
| 12 | Have succeed as a nurse regarding BLS | Yes | 197 | 84.20% |
| No | 37 | 15.80% |
Table 2: Perception of nurses working at Gondar University comprehensive and specialized hospital, Gondar, Ethiopia, June 2020.
Educational and knowledge status of the study participants
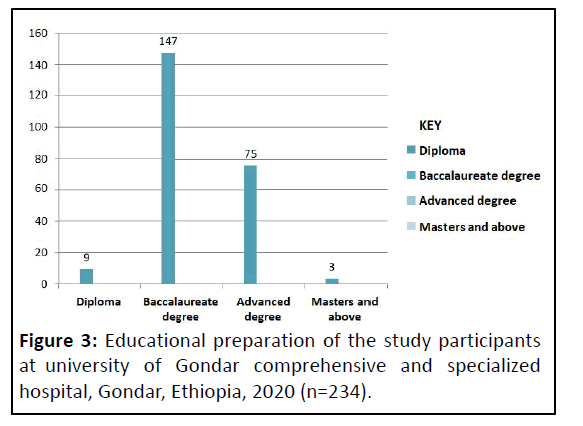
Out of 234 participants, 147 (62.8%) had a baccalaureate degree followed by 75 (32.1%) who had advanced degree in educational preparation (Figure 3). The knowledge scores of nurses were marked as low and high. Among the 234 nurses, the majority of the study participants 177 (75.6%) had poor knowledge while others 57 (24.4%) had high knowledge about BLS. The percentage of correct answer varied from 16.7% to 84.6%. The mean score for the participants was 3.69+/-1.57 (Table 3).
| No | Aspects to assess the knowledge of nurses | Knowledge level (% of nurses with correct answer | Self-perception | |
|---|---|---|---|---|
| High | Low | |||
| 1 | Abbreviation of BLS | 198 (84.6%) | 149 | 49 |
| 2 | What is the first response for unresponsive Patient found in the middle of the road? | 59 (25.2%) | 50 | 9 |
| 3 | After confirming somebody is unresponsive, what is your immediate action? | 17 | 6 | |
| 4 | Location of chest compression | 118 (50.5%) | 86 | 32 |
| 5 | Depth of compression in adults | 139 (59.4%) | 100 | 39 |
| 6 | Depth of compression in children | 39 (16.7%) | 27 | 12 |
| 7 | Depth of compression in neonates | 56 (24%) | 42 | 14 |
| 8 | Rate of chest compression in adult | 97 (41.5%) | 66 | 31 |
| 9 | Abbreviation of AED | 67 (28.6%) | 47 | 20 |
| 10 | What is your first response for responsive pt with choking? | 79 (33.4%) | 60 | 19 |
Table 3: Number and percentage of knowledge score of nurses working at Gondar University comprehensive and specialized hospital, Gondar, Ethiopia, June 2020.
Factors associated with perceived clinical competency of nurses towards BLS
To identify the effect of each independent variable on nurses’ perceived clinical competence of bivariate and multivariate logistic regression analysis was done.
In bivariate and multivariate logistic regressions income, work experience and duration of working in current area had significant association with nurses’ perceived clinical competency (Table 4).
| No | Variables | Category | Perception | COR (95%)CI | AOR (95%) CI | P-value | |
|---|---|---|---|---|---|---|---|
| High | Low | ||||||
| 1 | Age | 18-25 | 2 | 19 | 1 | ||
| 26-33 | 118 | 35 | 0.656 (0.339-1.269) | 0.812 | |||
| 34-41 | 10 | 5 | 1.105 (0.332-3.679) | 0.816 | |||
| >=42 | 2 | 3 | 3.316 (0.511-21.502) | 0.622 | |||
| 2 | Gender | Male | 102 | 33 | 0.781 (0.435-1.401) | 0.224 | |
| Female | 70 | 29 | 1 | ||||
| 3 | Marital status | Married | 69 | 20 | 0.711 (0.385-1.313) | 0.999 | |
| Single | 103 | 42 | 1 | 0.2 | |||
| 4 | Religion | Orthodox | 159 | 58 | 1.186 (0.385-1.313) | 1 | |
| Muslim | 13 | 4 | 1 | 0.999 | |||
| 5 | Income | 2500-3499 | 5 | 1 | 1 | 1 | |
| 3500-4499 | 39 | 19 | 2.436 (0.266-22.389) | 9.887 (0.594-18.560) | 0.11 | ||
| 4500-5499 | 83 | 17 | 1.024 (0.112-9.331) | 3.240 (0.702-14.953) | 0.132 | ||
| 5500-6499 | 37 | 18 | 2.432 (0.264-22.389) | 5.138 (1.237-21.345) | .024* | ||
| >=6500 | 8 | 7 | 4.37 (0.407-47.017) | 1.794 (0.445-7.240) | 0.412 | ||
| 6 | Educational preparation | Diploma | 5 | 4 | 1 | ||
| Baccalaureate | 104 | 43 | 0.517 (0.132-2.018) | 0.382 | |||
| Advanced | 61 | 14 | 0.287 (0.68-1.208) | 0.103 | |||
| Master and above | 2 | 1 | 0.625 (0.40-9.650) | 0.199 | |||
| 7 | Work experience | 0 to1 year | 24 | 15 | 1 | ||
| 2 to 5 years | 110 | 32 | 0.547 (1.64-1.820) | 3.248 (0.659-16.013) | 0.148 | ||
| 6 to 10 years | 31 | 7 | 0.255 (0.086-0.756) | 5.789 (1.440-23.272) | .013* | ||
| Over 10 years | 7 | 8 | 0.198 (0.054-0.728) | 6.445 (1.354-30.668) | .019* | ||
| 8 | Working area | Medical | 53 | 16 | 1 | ||
| Surgical | 31 | 15 | 1.603 (0.679-3.684) | 0.718 | |||
Note: AOR=Adjusted Odds Ratio, COR=Crude Odds Ratio, *=P-value <0.05, which is significantly associated with nurses self-perception of clinical competence.
Table 4: Bivariate and multivariate analysis of factors associated with perceived clinical competency of nurses towards BLS, Gondar, Northwest Ethiopia, June 2020 (n=234).
Discussion
The result of this study showed that nurses in the study sample perceive themselves in performing basic life support is high as indicated by the most frequent score with the overall mean score of 9.3+/-5.73. The overall score of nurses’ perceived clinical competency towards BLS was 73.5% as high and 26.5% as low which indicates nurses in this study feel competent regarding BLS. This finding is in line with a cross-sectional study conducted among nurses in Australia that showed 78% of the respondents were perceived themselves as highly competent. But lower than a study from Karlstad university among new graduated nurses using the nurse competence scale tool which revealed that overall 83% of the newly graduated nurses reported their competence as good and 16% of them reported it as very good. The difference might be from different study setting, study population, educational preparation as well as study period.
A study from Zambia revealed that 60.7% of the study participants had low perceived clinical competence whereas, 39.3% perceived themselves as highly competent which is lower than the current study. Likewise, the present study is inconsistent with the study from Trivandrum university which revealed that their perception was generally poor. This difference might be due to different reasons. First, it might be due to difference in study population and study period. Second, this might be difference in socio-demographic characteristics of the study participants. Thirdly, it could be from difference in educational level of the study population.
A study conducted in Ethiopia among final year nursing students showed that more than half of the study participants were perceived themselves as incompetent. This finding is inconsistent with the present study due to the possible reason of difference in study population, work experience and exposure of the study participants.
The highest perception score was observed in the area of prioritizing actions based on the patient’s condition (92.3%) and the lowest was in the area of knowledge regarding legal and ethical issues concerning BLS.
The overall score on the aspect of taking action to manage patients changing condition indicates nurses self-perceived competence is high, although not as highly scored as that of prioritizing actions based on patient’s condition. This finding was in line with the study conducted at university of Rhode Island.
Scores for nurses self-perception towards BLS were higher for those who participated in BLS training than for those who didn’t participate. A study from Trivandrum university showed that no significant association between BLS training, age and knowledge with perceived clinical competence. Even though knowledge score of the respondents was above the mean, their perception towards BLS was poor.
This study revealed that the participants had inadequate knowledge on BLS i.e. 75.6% of nurses scored below the mean whereas 24.4% of the participants answered ≥ 5 of the 10 questions. This finding is inconsistent with the study conducted in Trivandrum university among cardiac nurses showed that the knowledge of BLS was above the mean score even if there was no significant association between knowledge and clinical competence. This difference might be due to training on specialty, educational curriculum and the study population difference.
With the aim of this study being to explore the nature and extent of the relationships of several potential factors to nurses self-perceived clinical competence towards BLS, only three variables were found to be significant.
Based on the multivariate regression to identify associated factors, clinical work experience, income and duration of working in current clinical area were significantly associated with perceived clinical competence of nurses towards BLS.
This study showed that those nurses who had a clinical work experience of 6-10 years were nearly six times (AOR=5.789 (1.440-23.272)) and who had over 10 years were six times (AOR=6.445 (1.354-30.66)) more likely to perceive themselves as competent compared to those who had a work experience of 0 to 1 year. This finding is inconsistent with the study conducted in Nigeria showed that there was high perception in nurses who had less than five years’ experience. Similarly, a study conducted among 26 nurses which revealed that those newly graduated nurses were perceived themselves more highly competent than those who had 5 years’ experience. This difference might be due to the difference in the sample size, study period and sociodemographic characteristics of the participants.
The odds of having high perception are twelve times (12.184 (1.006-17.596)) in nurses who had a work experience 4 to 5 years in the current area than those nurses who had a work experience of 0 to 1 year in the current area. This finding is not comparable with other studies which revealed that statistical significant relationship was not demonstrated between duration of current working area and nurses’ perception of their clinical competence towards BLS.
Another association found in this study is monthly income of the respondents. It showed that those participants whose income was 5500-6499 Ethiopian birr were five times (AOR=5.138 (1.237-21.345)) perceived themselves highly competent when compared to those who had an average monthly income of 2500-3499 Eth. Birr.
Although the current study did not reveal any significant association between knowledge and perceived clinical competence, a number of studies indicated the associations of the two variables.
A study from Rhode Island revealed that attending in case review session and recent training on BLS were predictive of the nurses’ perceived clinical competence towards BLS. This finding was inconsistent with our study. This could be due to the difference study population, study design as well as educational preparation and training of the study participants.
In the current study no association was seen between self-perceived clinical competences between training on BLS, theoretical knowledge and working area. This finding was inconsistent with the study from Korea which revealed that work experience and theoretical knowledge of BLS were factors significantly associated with nurses’ perceived clinical competence towards BLS.
Conclusion
Based on the findings of this study, we conclude that the overall score of nurses’ perception towards BLS was high. This study showed that monthly average income, clinical work experience and duration of working in the current area were factors significantly associated with perceived clinical competence of nurses. However, the study showed that there is no statistically significant association between knowledge, attitude, BLS training or working area and perceived clinical competence.
Ethics Approval and Consent to Participate
This study was approved by the ethical review board of school of nursing, college of medicine and health sciences with reference number of (SOM/589/03/2020). After the purpose and objective of the study had informed, written consent was obtained from each study participant. Data was kept anonymously in the distributed questionnaire in order to keep confidentiality. All methods were performed in accordance with the relevant guidelines and regulations.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgement
We would like to express our heartfelt gratitude to department of emergency and critical care nursing, school of nursing, college of medicine and health science, university of Gondar for giving this chance. Next, we are very grateful to nurses who are working at Uuniversity of Gondar comprehensive and specialized hospital for being willing to participate and consumed a non-negligible amount of their time to fill up and complete all our questions in the questionnaire.
References
- Cheng C-Y, Liou SR (2013) Perceptions of clinical competence among nurse pregraduates: Do different types of nursing programs make a difference? J Nurs Educ 3:139-147
[Crossref] [Googlescholar] [Indexed]
- White AH (2003) Clinical decision making among fourth-year nursing students: An interpretive study. J Nurs Educ 42:113-120
[Crossref] [Googlescholar] [Indexed]
- Sportsman S (2010) Editor competency education and validation in the United States: What should nurses know? Nurs Forum 45:140-149
[Crossref] [Googlescholar] [Indexed]
- Klein CJ, Fowles ER (2009) An investigation of nursing competence and the competency outcomes performance assessment curricular approach: Senior students' self-reported perceptions. J Prof Nurs 25:109-121
[Crossref] [Googlescholar] [Indexed]
- Xanthos T, Akrivopoulou A, Pantazopoulos I, Aroni F, Datsis A, et al. (2012) Evaluation of nurses’ theoretical knowledge in basic life support: A study in a district Greek hospital. Int Emerg Nurs 20:28-32
[Crossref] [Googlescholar] [Indexed]
- Kandray DP, Pieren JA, Benner RW (2007) Attitudes of Ohio dentists and dental hygienists on the use of automated external defibrillators. J Dent Educ 71:480-486
[Crossref] [Googlescholar] [Indexed]
- Chandrasekaran S, Kumar S, Bhat SA, Shabbir PM, Chandrasekaran V (2010) Awareness of basic life support among medical, dental, nursing students and doctors. Indian J Anaesth 54:121-126
[Crossref] [Googlescholar] [Indexed]
- Yenus AM, Habib M, Vandana R (2015) Knowledge, attitude and practice among junior doctors and students in tertiary hospital. Shillong, India 3:12-13
- Greenberger H, Reches H, Riba S (2005) Do new graduates of registered nursing programs in Israel perceives themselves as technically competent? J Contin Educ Nurs 36:133-140
[Crossref] [Googlescholar] [Indexed]
- Jose ZM, Deepika V, Melita S (2015) Perceived competence on evidence based nursing practice among final year nursing students of selected college of Udupi Taluk. Int J Sci Res 4:248-249
- Katowa-Mukwato P, Banda S (2016) Self-perceived versus objectively measured competence in performing clinical practical procedures by final year medical students. Int J Med Educ 7:122-129
[Crossref] [Googlescholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences