ISSN : 2574-2825
Journal of Nursing and Health Studies
Birth Preparedness among Pregnant Women Attending Antenatal Clinic in Lagos Island Hospitals, Lagos, Nigeria
Folami F*, Olowe A and Ajibola A
Department of Nursing, College of Medicine, University of Lagos, Nigeria
Corresponding Author:
Dr. FF Folami
Department of Nursing, College of Medicine
University of Lagos, Nigeria.
Tel: +16788988314
E-mail: flofolami@yahoo.com
Received: December 11, 2018; Accepted: January 03, 2019; Published: Janaury 07, 2019
Citation: Folami F, Olowe A, Ajibola A (2019) Birth Preparedness among Pregnant Women Attending Antenatal Clinic in Lagos Island Hospitals, Lagos, Nigeria. J Nurs Health Stud Vol.3 No.2:5
DOI: 10.36648/2574-2825.1000034
Abstract
Globally, maternal mortality has remained a public health concern especially in developing countries in which Nigeria is not spared. Birth preparedness is a strategy to promote the timely use of skilled maternal and neonatal care, especially during childbirth, based on the theory that preparing for childbirth reduces delays in obtaining this care. The objective of this study is to assess the awareness of obstetric danger signs and practice of birth preparedness among pregnant women. The study adopted a descriptive cross-sectional design to provide answers to the objectives of the study. Respondents were recruited using simple random sampling technique with a total of 270 pregnant women participating in the study. A structured interviewer -administered questionnaire was used to collect data for a period of three weeks. Almost half of the respondents were young adults, with 78.1% having a tertiary education. There was a significant relationship between their knowledge of obstetric danger signs and level of education as well as the parity (χ2=11.935, df=4, p=0.018); (χ2=35.962, df=3, p=0.001) respectively. Also, a significant relationship was seen between respondents’ birth preparedness and the level of education (χ2=27.201, df=3, p=0.001). The respondents had fair knowledge of the danger signs during pregnancy and likewise practice of birth preparedness was fair. However, proper health education and awareness programme about the danger signs of pregnancy as well as the importance of proper preparedness of birth is still needed to help reduce maternal mortality in the country.
Keywords
Birth preparedness; Birth plan; Antenatal care; Maternal mortality
Background of Study
Each year, more than half a million women die during pregnancy and childbirth making pregnancy-related complications among the greatest killers of women of reproductive age in developing countries [1]. Globally, maternal death has remained a public health concern especially in developing countries where 99% of these deaths occur [2]. The burden of maternal death is currently alarming; not less than 289,000 maternal deaths occurred globally in 2013 (World health organization (WHO, UNICEF, United Nations Population Fund UNFPA, 2014); Sub-Saharan Africa alone accounts for 62% (179,000 maternal deaths) of these globally estimated maternal deaths [3]. Nigeria is one of the main countries experiencing burden of unsafe motherhood with a high maternal mortality ratio which account for more than 10% of the global estimate of maternal mortality [4]. Nigeria Demographic and Health Survey (NDHS) report for Nigeria in 2013 shows that Nigeria has maternal mortality ratio of 545 deaths/100,000 live births estimated to be 13% of the global maternal deaths.
One of the key roles of antenatal care is to provide health education on danger signs of pregnancy, delivery, preparation of a birth plan and to encourage delivery under a skilled attendant [5]. Studies performed in different countries have shown that health education during antenatal care enhances the utilization of skilled health care and improves mothers’ knowledge about obstetric danger signs [6,7]. Improved knowledge of obstetric danger signs, birth preparedness practices, and readiness for emergency complications are among strategies aimed at both enhancing utilization of maternal health services and increasing access to skilled care during childbirth, particularly for women with obstetric complications [8].
Birth preparedness is a strategy to promote the timely use of skilled maternal and neonatal care, especially during childbirth, based on the theory that preparing for childbirth reduces delays in obtaining this care. A birth plan/emergency preparedness plan include identification of following elements: knowledge of danger signs, the desired place of birth, the preferred birth attendant, the location of the closest appropriate care facility, funds for birthrelated and emergency expenses, a birth companion, support in looking after the home and children while the woman is away, transport to a health facility for the birth, transport in the case of an obstetric emergency, and identification of compatible blood donors in case of emergency [9].
Statement of Problem
According to World Health Organization in 2009, maternal deaths are thought to occur in developing countries due to delay in deciding to seek appropriate care, delay in reaching an appropriate health facility, and delay in receiving adequate emergency care once at a facility. The common causes of maternal deaths are haemorrhage, postpartum infection, hypertensive disorders, obstructed labour and abortion complications [10].
Since awareness of obstetric danger signs and adequate preparation for the birth of a baby would promote timely intervention and reduce delay in obtaining care in case of an emergency or complication, this study therefore assessed the awareness of obstetric danger signs and practice of birth preparedness among pregnant women attending antenatal clinic in Lagos island maternity hospital, Lagos, Nigeria.
Objectives
The broad objective of this study is to assess the awareness of obstetric danger signs and practice of birth preparedness among pregnant women attending antenatal clinic in Lagos island maternity hospital, Lagos. The study will specifically assess the level of awareness of obstetric danger among pregnant women attending antenatal clinic at Lagos island maternity hospital and the practice of birth preparedness among women attending antenatal clinic.
Concept of birth preparedness
According to Hiluf and Fantahun [11], every pregnant woman faces the risk of sudden, unpredictable complications that could end in death or injury to herself or to her infant. Hence, it is necessary to employ strategies to overcome such problems as they arise. Lack of advance planning for use of a skilled birth attendant for normal births, and particularly inadequate preparation for rapid action in the event of obstetric complications, are well documented factors contributing to delay in receiving skilled obstetric care [11]. Birth preparedness is a comprehensive strategy to improve the use of skilled providers at birth and the key intervention to decrease maternal mortality [12]. Women should discuss and review their birth preparedness plan with a skilled attendant at every antenatal care (ANC) assessment and one month before the expected date of birth. A birth and emergency preparedness plan includes identification of the following elements:- the desired place of birth, the preferred birth attendant, the location of the closest appropriate care facility, funds for birthrelated and emergency expenses, a birth companion, support in looking after the home and children while the woman is away, transport to a health facility for the birth, transport in the case of an obstetric emergency and identification of compatible blood donors in case of emergency [9]. Mutiso et al. [13] mentioned that birth preparedness and complication readiness is a safe motherhood strategy whose objective is to promote the timely use of skilled maternal and neonatal care during childbirth or obstetric emergencies by reducing delays at the first, second and third levels. Stating Ekabua et al. [14], in a setting where there is prevailing illiteracy, lack of infrastructure, poor transport system, and the principle and practice of birth preparedness and complication readiness (BP/CR) in a third world where access to skilled care providers are unpredictable have the potential of reducing the existing high maternal and neonatal morbidity and mortality rates. Women and new-borns need timely access to skilled care during pregnancy, childbirth, and the post-partum/ new-born period. However, too often, their access to care is impeded by delays in deciding to seek care, delays in reaching care, and delays in receiving care.
Elements of birth preparedness
According to the Skilled Initiative (Family Care International, FCI, 2013), the key elements of birth preparedness comprise attending antenatal care at least four times during pregnancy; identify a skilled provider and making a plan for reaching the facility during labour, setting aside personal funds to cover the costs of travelling to and delivering with a skilled provider and any required supplies; recognizing signs of complications; knowing what community resources-emergency transport, funds, communications, to mention a few are available in case of emergencies; having a plan for emergencies; knowing what transport can be used to get to the hospital, setting aside funds; identifying person(s) to accompany to the hospital and/or to stay at home with family; and identifying a blood donor. Since there is a probability of life-threatening complications occurring during the early postpartum period, birth preparedness also includes planning to access postpartum care during the first week after delivery and at six weeks after delivery.
Factors influencing birth preparedness
A study in Adrigat, Ethiopia indicated that maternal education was a strong predictor in preparation for birth and complication. Literate mothers were about two times more likely to be prepared for birth and complication than illiterate women [11]. A cross sectional study on birth preparedness among slum women in Indore city (India) found that literacy, availability of ante-natal services, literate husband, better knowledge about maternal/ new born danger signs suggestive for seeking referral were associated with well preparedness [15].
Women carrying their first child were probably more susceptible to difficulties during labour and were more cautious than women who have had several births [16]. Before, women who were pregnant for the first time were more motivated to utilize maternity care because they did not know what to expect from the process [17]. Subsequently, as a woman endured more pregnancies, she would rely on her experience and draw from that knowledge [17].
Age was highly correlated with parity (number of pregnancies) and, in some settings, with educational level [18]. Babalola and Fatusi [19] found that in Nigeria, women in the middle child bearing ages were more likely to use maternal health services than women in early and late child bearing. Ethnicity and religion are often considered markers of cultural background and are thought to influence beliefs, norms, and values in relation to childbirth, service use, and women's status [18]. In a study conducted in Nigeria, it was determined that ethnicity seemed to make no significant difference in the use of antenatal care, however, it made a significant difference in the use of skilled assistance and post- natal care. In the same study, it was found that the level of service utilization was significantly higher among the Igbos (in the south) and the minority tribe compared to the Hausas (in the north). This result reflects the influence of the cultural and religious beliefs in the north. The Islamic religion may have had a strong influence on the cultural beliefs and traditions on child birth of the Hausas in the north [19]. Women who were working and earning money may have been able to save and decided to spend it on a facility delivery [18].
In addition to health factors like haemorrhage, non -health factors have been associated with poor maternal outcomes. They include poor health seeking behaviour, illiteracy, inadequate health education on obstetric emergencies and poverty. Sociocultural beliefs and practices that lead to gender inequity have also contributed in some societies. Poverty and low priority in health in developing countries have led to bad health indicators. Finally inadequate infrastructure and long travelling distance to health facilities increase the second and third delay [20].
Awareness of birth preparedness and practice
Birth Preparedness (BP) is the process of planning for normal birth and anticipating the actions needed in case of an emergency. Responsibility for BP must be shared among all safe motherhood stakeholders; policy makers, facility managers, providers, communities, families, and women because a coordinated effort is needed to reduce the delays that contribute to maternal and new born deaths [21]. John [22] in a cross sectional study carried out on awareness of birth preparedness and complication readiness in south-eastern Nigeria indicated that although awareness of the concept of birth preparedness was high (70.6%), knowledge of specific key danger signs was poor. A study in Ogbomoso (South-west, Nigeria) shows that only 40.3% of the respondents were reported well prepared for births and were complication ready. The proportion of women who had Birth preparedness and complication readiness was significantly higher among those in the middle socio-economic group (51.6%, p<0.05), Respondents in lower socio-economic group were 42% less likely to have prepared for birth compared to women in the high socio-economic class (OR: 0.58, 95% CI: 0.34-0.99) [23]. Also, according to a study carried out on birth preparedness among women in Tharakanithi county, Kenya [24], the proportion of women that was prepared for birth was low (20.3%). The aspect of birth preparedness that was identified and planned for by the highest number of women was finances for delivery expenses (74%) followed by place of delivery (68%) while the least was the mode of transport to the facility (35%).
The role of knowledge on pregnancy and childbirth in birth preparedness
Provision of a health worker with midwifery skills at every birth is considered a crucial intervention for safe motherhood, yet the WHO estimates that 47% of births in the developing world are assisted only by TBAs, family members, or no one [3]. This, together with poor communication between lay women and providers, sharply influences pregnant women’s perceptions of antenatal care services and helps to shape their service utilization, reinforcing views of antenatal care as a nuisance and of labour and delivery as requiring facility-based care [25]. While these approaches to antenatal care provision and utilization may help contribute to safer childbearing through facility-based delivery, they also serve to limit women’s understandings of health and health risks during pregnancy. Women’s limited understandings of health in pregnancy contribute to late antenatal health seeking and inadequate attendance partners, which contribute in turn to avoidable prenatal deaths. Findings from a previous study by Kabakyenga et al. [26] revealed that knowledge of obstetric danger signs and birth preparedness are strategies that enhance the utilization of skilled care during low-risk births and emergency obstetric care in complicated cases in low income countries. The presence of skilled attendants at births and availability of emergency obstetric care have been shown to greatly reduce maternal deaths that occur due to obstetric complications [25].
Obstetric danger signs
Women individually, their partners and the communities need to be educated on danger signs so that they can seek appropriate care from skilled providers in time. Studies in low-income countries showed knowledge of obstetric danger signs especially during pregnancy and delivery among women is deficient [10]. Studies further reported that prolonged labour as a danger sign was reported by the least number of women respondents [10,27]. Obstetric danger signs include persistent vomiting, severe persistent abdominal pain, vaginal bleeding during pregnancy and delivery, severe vaginal bleeding after delivery, swelling of face, fingers and feet, blurring of vision, fits of pregnancy, severe recurrent frontal headache, high grade fever, marked change in fetal movement, awareness of heart beats, high blood pressure, sudden escape of fluid from the vagina, dysuria, oliguria or anuria, prolonged labour, loss of consciousness and retained placenta [28]. Counseling on pregnancy danger signs is to be conducted according to focused antenatal care (FANC) guidelines, which include signs such as vaginal bleeding, severe headache or blurred vision, severe abdominal pain, swollen hands and face, fever, fetus movement reduced or absence and excessive tiredness /breathlessness [10]. Obstetric nurse/ midwife plays a crucial role in promoting an awareness of the public health issues for the pregnant woman and her family, as well as helping the pregnant woman to recognize complications of pregnancy and where to seek medical assistance [28]. Lack of awareness about obstetric danger signs was related younger age, low level of education, income, gravidity and parity, previous experiences with any obstetric complications, lack of antenatal care and decision making power [28].
Theoretical Review
Thaddeus and Maine three delays model
The Thaddeus and Maine [29] model have provided the safe motherhood community with an explanatory model of maternal mortality that identifies delays in seeking, reaching and obtaining care as the key factors leading to maternal death. According to the three-delay model, delays in seeking care, delays in reaching care and delays in receiving adequate care once at the point of service are key factors leading to maternal death, awareness of obstetric danger signs and practice of birth preparedness can prevent these three forms of delay, thereby improving maternal heath outcome. practice of birth preparedness ensures that there is a decision maker on ground and also since the family is aware of the obstetric danger, problem is easily recognized and this would prevent waste of time while trying to make a decision and would guide towards making a healthy decision, planning for transportation, saving money and locating an accessible and appropriate health centre and plan to reach an appropriate referral facility is part of birth preparedness and would go a long way in ensuring a smooth journey towards delivery of a baby and enable quick and appropriate response to problems or complications that may occur during the process of giving birth, thereby reducing maternal mortality in the long run.
Research Methods
Research design
A non-experimental approach was adopted which involves no intervention or manipulation of variables, therefore a descriptive quantitative research design was used since it describes the aspect of a situation that existed at a particular time, hence facilitating the objective of the study which is to assess the birth preparedness and complication readiness among pregnant women attending antenatal clinic in Lagos island maternity hospital, Lagos state.
Sampling technique
Simple random sampling technique was employed. In the absence of a sampling frame, the lottery method was the most appropriate sampling technique for this study. An average of 80 women report at the ANC per day based on the hospital statistics. Using this information, a lottery method was adopted where fifty (50) cards were marked, (forty (40)” yes” and ten (10) “no” these cards were placed in a sack and all the pregnant women in their second and third trimester visiting the ANC were asked to dip their hands into the sack and pick a card. Those who picked “yes” were interviewed after they gave their consent and their ANC cards were marked to avoid interviewing them twice.
Sample size estimation
The sample size was calculated using the formula:

For population greater than 10,000, Where,
n=sample size for a population greater than 10,000,
z=the normal standard deviation set at 1.96 which corresponds with 95% confidence interval,
p=the prevalence rate, which is the proportion of the pregnant women that the practice of birth preparedness was from the previous study, was (20.0%) [30].
q=1-p, 80%
e=degree of accuracy/precision usually set at 0.05,
n=1.962 × 0.20(0.80)/0.052,
n=3.8416 × 0.403 (0.597)/0.0025
n=245.8
n=246
To compensate for improperly completed questionnaires or opt out by any of the selected respondents; the formula is:
ns=10% of nf+nf
where, ns=minimum population for non-response.
n=10% (246)+246=270 participants.
Data collection instrument
A stuctured interviewer-administered questionnaire was used to collect data for a period of three weeks Data collection started on each day from the beginning of the clinic till when clinic ends. Only Participants that give informed consent were used. The questionnaire was developed using prototype created by the JHPIEGO-monitoring birth preparedness and complication readiness practice; tools and indication by Del Barco [31]. It was created for researchers to assess birth preparedness practice. Some more questions were adapted from previous studies [22,32]. The questionnaire was made of four (4) sections; A, B, C and D. Section A consists of questions on socio-demographic data, section B consists of questions on respondents clinical characteristics, section C consists of questions on awareness of obstetric danger signs while Section D consists of questions on practice of birth preparedness.
Validity and reliability of the instrument
The instrument was validated through a review by the supervisor and a panel of experts consisting of nursing professionals as well as experienced professional researchers. Their observations and comments were used to effect corrections before the instrument will be administered to the respondents. A pilot study was carried out on thirty seven (10% of total sample) respondents in another health institution to ensure that the instrument measure what it is supposed to measure. All ambiguous questions were either reframed or removed.
Method of Data Collection
Data was collected through face-face interviews with the pregnant women at the Lagos Island maternity hospital. Two nurses were recruited as data collectors, their knowledge on the topic were tested before recruitment. Purpose of the study and method of data collection was explained to the data collectors before beginning of data collection and to the participants as well. Consent was sought, assurance of confidentiality was made, and freedom to withdraw from participating was made known to the participants before the onset of data collection. This was done within three weeks.
Method of data analysis
The data obtained was analysed electronically using Epi-Info software (version 3.5.1) and Microsoft Excel 2007. Frequency, mean and tables were generated from relevant variables. Chisquared test will be used to calculate association between exposure and outcome.
Ethical consideration
Ethical approval for the study was obtained from the ethics and research committee of the Lagos University Teaching Hospital. Permission was sought from the chief medical director of Lagos Island maternity hospital. Informed consent was obtained from each of the participant with an assurance of confidentiality.
Presentation of Results
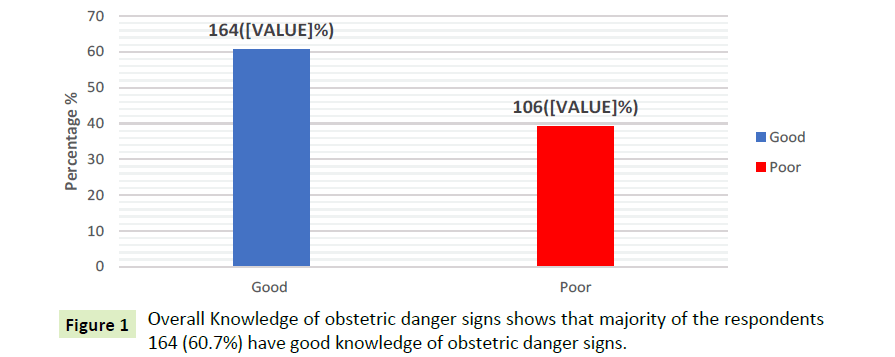
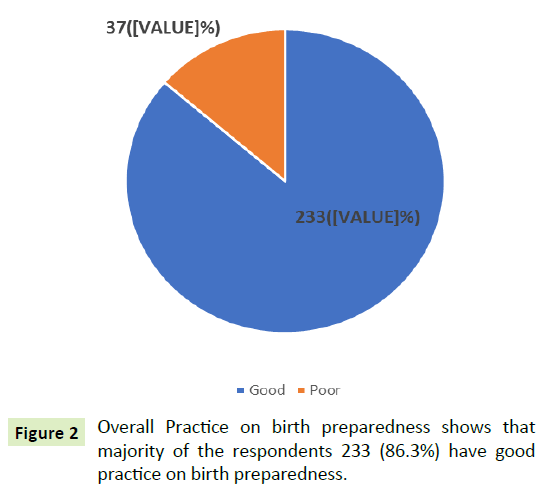
This presents the result of the study based on data analysis. The results are set out in a format aligned with the four sections of the questionnaires- socio demographic characteristics, clinical characteristics of respondents, knowledge of obstetric danger signs and practice of birth preparedness. A total of 270 questionnaires were distributed to assess the awareness of obstetric danger signs and practice of birth preparedness among pregnant women attending antenatal clinic in Lagos island maternity hospital, Lagos. All the questionnaires were returned and adequately filled giving a response rate of 100% (Tables 1-6; Figures 1 and 2).
| Variables Age (years) | Frequency (n=270) | Percentage (%) |
|---|---|---|
| Below 20 | 7 | 2.6 |
| 21-30 | 134 | 49.6 |
| 31-40 | 109 | 40.4 |
| Above 40 | 20 | 7.4 |
| Total | 270 | 100.0 |
| Marital status | ||
| Single | 5 | 1.9 |
| Married | 265 | 98.1 |
| Total | 270 | 100.0 |
| Educational Status | ||
| No formal education | 3 | 1.1 |
| Primary | 6 | 2.2 |
| Secondary | 50 | 18.5 |
| Tertiary | 211 | 78.1 |
| Total | 270 | 100.0 |
| Religion | ||
| Christianity | 163 | 60.4 |
| Islam | 103 | 38.1 |
| Others | 4 | 1.5 |
| Total | 270 | 100.0 |
| Source of income | ||
| Trade | 59 | 21.9 |
| Civil servant | 47 | 17.4 |
| Self-employed | 132 | 48.9 |
| Others | 32 | 11.9 |
| Total | 270 | 100.0 |
Table 1 Socio-Demographic Characteristics shows that majority of the respondents 134 (49.6%) were within the age range 21-30 followed by 40.4% of who were within the age range 31-40 years. Most of the respondents 265 (98.1%) were married and 211 (78.1%) of the respondents had tertiary education. More than half of the respondents 163 (60.4%) were practicing Christianity and 132 (48.9%) of the respondents were self-employed.
| Variables Gravidity | Frequency (n=270) | Percentage (%) |
|---|---|---|
| Once | 136 | 50.4 |
| Twice | 68 | 25.2 |
| 3 times | 29 | 10.7 |
| More than 3 times | 37 | 13.7 |
| Total | 270 | 100.0 |
| Parity | ||
| None | 142 | 52.6 |
| Once | 61 | 22.6 |
| 2 times | 50 | 18.5 |
| 3 times | 9 | 3.3 |
| More than 3 times | 8 | 3.0 |
| Total | 270 | 100.0 |
| Number of ANC Visit | ||
| Less than 4 | 116 | 43.0 |
| 4-8 | 93 | 34.4 |
| 9-12 | 30 | 11.1 |
| More than 12 | 31 | 11.5 |
| Total | 270 | 100.0 |
| Gestational age | ||
| Second trimester | 113 | 41.8 |
| Third trimester | 157 | 58.1 |
| Total | 270 | 100.0 |
| Type of Previous Delivery | ||
| None | 145 | 53.7 |
| Vaginal delivery | 93 | 34.4 |
| Caesarean section | 27 | 10.0 |
| Vaginal and caesarean section | 1.9 | 5 |
| Total | 270 | 100.0 |
| Place of Previous Delivery | ||
| Home | 13 | 4.8 |
| Governmental hospital | 91 | 33.7 |
| Private hospital | 26 | 9.6 |
| Primary health Centre | 9 | 3.3 |
| No response | 131 | 48.5 |
| Total | 270 | 100.0 |
| History of still birth and health problem during previous pregnancy | ||
| Yes | 26 | 9.6 |
| No | 176 | 65.2 |
| No response | 68 | 25.2 |
| Total | 270 | 100.0 |
Table 2 Clinical characteristics of the respondents half of the respondents 136 (50.4%) number of gravidity is one and only 37 (13.7%) had gravidity of more than 3 times. more than half of the respondents 142 (52.6%) are non-parous while 61 (22.6%) of the respondents parity is one.
| Variables | Frequency (n=270) | Percentage (%) |
|---|---|---|
| Do you have a knowledge of obstetric danger signs? | ||
| Yes | 136 | 50.4 |
| No | 134 | 49.6 |
| Total | 270 | 100.0 |
| Source of Information | ||
| Health personnel | 104 | 38.5 |
| Mass media | 22 | 8.1 |
| Others | 5 | 1.9 |
| Personnel and mass media | 14 | 5.2 |
| No response | 125 | 46.3 |
| Total | 270 | 100.0 |
| What are the danger signs during pregnancy that you know can endanger the life of a woman? | ||
| Fever | 32 | 11.9 |
| Bleeding | 38 | 14.1 |
| Severe headache | 8 | 3.0 |
| Swollen hands/face | 3 | 1.1 |
| Loss of consciousness | 2 | 0.7 |
| Convulsion | 3 | 1.1 |
| Water breaks without labour | 8 | 3.0 |
| Trouble with vision and swollen hand/face | 20 | 3 |
| Water breaks without labour | 10 | 3.7 |
| Fever, bleeding, convulsion and loss of consciousness |
43 | 15.9 |
| Reduced or accelerated foetal | 35 | 12.9 |
| Don’t know | 7 | 2.6 |
| No response | 5 | 1.9 |
| What the danger signs are during labour that you know can endanger the life of a woman | ||
| Placental not delivered 30 minutes after baby | 117 | 43.3 |
| Severe abdominal pain | 13 | 4.8 |
| Don’t know | 104 | 38.5 |
| Severe abdominal pain | 27 | 10.0 |
| Others | 8 | 3.0 |
| No response | 1 | 0.4 |
| Total | 270 | 100.0 |
| What are the danger signs after labour that you know can endanger the life of a woman | ||
| Severe bleeding | 72 | 26.7 |
| Loss of consciouness | 3 | 1.1 |
| Difficulty breathing | 6 | 2.2 |
| Severe weakness | 8 | 3.0 |
| Don’t know | 85 | 31.5 |
| Malodorous vaginal discharge | 11 | 4.1 |
| Difficulty breathing and severe weakness | 11.5 | 31 |
| Severe bleeding and loss of consciousness | 27 | 10.0 |
| No response | 3 | 1.1 |
| Others | 24 | 8.9 |
Table 3 knowledge of obstetric danger signs shows that 136 (50.4%) of the respondents reported that they have knowledge of obstetric danger signs, 104 (38.5%) of the respondents source of information was from health personnel. only 53 (19.6%) of the respondents reported that they don’t know the danger signs during pregnancy that can endanger the life of a woman. 38 (14.1%) of the respondents identified bleeding as a danger sign during pregnancy. placental not delivered 30 minutes after baby was identified by 117 (43.3%) as a danger sign during labour that they know can endanger the life of a woman while 104 (38.5%) said they don’t know.72 (26.7%) also identified severe bleeding as a danger sign after labour that could endanger the life of a woman.
| Variables | Frequency (n=270) | Percentage (%) |
|---|---|---|
| Do you know your expected date of delivery? | ||
| Yes | 209 | 77.4 |
| No | 61 | 22.6 |
| Total | 270 | 100.0 |
| Is it possible for labour to start before due date? | ||
| Yes | 240 | 88.9 |
| No | 30 | 11.2 |
| Total | 270 | 100.0 |
| Have you identified the facility you will give birth in? | ||
| Yes | 228 | 84.4 |
| No | 42 | 14.6 |
| Total | 270 | 100.0 |
| If yes, where | ||
| Private hospital | 39 | 14.4 |
| Government hospital | 204 | 75.6 |
| No response | 27 | 10.0 |
| Total | 270 | 100.0 |
| Have you identified the mode of transportation to hospital when labour begins? | ||
| Yes | 197 | 73.0 |
| No | 73 | 27.0 |
| Total | 270 | 100.0 |
| If yes what mode of transportation have you arranged for? | ||
| Private transport | 100 | 37.0 |
| Public transport | 79 | 29.3 |
| No response | 91 | 33.7 |
| Total | 270 | 100.0 |
| Are you aware that you may need blood during labour? | ||
| Yes | 224 | 83.0 |
| No | 46 | 17.0 |
| Total | 270 | 100.0 |
| Have you already arranged for a blood donor? | ||
| Yes | 185 | 68.5 |
| No | 85 | 31.5 |
| Total | 270 | 100.0 |
| Do you already have blood in the blood bank? | ||
| Yes | 192 | 71.1 |
| No | 78 | 28.9 |
| Total | 270 | 100.0 |
Table 4 Practice of birth preparedness shows that majority of the respondents 209 (77.4%) knew their expected date of delivery and most of them 240 (88.9%) reported that it is possible for labour to start before due date.
| Overall knowledge | Good (%) | Poor (%) | Total (%) | ?2 | df | p-value |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Below 20 | 4 (57.1) | 3 (42.9) | 7 (100.0) | 2.525 | 3 | 0.471 |
| 21-30 | 85 (63.4) | 49 (36.6) | 134 (100.0) | |||
| 31-40 | 66(60.6) | 43(39.4) | 109(100.0) | |||
| Above 40 | 9(45.0) | 11(55.0) | 20(100.0) | |||
| Marital status | ||||||
| Single | 5(100.0) | 0 | 5(100.0) | 3.293 | 1 | 0.070 |
| Married | 159(60.0) | 106(40.0) | 265(100.0) | |||
| Level of education | ||||||
| No formal education | 1(33.3) | 2(66.7) | 3(100.0) | 35.962 | 3 | <0.001 |
| Primary | 2(33.3) | 4(66.7) | 6(100.0) | |||
| Secondary | 13(26.0) | 37(74.0) | 50(100.0) | |||
| Tertiary | 148(70.1) | 63(29.9) | 211(100.0) | |||
| Parity | ||||||
| None | 84(59.2) | 58(40.8) | 142(100.0) | 11.935    4 | 0.018 | |
| Once | 34(55.7) | 27(44.3) | 61(100.0) | |||
| Twice | 29(58.0) | 21(42.0) | 50(100.0) | |||
| 3 times | 9(100.0) | 0 | 9(100.0) | |||
| More than 3 times | 8(100.0) | 0 | 8(100.0) | |||
Table 5 Relationship between respondents’ knowledge of obstetric danger signs and their socio-demographic variables shows that there is no significant association between respondents’ knowledge of obstetric danger signs and their age and marital status with a p-value>0.05. There is a significant association between respondents’ knowledge of obstetric danger signs and their level of education and parity with a p-value <0.05.
| Overall practice | Good (%) | Poor (%) | Total (%) | X2 | df | p-value |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Below 20 | 4 (57.1) | 3 (42.9) | 7 (100.0) | 8.303 | 3 | 0.040 |
| 21-30 | 116 (86.6) | 18 (13.4) | 134 (100.0) | |||
| 31-40 | 93(85.3) | 16(14.7) | 109(100.0) | |||
| Above 40 | 20(100.0) | 0 | 20(100.0) | |||
| Marital status | ||||||
| Single | 5(100.0) | 0 | 5(100.0) | 0.809 | 1 | 0.368 |
| Married | 228(86.0) | 37(14.0) | 265(100.0) | |||
| Level of education | ||||||
| No formal education | 0 | 3(100.0) | 3(100.0) | 27.201 | 3 | <0.001 |
| Primary | 3(50.0) | 3(50.0) | 6(100.0) | |||
| Secondary | 42(84.0) | 8(16.0) | 50(100.0) | |||
| Tertiary | 188(89.1) | 23(10.9) | 211(100.0) | |||
| Parity | ||||||
| None | 121(85.2) | 21(14.8) | 142(100.0) | 3.082 | 4 | 0.544 |
| Once | 53(86.9) | 8(13.1) | 61(100.0) | |||
| Twice | 42(84.0) | 8(16.0) | 50(100.0) | |||
| 3 times | 9(100.0) | 0 | 9(100.0) | |||
| More than 3 times | 8(100.0) | 0 | 8(100.0) | |||
Table 6 Relationship between respondents’ Practice on birth preparedness and their socio-demographic variables shows that there is no significant association between respondents’ Practice on birth preparedness and their marital status and parity with a p-value >0.05. But there is a significant association between respondents’ Practice on birth preparedness and their age and level of education with a p-value <0.05.
Discussion
Socio-demographic characteristics
The result of this study showed that majority of the respondents 134 (49.6%) were within the age range 21-30. Most of the respondents 265 (98.1%) were married and 211 (78.1%) of the respondents had tertiary education. More than half of the respondents 163 (60.4%) were practicing Christianity. This result is similar to that of Oni et al. [33] in their study on a comparative assessment of the awareness of danger signs and practice of birth preparedness and complication readiness among pregnant women attending rural and urban general hospitals in Lagos State which revealed that 54.5% of the respondents were within 20-29 years, 92.6% were married (92.6%) and most of the respondents were Christians (78.4%).
Clinical characteristics of respondents
Half of the respondents 136 (50.4%) number of gravidity is one and only 37 (13.7%) had gravidity of more than 3 times. More than half of the respondents 142 (52.6%) are nulli-parous while 61 (22.6%) of the respondents parity is one. Most of the respondents 116 (43.0%) had less than 4 number of ANC visits while 30 (11.1%) had between 9-12 times of ANC visits. Most of the respondents 157 (58.1%) were in their third trimester and more than half of the respondents 145 (53.7%) had no previous delivery. Only 26 (9.6%) of the respondents have had history of still birth and health problem during previous pregnancy.
Assessing the level awareness of obstetric danger signs
This study showed that majority of the respondents (60.7%) had good knowledge of obstetric danger signs. This is dissimilar to the study conducted by John in a cross sectional study carried out on awareness of birth preparedness and complication readiness in south-eastern Nigeria indicated that although awareness of the concept of birth preparedness was high (70.6%), knowledge of specific key danger signs was poor. The result of this study is also inconsistent with that of Pembe [10] on Rural Tanzanian women's Awareness of Danger Signs of Obstetric Complications which reported that Studies in low-income countries show that knowledge of obstetric danger signs especially during pregnancy and delivery among women is deficient. In this study only 19.6% of the respondents reported that they don’t know the danger signs during pregnancy that can endanger the life of a woman 38 (14.1%) of the respondents identified bleeding as a danger sign during pregnancy. Placental not delivered 30 minutes after baby was identified by 117 (43.3%) as a danger sign during labour that they know can endanger the life of a woman while 104 (38.5%) said they don’t know. 72 (26.7%) also identified severe bleeding as a danger sign after labour that could endanger the life of a woman, Wafaa [28] in their study on Women’s Awareness of Danger Signs of Obstetrics. Alexandria, Egypt, revealed that Obstetric danger signs include persistent vomiting, severe persistent abdominal pain, vaginal bleeding during pregnancy and delivery, severe vaginal bleeding after delivery, swelling of face, fingers and feet, blurring of vision, fits of pregnancy, severe recurrent frontal headache, high grade fever, marked change in fetal movement, awareness of heart beats, high blood pressure, sudden escape of fluid from the vagina, dysuria, oliguria or anuria, prolonged labour, loss of consciousness and retained placenta.
Assessing the practice of birth preparedness
Majority of the respondents 209 (77.4%) knew their expected date of delivery and most of them 240 (88.9%) reported that it is possible for labour to start before due date. Most of the respondents 228 (84.4%) reported that they have identified the facility they will give birth. More than half of the respondents 204 (75.6%) reported that they will give birth in a government hospital. Most of the respondents 185 (68.5%) reported that they have already arranged for a blood donor and most of the respondents 222 (82.2%) said they are saving money in case of emergency during delivery.
The result of this study showed that majority of the respondents (86.3%) had good practice on birth preparedness. This result disagrees with a study Ajibola [34] on birth Preparedness and Complication Readiness among Women. Attending Antenatal Clinic in Ogbomoso (Southwest, Nigeria) which revealed that only 40.3% of the respondents were reported well prepared for births and were complication ready. Also, according Makunyi [26] in a study carried out on Birth preparedness among women in Tharaka Nithi county, Kenya revealed that the proportion of women that were prepared for birth were low (20.3%).
Conclusion
The result of this study has shown that greater percentage of the respondents have adequate knowledge of the danger signs during pregnancy and likewise practice of birth preparedness was also good. Although some of the respondents could not identify the danger signs during pregnancy as well as during labour. This calls for proper health education and awareness programme about the danger signs of pregnancy as well as the importance of proper preparedness of birth. Activities designed to improve practice of birth preparedness are recommended particularly for women who lack knowledge of danger signs of pregnancy and birth preparedness.
Implication to nursing
Birth Preparedness is the process of planning for normal birth and anticipating the actions needed in case of an emergency. Nurses/ midwives should assist the women to share the responsibility of birth preparedness among all safe motherhood stakeholders; policy makers, facility managers, providers, communities, families, and women because a coordinated effort is needed to reduce the delays that contribute to maternal and new born deaths. Nurses should encourage women to discuss and review their birth preparedness plan with a skilled attendant at every antenatal care (ANC) assessment and one month before the expected date of birth. The nurses should also draw plans for birth and emergency preparedness which will include identification of the following elements:- the desired place of birth, the preferred birth attendant, the location of the closest appropriate care facility, funds for birth- related and emergency expenses, a birth companion, support in looking after the home and children while the woman is away, transport to a health facility for the birth, transport in the case of an obstetric emergency and identification of compatible blood donors in case of emergency.
Recommendations
Based on the findings from this study the following are recommended:
1. There is need to intensify education on danger signs during pregnancy and during labour in order to promote child and maternal health.
2. There should be improved awareness of women both at community and institutional level and reinforced counselling on obstetric danger signs at Antenatal Care.
3. Pregnant women should be given necessary support needed both financially and easy access to ANC clinics in order to prevent the danger signs.
4. For each visit to the ANC clinic the nurse/midwife should discuss the danger signs during pregnancy and ways to prevent them to the women.
Suggestions for further studies
1. Studies conducted to ascertain the reasons why some women lack the practice of birth preparedness.
2. A larger sample size should be used in a different location to ascertain the result of this study.
References
- UNICEF (2009) Half a million women die from pregnancy complications each year.
- World Health Organization (2014) Maternal Mortality: Fact Sheet 348. Geneva, Switzerland.
- WHO, UNICEF, UNFPA (2017-2019) The World Bank, United Nations population division. Trends in maternal mortality: 1990 to 2013.
- Doctor HV, Findley SE, Afenyadu GY (2012) Estimating maternal mortality level in rural northern Nigeria by the sisterhood method. International Journal of Population Research 2012: 5
- Affipunguh PK, Laar AS (2016) Assessment of knowledge and practice towards birth preparedness and complication readiness among women in Northern Ghana: a cross-sectional study. Int J Sci Rep 2: 121.
- Magoma M, Requejo J, Campbell OM, Cousens S, Filippi V (2010) High ANC coverage and low skilled attendance in a rural Tanzanian district: a case for implementing a birth plan intervention. BMC Pregnancy and Child Birth 10: 13.
- Kakaire O, Kaye DK, Osinde MO (2011) Male involvement in birth preparedness and complication readiness for emergency obstetric referrals in rural Uganda. Reproductive Health 8: 12.
- Hussein J, Kanguru L, Astin M, Munjanja S (2012) The effectiveness of emergency obstetric referral interventions in developing country settings: a systematic review. PLoS Med 9: e1001264.
- Kushwah SS, Dubey DK (2008) A Study for Assessing Birth Preparedness and Complication Readiness Intervention in Rewa District of Madhya Pradesh Chief Investigator, India. (Department of Community Medicine, SS Medical College, Rewa, MP). 2008:9.
- Pembe AB, Urassa P, Carlstedt A, Lindmark G, Nystrom L, et al. (2009) Rural Tanzanian women's Awareness of Danger Signs of Obstetric Complications. Biomed Central BMC Pregnancy and Child Birth 9: 12.
- Hiluf M, Fantahun M (2008) Birth Preparedness and Complication Readiness among Women in Adigrat Town, North Ethiopia. Ethiop J Health Dev 22: 14-20.
- Kaso M, Addisse M (2014) Birth preparedness and complication readiness in Robe Woreda, Arsi Zone, Oromia Region, Central Ethiopia: a cross-sectional study. Reprod Health 11: 55.
- Mutiso SM, Qureshi Z, Kinuthia J (2008) Birth preparedness among antenatal clients. East Afr Med J 85: 275-283.
- Ekabua JE, Ekabua KJ, Odusolu P, Agan TU, Iklaki CU, et al. (2011) Awareness of birth preparedness and complication readiness in southeastern Nigeria. ISRN Obstet Gynecol 2011: 1-6.
- Agarwal S, Sethi V, Srivastava K, Jha PK, Baqui AH (2010) Birth preparedness and complication readiness among slum women in Indore city, India. J Health Popul Nutr 28: 383-391.
- Raj A, Saggurti N, Balaiah D, Silverman JG (2009) Prevalence of child marriage and its effect on fertility and fertility-control outcomes of young women in India: a cross-sectional, observational study. The Lancet 373: 1883-1889.
- Singh PK, Rai RK, Alagarajan M, Singh L (2012) Determinants of Maternity Care Services Utilization among Married Adolescents in Rural India. PLoS ONE 7: e31666.
- GabryschS, Campbel OM (2009) Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Child Birth 11: 34.
- Babaloba S, Fatusi A (2009) Determinant of use of maternal health services in Nigeria-looking beyond individual and household factors. BMC Pregnancy Child Birth 9: 43.
- Kiyugu OD (2009) Analysis of factors that contribute to high number of Maternal deaths in Singida region in Tanzania, Royal Tropical Institute, Amsterdam.
- Deoki N, Kushwah SS, Dubey DK, Singh G, Shivdasani S, et al. (2008) A Study for Assessing Birth Preparedness and Complication Readiness Intervention in Rewa District of Madhya Pradesh Chief Investigator, India. (Department of Community Medicine, SS Medical College, Rewa, MP). 2008: 9.
- Ekabua JE, Ekabua KJ, Odusolu P, Agan TU, Iklaki CU, et al. (2011) Awareness of birth preparedness and complication readiness in southeastern Nigeria. ISRN Obstet Gynecol 2011: 1-6.
- Idowu A, Deji SA, Arem OA, Bojuwoye OM (2015) Birth preparedness and Complication readiness among women attending antenatal clinics in Ogbomoso, South West, Nigeria. Int J MCH AIDS 4: 47-56.
- Makunyi EG (2014) Birth preparedness among women in Tharaka Nithi county, Kenya. A thesis in partial fulfilment for the award of master’s in public health, School of Public Health of Kenyatta University.
- Agbodohu D (2013) Birth preparedness and complication readiness among expectant mothers at the Ridge Regional Hospital, Accra Doctoral Dissertation, University of Ghana.
- Kabakyenga JK, Östergren PO, Turyakira E, Pettersson KO (2011) Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health 8: 33.
- Anya SE, Hydara A, Jaiteh LE (2008) Antenatal care in The Gambia: missed opportunity for information, education and communication. BMC Pregnancy Child Birth 8: 9.
- Wafaa AR, Rasha ME(2010) Women’s Awareness of Danger Signs of Obstetrics . Alexandria, Egypt. Am J Sci1299-1306.
- Thaddeus S, Maine D (1994) Too far to walk: maternal mortality in context. Social Science & Medicine 38: 1091-1110.
- Ilo IJ (2015) Assessing Knowledge, Practice and Factors Influencing Birth Preparedness and Complication Readiness Among Couples in Selected Rural Communities in Oji River Local Government Area of Enugu State. (Doctoral Dissertation, University of Nigeria).
- Del Barco R (2004) Monitoring birth preparedness and complication readiness tool and indicator for maternal and new born care. pp: 330.
- Hailu M, Gebremariam A, Alemseged F, Deribe K (2011) Birth Preparednes and Complication Readiness among Pregnant Women in Southern Ethiopia. PLoS One 6: e21432.
- Oni B, Odukoya OO, Okunowo AA, Ojo OY, Abatan YO (2016) A comparative assessment of the awareness of danger signs and practice of birth preparedness and complication readiness among pregnant women attending rural and urban general hospitals in Lagos State. Sahel Med J 19: 206-214.
- Idowu A, Deji SA, Arem OA, Bojuwoye OM (2015) Birth preparedness and Complication readiness among women attending antenatal clinics in Ogbomoso, South West, Nigeria. Int J MCH AIDS 4: 47-56.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences