Pancreaticoduodenal Artery Aneurysm Secondary to Median Arcuate Ligament Syndrome Treated with Preserving Pancreas and Reimplantation of the Celiac Trunk
Cihan Agalar1*, Tufan Egeli1, Mücahit Özbilgin1, Tarkan Unek1,Sevket Baran Ugurlu2 and Ibrahim Astarcıoğlu1
1Department of General Surgery, Medical School, Dokuz Eylul University, Izmir, Turkey
2Department of Heart and Vascular Surgery, Medical School, Dokuz Eylul University, Izmir, Turkey
- *Corresponding Author:
- Cihan Ağalar
Department of General Surgery
Medical School, Dokuz Eylul University
Izmir 35340, Turkey
Tel: +90 506 2922575
Fax: +90 232 4122388
E-mail: cihan.agalar@deu.edu.tr
Received Date: October 30, 2017; Accepted Date: November 25, 2017; Published Date: December 07, 2017
Citation: Agalar C, Egeli T, Özbilgin M, Unek T, Ugurlu SB, et al. (2017) Pancreaticoduodenal Artery Aneurysm Secondary to Median Arcuate Ligament Syndrome Treated with Preserving Pancreas and Reimplantation of the Celiac Trunk. Gen Surg Rep. Vol.1 No.1:6
Abstract
Visceral artery aneurysms are located only 1.3-2% in pancreaticoduodenal artery. Rupture risk is 15-22% and they are related to about 40% death if rupture occurs, rupture risk is not related to the aneurysm size. Pancreaticoduodenal artery aneurysm secondary median arcuate ligament syndrome was diagnosed in 45-years old female. Because of the big size of aneurysm which was 3.5 centimetres in diameter, instead of embolization the aneurysm was treated by open surgical approach with resection of the aneurysm with preventing head of pancreas and re-implantation of celiac trunk to the abdominal aorta. Regardless of their size, pancreaticoduodenal artery aneurysms must be treated. The issue of treatment options of pancreaticoduodenal artery aneurysm is still controversial, recently endovascular treatment has become popular but open surgical repair is rational option for young patients with no malignancy, for whom long term survival is expected.
Keywords
Median arcuate ligament syndrome; Pancreaticoduodenal artery aneurysm; Visceral artery aneurysm
Introduction
The superior pancreaticoduodenal artery arise from the gastroduodenal artery and inferior pancreaticoduodenal artery (PDA) may arise directly from the superior mesenteric artery (SMA) or from the first jejunal branch of the SMA, these arteries divide into anterior and posterior branches. Anterior superior and anterior inferior arteries become confluent on anterior side of pancreatic head, posterior superior and inferior branches communicate with each other on posterior side of pancreatic head. These arteries generate collateral between the SMA and gastroduodenal artery [1].
Visceral artery aneurysms are infrequent conditions and found 0.1-0.2% in autopsy series [2]. They divided into two groups: true aneurysms and pseudo-aneurysms. True aneurysms are secondary to vessel wall malformations, pseudo-aneurysms are usually formed after inflammation and trauma [3]. Aneurysms occur mostly in splenic artery 46%, and renal artery 22%, only 1.3%-2% of them are located in PDA [4,5]. The risk of visceral artery aneurysm rupture is reported as 15-22% in literature [6] and they are related to about 40% death if rupture occurs [7].
Median arcuate ligament (MAL), was first anatomically reported by Lipshutz in 1917 [8], Harjola and Dunbar described the Median arcuate ligament syndrome (MALS) in respectively 1963 and 1965 [9,10]. Median arcuate ligament syndrome is an infrequent condition, characterized by narrowing and limiting of the celiac trunk by the median arcuate ligament [1]. With limiting celiac trunk, arterial blood flow of spleen, liver and stomach is decreased, to compensate this hypoperfusion situation, the blood flow of superior mesenteric artery (SMA) is increased and liver, stomach and spleen blood necessity is supplied through the SMA using by pancreaticoduodenal artery arcade. Chronically increased blood volume and hypertension on the small arteries, lead to endoluminal damage and true aneurysm formation occurs on collateral arteries [11]. This physiologic mechanism was described by Sutton and Lawton in 1973 [12]. Since Sutton and Lawton described the relationship between MALS and pancreaticoduodenal artery aneurysm, more than 600 cases with PDA aneurysm developed secondary to MALS [13] were reported in the literature. Most of the PDA cases with no relation to MALS were mostly associated with atherosclerosis in celiac artery and branches [14].
Case Presentation
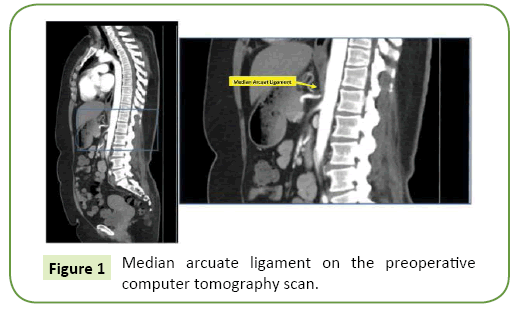
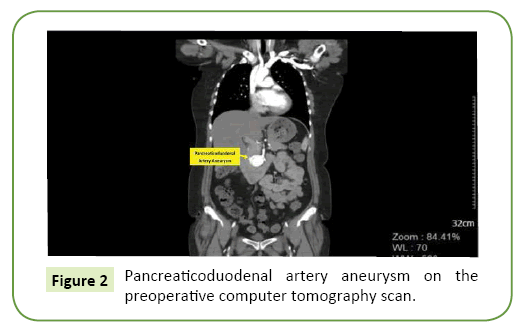
45-years old female with no medical history, apply to the emergency service with dysuria and abdominal pain. With suspicion of pyelonephritis, abdominal ultrasonography was performed and showed anechoic lesion close to the pancreatic head, Doppler ultrasonography was performed at the same time and it demonstrated enlarged, tortuous artery and turbulent arterial blood flow on posterior side of pancreatic head. After ultrasonography examination, abdominal computed tomographic angiography with intravenous contrast was performed and computer tomography demonstrated severe narrowing of the celiac trunk by the MAL (Figure 1) and aneurysm with about 3, 5 centimetres in diameter was seen on posterior side of pancreatic head (Figure 2). The aneurysm was between gastro duodenal artery and posterior inferior pancreatic duodenal artery.
Figure 2: Pancreaticoduodenal artery aneurysm on the preoperative computer tomography scan.
Firstly our interventional radiology department consult the patient but because of the aneurysm size they thought that this aneurysm was not appropriate for embolization.
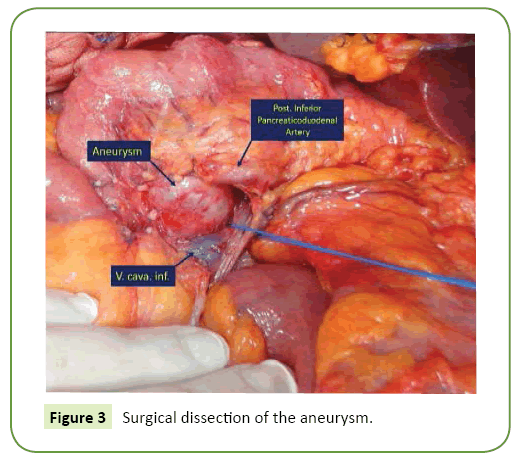
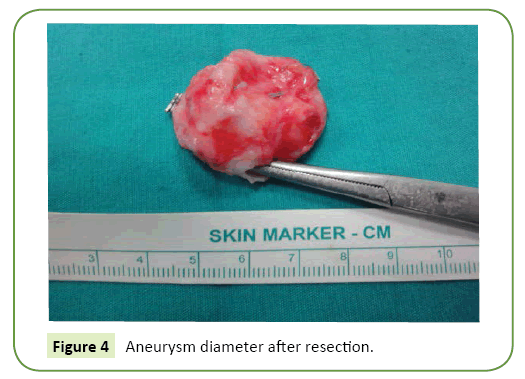
In general surgery department, we decided to perform urgent open surgery and started operation with bilateral subcostal incision, Kocher manoeuvre was completed. We saw aneurysm and we felt thrill blood flow on posterior side of pancreatic head. The superior mesenteric artery (SMA) vascularized the celiac arterial zone through the PDA arcade. Gastro duodenal artery was dissected carefully and prepared for clamping, right medial visceral rotation manoeuvre (Cattel-Braasch) was performed and proximal territory of superior mesenteric artery was prepared for clamping, in case the risk of bleeding. We dissected the aneurysm carefully from the pancreas (Figures 3 and 4).
Figure 4: Aneurysm diameter after resection.
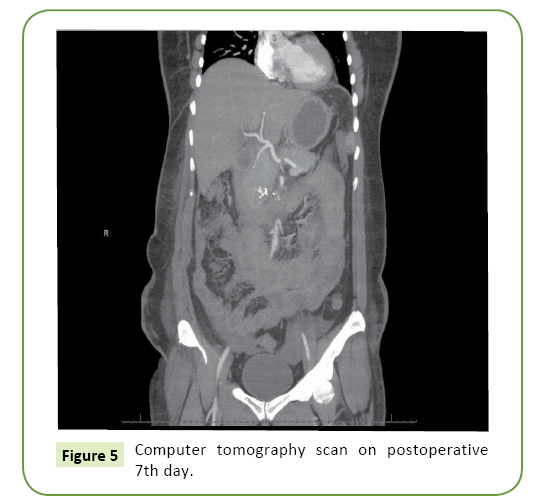
MAL was transsected henceforth we saw that celiac artery was very weak. Perioperative Doppler ultrasonography was performed by the radiologist and Doppler ultrasonography proved us there was no blood flow in celiac artery. Re-implantation of the celiac artery was decided. After systemic heparinization the celiac artery was re-implanted end-to-side to the aorta with 6-0 polypropylene sutures. There was a good pulsation in the celiac artery and branches after anastomosis, and there was no sign of ischemia on liver after revascularization. Doppler ultrasonography was performed again and vigorous blood flow was shown in celiac artery and branches. The patient had no postoperative complications, no increase of transaminases and discharged on ninth postoperative day. On postoperative seventh day, computer tomographic angiography was performed again and good arterial distribution was seen on celiac artery and branches (Figure 5). Patient gave informed consent about the publishing of her operation data and documents for scientific purposes.
Discussion
Patients with visceral artery aneurysm mostly complain about abdominal pain, other symptoms may be jaundice, lack of appetite, melena and hypovolemic shock symptoms secondary to aneurysm rupture. More than 60% of patients who had pancreaticoduodenal artery aneurysm firstly are presented with rupture [15]. Rupture risk is not related to the aneurysm size, in literature ruptured aneurysms diameters ranged between 0.7 cm and 2 cm. On the other hand unruptured aneurysms sizes between 0.7 cm and 6 cm [1].
The rupture risk of pancreaticoduodenal artery aneurysms is about 65%. Among the 88 patients published in the literature with pancreaticoduodenal artery aneurysm, 53 patients had rupture, 26 patients died by the reason of ruptured aneurysm [16].
Regardless of their size, pancreaticoduodenal artery aneurysms must be treated. Open surgical approach is the standard treatment for the patients with ruptured aneurysm. In nonruptured patient group, treatment options are interventional radiology and surgery. Recently endovascular treatment which involves stent and coil embolization has become highly popular and has less mortality and morbidity rates. If the aneurysm is small and the patient does not have chronic abdominal pain, endovascular treatment must be the first choice for treatment. In large aneurysm resection is feasible option, after resection of aneurysm; vascular reconstruction is not always needed. Collateral arterial branches supply the blood flow.
Our first choice in this patient was endovascular treatment but due to the aneurysm size we performed open surgery. After the resection of aneurysm, the condition of celiac trunk needed additional procedure, treatment options were endovascular stent placement to the celiac trunk and re-implantation. We chose re-implantation for young and non-malignant patient.
The issue of treatment options of pancreatic duodenal artery aneurysm is still controversial. Endovascular treatment is less invasive than surgery but suggested treatment is to liberate the MAL and revascularization of the celiac trunk [17,18]. Recently two publications from Germany and Japan showed that the patient group who underwent resection of aneurysm and revascularisation of celiac artery had successful results for life quality in long term follow up [2,19].
In the literature, most of the cases were treated with open surgery but the method of laparoscopic MAL release was first reported in USA [20].
Conclusion
We conclude that, open surgical treatment is a rational option for young patients with no malignancy who had big size pancreatic duodenal artery aneurysm secondary to MALS, for whom long term survival is expected.
References
- Kallamadi R, DeMoya M, Kalva SP (2009) Inferior pancreaticoduodenal artery aneurysms in association with celiac stenosis/occlusion. SeminIntervent Radiol 26: 215-223.
- Grotemeyer D, Duran M, Park EJ, Hoffmann N, Blondin D, et al. (2009) Visceral artery aneurysms - Follow-up of 23 patients with 31 aneurysms after surgical or interventional therapy. Langenbeck’s Arch Surg 394: 1093-1100.
- Iyori K, Horigome M, Yumoto S, Yamadera Y, Saigusa Y, et al. (2004) Aneurysm of the gastroduodenal artery associated with absence of the celiac axis: Report of a case. Surg Today 34: 360-362.
- Deterling RA (1971) Aneurysm of the visceral arteries. J Cardiovasc Surg12: 309-322.
- Pasha S, Gloviczki P, Stanson AW, Kamath PS (2007) Splanchnic artery aneurysms. Mayo Clin Proc 82: 472-479.
- Guntani A, Yamaoka T, Kyuragi R, Honma K,Iwasa K, et al. (2011) Successful treatment of a visceral artery aneurysm with a celiacomesenteric trunk: Report of a case. Surg Today 41: 115-119.
- Lee PC, Rhee RY, Gordon RY, Fung JJ, Webster MW(1999) Management of splenic artery aneurysms: The significance of portal and essential hypertension. J Am Coll Surg 189: 483-490.
- Lipshutz B (1917) Acomposite study of the coeliac axis artery. Ann Surg 65: 159-169.
- Harjola PT (1963) A rare obstruction of the coeliac artery. Report ofa Case. Ann Chir Gynaecol Fenn 52: 547-550.
- Dunbar JD, Molnar W, Beman FF, Marable SA (1965) Compression of the celiac trunk and abdominal angina: preliminary report of 15 cases. Am J Roentgenol 95: 731-744.
- Kalva SP, Athanasoulis C, Greenfield J, Curvelo M, Waltman C, et al. (1965) Inferior pancreaticoduodenal artery aneurysms in association with celiac axis stenosis or occlusion. Eur J Vasc Endovasc Surg 33: 670-675.
- Sutton D, Lawton G (1973) Coeliac stenosis or occlusion with aneurysm of the collateral supply. Clin Radiol 24: 49-53.
- De Perrot M, Berney T, Deleaval J, Bühler L, Mentha G, et al. (1999) Management of true aneurysms of the pancreaticoduodenal arteries. Ann Surg 229: 416-420.
- Chiang KS, Johnson CM, McKusick MA, Maus TP Stanson AW (1994) Management of inferior pancreaticoduodenal artery aneurysms: a 4-year, single center experience. Cardiovasc Interv Radiol 17: 217-221.
- Moore E, Matthews MR, Minion DJ, Quick R, Schwarcz TH, et al. (2004) Surgical management of peripancreatic arterial aneurysms. J Vasc Surg 40: 247-253.
- Miyayama S, Terada T, Tamaki M(2015) Ruptured pancreaticoduodenal artery aneurysm associated with median arcuate ligament compression and aortic dissection successfully treated with embolotherapy. Ann Vasc Dis 8: 40-42.
- Takach TJ, Livesay JJ, Reul GJ, Cooley DA (1996) Celiac compression syndrome: Tailored therapy based on intraoperative findings. J Am Coll Surg 183: 606-610.
- Palmer OP, Tedesco M, Casey K, Lee JT, Poultsides G (2012) Hybrid treatment of celiac artery compression (median arcuate ligament) syndrome. Dig Dis Sci 57: 1782-1785.
- Nishiyama A, Hoshina K, Hosaka A, Okamoto H, Shigematsu K, et al. (2013) Treatment strategies for a pancreaticoduodenal artery aneurysm with or without a celiac trunk occlusive lesion. Ann Vasc Dis 6: 725-729.
- Duffy AJ, Panait L, Eisenberg D, Bell RL, Roberts KE, et al. (2009) Management of median arcuate ligament syndrome: A new paradigm. Ann Vasc Surg 23: 778-784.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences