Magnetic Resonance Imaging Findings in Chronic Inflammatory Demyelinating Polyradiculoneuropathy: Report of Two Cases
1Department of Neurology, Military Hospital, Tunis, Tunisia
2Department of Physiology, Medical School, Tunis, Tunisia
- *Corresponding Author:
- Mansour M
Department of Neurology
Military Hospital, Tunis, Tunisia
Tel: +21655939393
E-mail: ichard.sadig1@my.nd.edu.au
Received Date: October 30, 2017; Accepted Date: November 13, 2017; Published Date: November 27, 2017
Citation: Mansour M, Laabidi K, Rachdi A, Riahi A, Zaouali J, et al. (2017) Magnetic Resonance Imaging Findings in Chronic Inflammatory Demyelinating Polyradiculoneuropathy: Report of Two Cases. J Nerv Syst Vol.1 No.1:2
Introduction
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired peripheral neuropathy of presumed autoimmune etiology. It is considered to be an autoimmune disorder of the peripheral nervous system (PNS). Magnetic resonance imaging (MRI) evidence of central nervous system (CNS) demyelinating lesions in CIDP is rare. We present MRI features in two male patients with CIDP.
Case Reports
Case 1
Mr. AB, a 45 years old man, truck driver, off work since an accident causing amputation of the right arm in 1993. He presented in March 2003 with a two-year history of slowly progressive sensory disturbance involving lower limbs gradually associated with gait disorder. His medical history was unremarkable and there was no family history of neuromuscular disease.
Initial neurological assessment revealed paraparesis but the gait was still being possible unaided. Romberg's test was positive.
Reflexes in the lower limbs were absent with bilateral extensor plantar. There was a thermo-algic hypoesthesia in the left side of the body. Examination also showed propioceptive impairment in the right lower limb and dysmetria in the left upper limb.
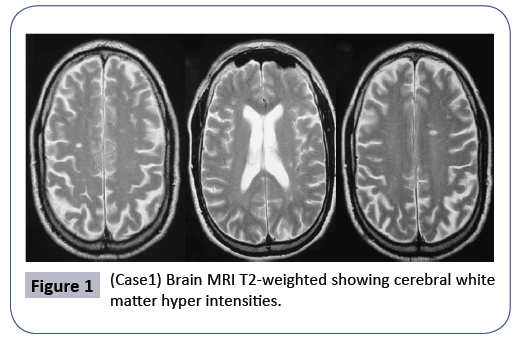
Brain MRI revealed T2 hyper intensities of the cerebral white matter Figure 1. We did not identify any MRI abnormalities in the spinal cord. The study of visual evoked potentials revealed a bilateral lengthening of the P100 wave latency, suggesting bilateral demyelinating optic neuropathy. Auditory evoked potentials were also in favor of a demyelinating lesion. The somatosensory evoked potentials of tibial nerves were abnormal: absence of N21 responses of cortical events. Based on these clinical and radiological findings, the diagnosis of inflammatory disease of the central nervous system was established. The patient was treated with intravenous methylprednisolone and he had partial clinical improvement.
Figure 1: (Case1) Brain MRI T2-weighted showing cerebral white matter hyper intensities.
Nerve conduction studies were consistent with a chronic sensorimotor demyelinating peripheral neuropathy, with slow nerve conduction velocities, absent F responses in lower and upper limbs and evidence of conduction blocks.
Lumbar MRI showed D11-D12 and L1 disc space narrowing. At that time, cerebral spinal fluid (CSF) analysis revealed protein level of 0.66 g/l, normal glucose level without cells and no oligoclonal bands.
The diagnosis of CIDP with CNS involvement was made. Brain MRI showed remained identical. Standard hematological and biochemical tests were normal. Screening for auto antibodies was negative. The immunological tests were normal. Tumor markers were negative, as well as infectious serology.
Thoracic scan was performed and showed two calcified nodule in the right upper lobe. Pooled intravenous immunoglobulin therapy (0.4g/kg/day) over five days led to mild improvement in sensory and gait impairment.
The patient was discharged on oral prednisolone. He relapsed later several times, during steroid tapering and the same pattern of symptoms developed. Steroid dose was gradually reduced because of side effects. The introduction of azathioprine then mycophenolate mofetil was therefore decided to help improve neurological status.
Case 2
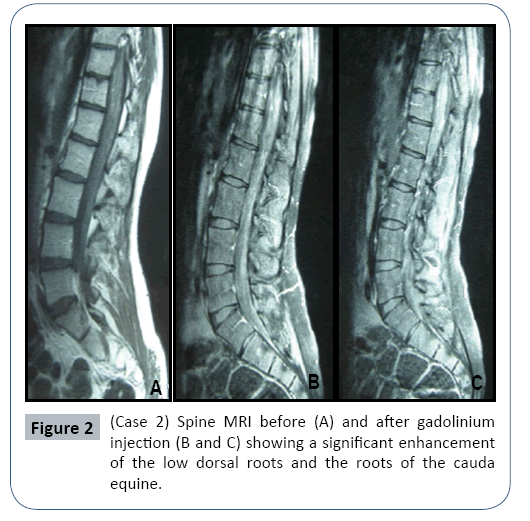
In June 2006, a 17 years old man presented with a three-month history of numbness and tingling in the lower limbs. These symptoms gradually spread to his trunk and were associated with gait disturbance. He had no medical history. Neurological examination showed proximal and distal weakness, diffuse areflexia. Routine laboratory tests were normal. CSF analysis revealed no cells, normal glucose and increased protein at 2.5 g/l. Brain MRI was normal, but spinal MRI disclosed enhancement of lumbosacral nerve roots by gadolinium Figure 2. Electroneuromyogram (ENMG) revealed denervation potentials in proximal and distal muscles. Nerve conduction studies showed reduced sensory and motor action potentials and slowing of nerve conduction and motor conduction blocks, in keeping with a demyelinating polyneuropathy. These neurophysiological and pathological findings supported the diagnosis of CIDP.
Associated immune disorders such as infectious diseases, inflammatory bowel diseases, lymphoma, monoclonal gammopathy of undetermined significance (MGUS), connective tissue disorders and diabetes mellitus were excluded through either clinical data or appropriate laboratory investigations. Subsequently, the disease had showed relapsing-remitting course. Indeed, the patient relapsed twice in 2008 and 2011. The relapses were treated with three days course of intravenous pulsed methylprednisolone (1g per day) with resulting improvement.
Discussion
The diagnostic criteria for CIDP are usually based on clinical presentation, CSF analysis and electrophysiological findings, rather than MRI features [1]. In fact, MRI has not been widely used as a diagnostic tool in the CIDP. Radiological features of CNS involvement in CIDP are rare and seldom reported.
Although peripheral myelin is targeted by an autoimmune attack, CNS involvement has been suggested in a fraction of CIDP patients with the presence of subclinical electrophysiological and MRI abnormalities. The incidence of lesions ranges from 3 to 23%, but in many studies, specific imaging criteria for CNS demyelination were not clearly defined [2,3].
The occurrence of CNS lesions was not noted in any of the series of 53 cases of CIDP reported by Dyck et al. or the series of 92 documented CIDP by Combe et al. [4].
However, some reports had already documented the infrequent coexistence of peripheral and CNS demyelination [5,6]. Six of sixteen patients with established CIDP examined by Mendell et al. were found to have periventricular, subcortical or brainstem white matter lesions on MRI [7]. Three of these patients were preselected because of clinical evidence of central involvement, but none of the other three patients had clinical features suggesting CNS demyelination. The three asymptomatic patients were all older than 70 years. At that age, it is not uncommon to see such MRI patterns in completely asymptomatic individuals.
In the electrophysiological study by Ormerod et al. [5], six of 18 patients (33%) had unilateral or bilateral abnormalities in central motor conduction time on motor evoked potentials. On brain MRI, a third to a half of CIDP patients have been reported to have brain lesions [8,9] Bouchard et al. on the other hand, found a much lower incidence with only 5% in a series of 100 patients with CIDP having symptomatic CNS involvement [4]. It is suggested that these features are characteristic and strongly supportive of the diagnosis of CIDP with a prolonged clinical course.
More recent studies employing MRI and evoked potential recordings showed that subclinical brain abnormalities are encountered in a small proportion of CIDP patients, whereas concurrent severe CNS disease is rare [10,11].
Our first patient, who had sus tentorial white matter lesions, had a severe clinical course of the illness with non-response to immunotherapies.
The pathophysiological link that bridges peripheral and central demyelinating disorders in CIDP is unknown [12-14].
Spine MRI is a valuable addition to the diagnostic armamentarium in CIDP [15]. Enlarged spinal roots may be identified in patients being investigated for a demyelinating polyneuropathy or, as in our patient, may be discovered unsuspectingly when root disease is being considered. Even in the absence of nerve root thickening, abnormal enhancement of the cauda equina after intravenous gadolinium may be demonstrable in CIDP as well as in acute upper motor neuron features of more widespread CNS dysfunction have been reported in a proportion of patients with CIDP [16].
Other authors have underlined the fact that the nerve pathology in CIDP is relatively non-specific and that clinical and electro diagnostic assessment usually suffices to make the diagnosis [17,18].
All previous series with a single exception had focused on the brain. To the best of our knowledge, we are aware of two studies that investigated the spinal cord in patients with definite and possible CIDP using MRI with gadolinium enhancement [19,20]. In the series by Panagiotis et al. [21] in 2014, two out of twelve of patients presented a clear clinical spinal cord syndrome and radiological findings compatible with spinal cord demyelination [5].
Thickening in the spinal nerve roots and peripheral nerves in the lumbar and brachial plexuses has been reported as one of the characteristic features of CIDP in adult series with a prolonged clinical course [22].
Conclusion
Our cases support earlier observations that a minority of CIDP patients may additionally develop CNS involvement of variable degree and demonstrate that MRI can be a useful part of initial investigations in all suspected cases of CIDP. It may in such cases contribute to reaching the diagnosis and to the subsequent therapeutic decision making in these patients.
References
- Bril V, Banach M, Dalakas MC, Deng C, Donofrio P, et al. (2010) Electrophysiologic correlations with clinical outcomes in CIDP. Muscle Nerve 42: 492-497.
- Stojkovic T, De Seze J, Hurtevent JF, Arndt C, Beaume A, et al. (2000) Visual evoked potentials study in chronic idiopathic inflammatory demyelinating polyneuropathy. Clin Neurophysiol 111: 2285-2291.
- Dyck PJ, Lais AC, Ohta M, Bastron JA, Okazaaki H, et al. (1975) Chronic inflammatory polyradiculoneuropathy. Mayo Clin Proc 50: 621-637.
- Combe PA, Pollard JD, Leod JG (1987) Chronic inflammatory demyelinating polyradiculoneuropathy. A clinical and electrophysiological study of 92 cases. Brain 110: 1617-1630.
- Ormerod IEC, Waddy HM, Kermode AG, Murray NMF, Thomas PK (1990) Involvement of the central nervous system in
- chronic inflammatory demyelinating polyneuropathy: A clinical, electrophysiological and magnetic resonance imaging study. J Neurol Neurosurg Psychiatry 53: 789-793.
- Charil A, Yousry TA, Rovaris M, Barkhof F, De Stefano N, et al. (2006) MRI and the diagnosis of multiple sclerosis: expanding the concept of ‘‘no better explanation’’. Lancet Neurol 5: 841-852.
- Mendell JR, Kolkin S, Kissel JT, Weiss KL, Chakeres DW, et al. (1987) Evidence for central nervous system demyelination in chronic inflammatory demyelinating polyradiculoneuropathy. Neurology 37: 1291-1294.
- Rotta FT, Sussman AT, Bradley WG, Ram Ayyar D, Sharma KR, et al. (2000) The spectrum of chronic inflammatory demyelinating polyneuropathy. J Neurol Sci 173: 129-139.
- Hawke SHB, Hallinan JM, Mcleod JG (1990) Cranial magnetic resonance imaging in chronic inflammatory demyelinating polyneuropathy. J Neurol Neurosurg Psychiatry 53: 794-796.
- Tanaka K, Mori N, Yokota Y, Suenaga T (2013) MRI of the cervical nerve roots in the diagnosis of chronic inflammatory demyelinating polyradiculoneuropathy: a single institution, retrospective casecontrol study. BMJ Open 3: 003443. 11 Gungor L, Gungor I, Ozturk HE, Onar MK (2011) Visual Evoked Potentials in Guillain-Barre Syndrome. J Clin Neurol 7: 34-39.
- Pineda AA, Ogata K, Osoegawa M, Murai H, Shigeto H, et al. (2007) A distinct subgroup of chronic inflammatory demyelinating polyneuropathy with CNS demyelination and a favorable response to immunotherapy. J Neurol Sci 255: 1-6.
- Stoll G, Bendszus M, Perez J, Pham M (2009) Magnetic resonance imaging of the peripheral nervous system. J Neurol 256: 1043-1051.
- Zephir H, Stojkovic T, Latour P, Lacour A, De Seze J, et al. (2008) Relapsing demyelinating disease affecting both the central and peripheral nervous systems. J Neurol Neurosurg Psychiatry 79: 1032-1039.
- Staff NP, Figueroa JJ, Parisi JE, Klein CJ (2010) Hypertrophic nerves producing myelopathy in fulminant CIDP. Neurology 75: 750.
- De Silva RN, Willison HJ, Doyle D, Weir AI, Hadley DM, et al. (1994) Nerve root hypertrophy in chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 17: 168-170.
- Khadilkar SV, Visana DR, Huchche AM, Shah N, Gupta N, et al. (2013) Hypertrophic trigeminal nerves: moustache sign. Neurol India 61:566-567.
- Abe Y, Terashima H, Hoshino H, Sassa K, Sakai T, et al. (2015) Characteristic MRI features of chronic inflammatory demyelinating polyradiculoneuropathy. Brain Dev 7604: 22-24.
- De Smet K, De Maeseneer M, Talebian Yazdi A, Stadnik T, De Mey J (2013) MRI in hypertrophic mono-and polyneuropathies. Clin Radiol 68: 317-322.
- Bouchard C, Lacroix C, Plante V, Adams D, Chedru F, et al. (1999) Clinicopathologic findings and prognosis of chronic inflammatory demyelinating polyneuropathy. Neurology 52: 498-503.
- Loannidis P, Parissis D, Karapanayiotides T, Maiovis P, Karacostas D (2015) Spinal cord involvement in chronic inflammatory demyelinating polyradiculoneuropathy: a clinical and MRI study. Acta Neurol Belg 115: 141-145.
- Van den Bergh PY, Rajabally YA (2013) Chronic inflammatory demyelinating polyradiculoneuropathy. Presse Med 42: 203-215.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences