Laparoscopic Resection of Ileal GIST, Mimicking Acute Appendicitis
Cihan Ağalar1*, Sami Benli1, Berke Manoğlu2, Tufan Egeli1 and Mehtat Uz Unlu3
1Department of General Surgery, School of Medicine, Dokuz Eylul University, Izmir, Turkey
2Department of General Surgery Aydin State Hospital, Aydin, Turkey
3Department of Pathology, School of Medicine, Dokuz Eylul University, Izmir, Turkey
- *Corresponding Author:
- Cihan Ağalar
Department of General Surgery
School of Medicine, Dokuz Eylul University
Izmir 35340, Turkey
Tel: +90 506 2922575
Fax: +90 232 4122388
E-mail: cihan.agalar@deu.edu.tr
Received Date: November 02, 2017; Accepted Date: November 29, 2017; Published Date: December 10, 2017
Citation: Ağalar C, Benli S, Manoğlu B, Egeli T, Unlu MU (2017) Laparoscopic Resection of Ileal GIST, Mimicking Acute Appendicitis. Gen Surg Rep. Vol.1 No.1:7
Abstract
Gastrointestinal stromal tumour (GIST) is the most common mesenchymal neoplasm of the Gastrointestinal (GI) tract. Forty-nine years old man with no medical history was presented to the emergency service with abdominal pain, he underwent laparoscopic exploration with pre-diagnosed acute appendicitis. Ileal GIST was detected localized in the right - lower quadrant at the operation and resected by laparoscopically. Patients with GIST may be presented with various clinical symptoms including acute abdomen, Laparoscopic exploration allows the diagnosis and treatment at the same operation and laparoscopic surgery is a safe and reasonable option in small bowel GIST's.
Keywords
Tumour; Pain; Bowel; Neoplasm; Anesthesia; Laparoscopic; Surgery; Gastric
Introduction
Gastrointestinal stromal tumour (GIST) which originates from Cajal cells was firstly described by Mazur vs Clark in 1983 [1]. It is the most common Mesenchymal neoplasm of the Gastrointestinal (GI) tract [2]. GIST’s are mostly derived from stomach (60%) and small intestine (30%) in GI tract [3]. They mostly affect males (55%) and are usually diagnosed in fifth decade [4]. Presentation symptoms have a wide-spectrum including anemia, nausea, GI system bleeding, abdominal mass or acute abdomen [5]. In this case presentation, we aimed to publish our ileal GIST patient, who was presented with acute abdomen and underwent laparoscopic surgery.
Case Presentation
Forty-nine years old men with no medical history was presented to the emergency service with abdominal pain that started in mid umbilicus and placed to right lower-quadrant of abdomen five hours later. In physical examination abdominal guarding and rebound tenderness were detected on right-lower quadrant of abdomen. White blood cell count was 14000 in complete blood test. After evaluating these findings, laparoscopic exploration was decided because of pre-diagnosed acute appendicitis.
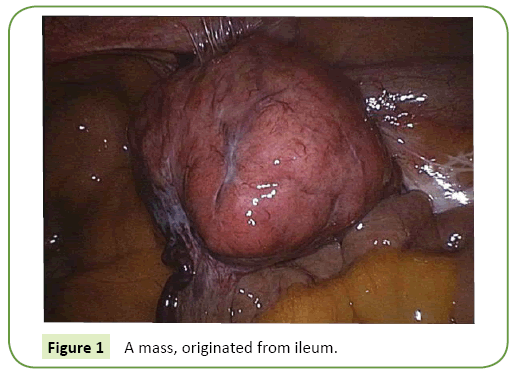
Under general anesthesia, 11 millimetres (mm) trocar was placed below the umbilicus, 30 degree endo camera was inserted to abdomen and a mass of approximately 6 cm in diameter, attached to abdominal wall below the lower right quadrant, was detected in laparoscopic exploration. The mass was originated from ileum and general appearance was similar with GIST (Figure 1). Adjacent tissues were gently dissected by considering the risk of tumor rupture and tumor was resected with segmental ileum. After completion of the resection, specimen was removed from the abdomen with using Alexis Contained Extraction System (Figure 2), side to side ileo-ileal anastomosis was performed extracorporeally. Patient was discharged uneventfully on postoperative fourth day.
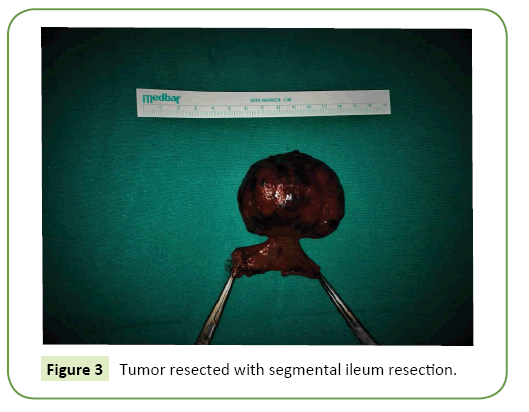
In histopathological examination, the tumor was diagnosed as GIST with size of 6.5 cm × 4.5 cm. diameter (Figure 3).
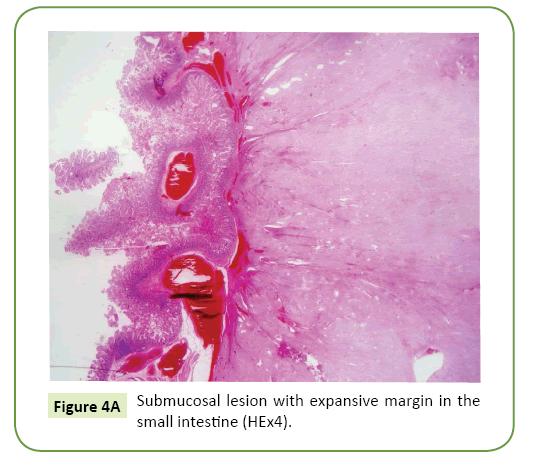
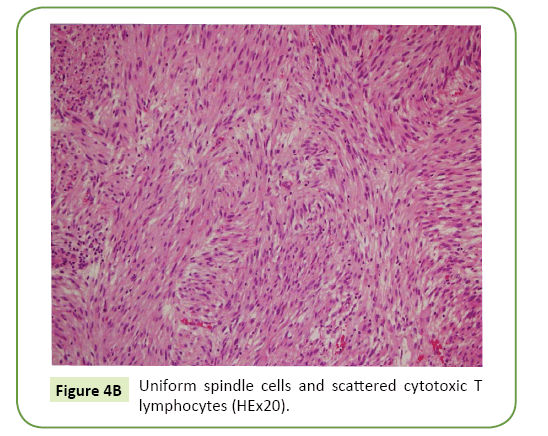
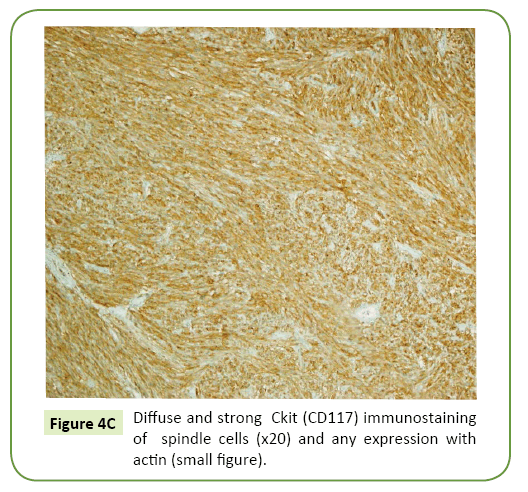
Mitosis count was 3 per 50 high power fields (HPF). Immunohistochemically, the tumor cells were positive for CD 117 and CD34 and negative for, Desmin and S100 (Figures 4A-4C). With these findings (>5 cm. in size and 3 mitoses per 50 HPF) the tumor was categorized in high risk group.
Figure 4B: Uniform spindle cells and scattered cytotoxic T lymphocytes (HEx20).
Figure 4C: Diffuse and strong Ckit (CD117) immunostaining of spindle cells (x20) and any expression with actin (small figure).
Contrast-enhanced Computerized Tomography (CT) was performed postoperatively for staging, no other tumor and/or metastasis was observed, adjuvant imatinib therapy was started to patient on postoperative first month and during 13 months follow-up period, no recurrence was detected.
Discussion
GIST’s can be located in anywhere in the GI tract. They usually originates from submucosa with exophytic growth pattern [5]. GIST is primarily caused by mutations in the KIT or plateletderived growth factor receptor A (PDGFRA) gene and CD117 (C-kit) is generally positive [3]. The prognosis of GIST is related with tumor size and mitotic activity [6], Miettinen et al. published their study in 2005, which included 1765 cases and they reported 86% metastasis in the group of tumors with >10cm tumor size and >5 mitosis per 50 HPF, on the other hand only 2% to 3% metastasis was observed in tumors with <10 cm size and <5 mitoses/50 HPF [7].
Gastrointestinal stromal tumors are fragile and capsular tumors, gentle manipulation is recommended during surgery to avoid tumor rupture. Spontaneously or surgical tumor rupture is an independent negative risk factor for disease-free survival [8,9]. Segmental or wedge resection with negative margin is the preferred surgical approach. Routine lymphadenectomy is not recommended due to low potential of nodal metastasis [10]. KIT inhibition and surgery are the main treatment modality, Imatinib is a selective KIT protein tyrosine kinase inhibitor [11], neoadjuvant Imatinib can be used for down-sizing and downstaging for un-resectable GIST’s [12].
Laparoscopic surgery is a safe and reasonable option in GIST’s. Compared to open surgery, laparoscopic surgery has better results in gastric GIST’s [13-15], Although there are limited publications about laparoscopic treatment in small bowel GIST’s minimal invasive surgery is much more recommended [16,17].
Laparoscopic surgery has advantages such as; less postoperative pain, shorter hospital stay, better cosmetic results, lower wound infection risk and faster return to normal bowel function, besides this advantages, if open surgery was preferred for our patient, tumor might get ruptured during McBurney incision. As a result of the preference of minimally invasive surgery, we could able to resect the tumor with intact capsule successfully by avoiding rupture, despite of the surrounding adhesions. For the GIST’s which are diagnosed peroperatively like in our case, surgical resection should be performed and tumor staging should be done during postoperative course.
Conclusion
In conclusion, patients with GIST may be presented with various clinical symptoms including acute abdomen, This case is presented to emphasize that the possibility of GIST should be kept in mind in the differential diagnosis of acute abdomen and to underline the advantages of laparoscopic resection for treatment of small bovel GIST’s.
References
- Mazur MT, Clark HB(1983) Gastric stromal tumors. Reappraisal ofhistogenesis. Am J Surg Pathol 7: 507-19.
- Sandvik OM, Søreide K, Kvaløy JT, Gudlaugsson E, Søreide JA (2011) Epidemiology of gastrointestinal stromal tumours: single-institution experience and clinical presentation over three decades. Cancer Epidemiol 35: 515-20.
- Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: Review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med 130:1466-1478.
- Van Der Zwan SM, DeMatteo RP DR (2005)Gastrointestinal stromal tumor: 5 years later. Cancer 104:1781-1788.
- Laurini JA, Carter JE (2010) Gastrointestinal stromal tumors: a review of the literature. Arch Pathol Lab Med 134:134-141.
- Miettinen M, Makhlouf H, Sobin LH, Lasota J (2006) Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol 30: 477-489.
- Miettinen M, Sobin LH Lasota J(2005) Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 29: 52-68.
- Hølmebakk T, Bjerkehagen B, Boye K, BrulandO,Stoldt S et al. (2016) Definition and clinical significance of tumour rupture in gastrointestinal stromal tumours of the small intestine. Br J Surg103: 684-691.
- Hohenberger P, Ronellenfitsch U, Oladeji O, Pink D, Ströbel P, et al.(2010) Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Br J Surg 97: 1854-18599.
- Giuliano K, Nagarajan N, Canner J, Najafian A, Wolfgang C, et al. (2017) Gastric and small intestine gastrointestinal stromal tumors: Do outcomes differ? J Surg Oncol 115: 351-357.
- Demetri GD, Von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, et al. (2014) NCCN Task Force Report: Update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8: S1–S44.
- Jakob J, Mussi C, Ronellenfitsch U, Wardelmann E, Negri T, et al. (2013) Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Ann Surg Oncol 20: 586-592.
- Pelletier JS, Gill RS, Gazala S, Karmali S (2015) Systematic Review and Meta-Analysis of Open vs. Laparoscopic Resection of Gastric Gastrointestinal Stromal Tumors. J Clin Med Res 7: 289-296.
- Koh YX, Chok AY, Zheng HL, Tan CS, Chow PK, et al. (2013) systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Surg Oncol 20: 3549-3560.
- Bischof DA, Kim Y, Dodson R, Carolina Jimenez M, Behman R etal. (2014) Open versus minimally invasive resection of gastric GIST: a multi-institutional analysis of short- and long-term outcomes. Ann Surg Oncol 21: 2941-2948.
- Nguyen SQ, Divino CM, Wang JL, Dikman SH (2006) Laparoscopic management of gastrointestinal stromal tumors. Surg Endosc 20: 713-716.
- Oida Y, Motojuku M, Morikawa G, Mukai M, Shimizu K, et al. (2008) Laparoscopic-assisted resection of gastrointestinal stromal tumor in small intestine. Hepato-gastroenterology 55: 146-149.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences