Laparoscopic Removal of Large Gangrenous Paraovarian Cyst in an Adolescent Girl
1Department of Obstetrics and Gynaecology, October 6th University and As-Salam International Hospital, Cairo, Egypt
2Department of General Surgery, El-Sahel Teaching Hospital and As-Salam International Hospital, Cairo, Egypt
- *Corresponding Author:
- Torky HA
Department of Obstetrics and Gynaecology
October 6th University and As-Salam International Hospital
Cairo
Egypt
Tel: +201001230161
E-mail: haithamtorky@yahoo.com
Received date: December 19, 2017; Accepted date: December 25, 2017; Published date: December 30, 2017
Citation: Torky HA, El-Sayed AA. Laparoscopic Removal of Large Gangrenous Paraovarian Cyst in an Adolescent Girl. J Biomed Sci Appl Vol. 1 No. 2:10.
Copyright: © 2017 Torky HA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Para ovarian cysts arise from the mesothelium lining of remnants of the Müllerian duct and Wolffian duct. They are mostly small and asymptomatic; however, torsion may occur in larger lesions. Case: A seventeen years old girl complained of acute abdominal pain. C.T. scan was arranged which revealed a large adnexal mass 82 × 63 mm. Doppler ultrasound showed absent blood flow to the adnexal mass. Laparoscopy revealed a large right torsion and gangrene in a Para ovarian cyst and right salpingo-oophorectomy was done via laparoscopy. Conclusion: Laparoscopy is preferred over laparotomy in the management of torsion of Para ovarian cysts as it is associated with shorter hospital stay and less patient discomfort. Salpingo-oophorectomy should be reserved to late gangrenous cases.
Keywords
Torsion; Para ovarian cyst; Laparoscopic management
Introduction
Paraovarian cysts are adnexal cysts lined by epithelium adjacent to the ovary and fallopian tubes. They arise from the mesothelium lining of remnants of the Müllerian and Wolffian ducts [1] and represent nearly 10% of adnexal masses [2].
They are mostly small and asymptomatic usually ranging between 1 and 8 cm in diameter 1 however, larger lesions of 20 or more cm have been reported giving rise to pressure symptoms and lower abdomen pain, in addition to, complications as torsion which causes acute abdominal pain and need surgical exploration and removal [3], with only few studies reporting successful laparoscopic management in such complicated cases.
The current case reports successful laparoscopic management of an adolescent girl presenting with acute abdominal pain due to torsion and gangrene of a Para ovarian cyst.
Case
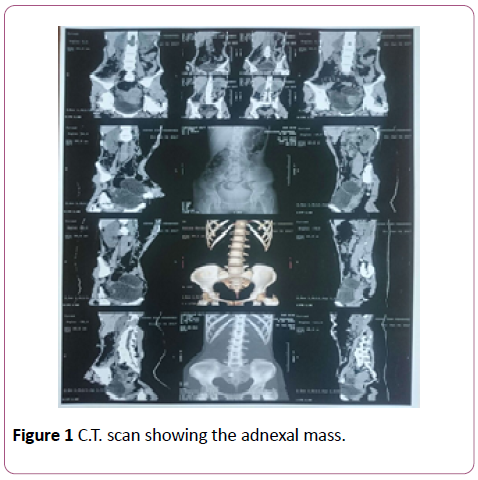
A seventeen years old girl presented to the emergency department of our hospital complaining of acute abdominal pain for 8 hours. On Examination her pulse was 120 beats per minute, blood pressure 100/60 and temperature was 37.8 Celsius, abdominal examination revealed lower abdominal tenderness and rebound tenderness. Laboratory investigations revealed leucocytosis. She was initially diagnosed as acute appendicitis and C.T. scan was arranged which revealed a large adnexal mass 82 × 63 mm (Figure 1).
So an urgent Doppler ultrasound was arranged, which showed absent blood flow to the adnexal mass. Based on the above findings laparoscopy with the possibility of laparotomy was decided and the patient was consented for that.
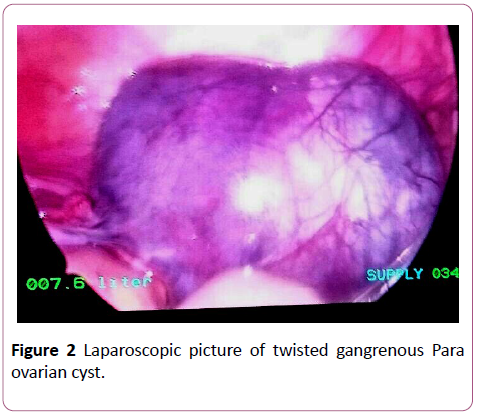
Laparoscopy was done through one umbilical 10 mm. incision and two side incisions 10 and 5 mm. in size. Laparoscopy revealed torsion and gangrene in the Para ovarian cyst (Figure 2).
The medial part of the right tube immediately next to the uterus was coagulated then cut by diathermy. The right infundibula-pelvic ligament was coagulated then cut by diathermy. The specimen was inserted in an endoscopic retrieval bag then the cyst punctured inside the bag to avoid intra-peritoneal spilling of the cyst contents and to decrease the size of the specimen to be able to extract it through the laparoscopy port, in addition to, aspiration of minimal amount of toxic fluid, which was present in the pelvis.
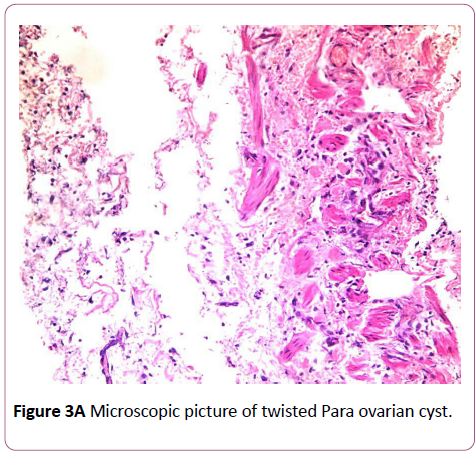
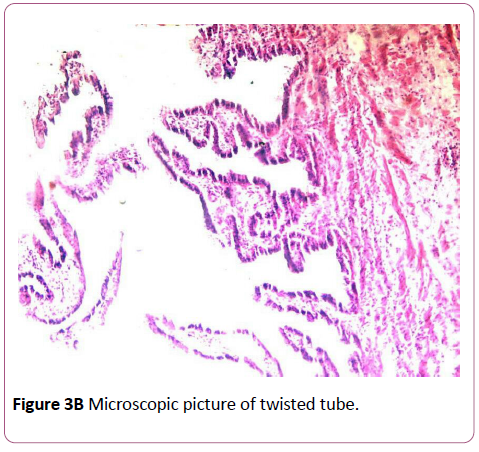
Postoperatively the girl made an uneventful recovery and was discharged after 2 days. Histo-pathological examination of the cyst revealed gangrenous simple serous Para ovarian cyst (Figure 3A) and gangrenous tube (Figure 3B).
Discussion
The current case represents a large complicated Para ovarian cyst managed by laparoscopy. Most of these cysts are accidentally discovered when they reach a large size or become complicated as with the current case.
Between 2.1 and 16% of Para ovarian cysts become complicated by Torsion [4], which presents clinically as abdominal and adnexal tenderness on pelvic examination, in addition to, a palpable mass with peritoneal signs which were all present in the current case; however, most of these findings are non-specific, and need to be differentiated from ruptured ovarian cyst, acute ureteric colic, pelvic inflammatory disease or acute appendicitis [5], the latter diagnosis was the initial diagnosis in the current case.
Grey scale and colour Doppler ultrasound have 99% specificity in diagnosing paraovarian cysts but only 14% sensitivity [6]. Ultrasonography can diagnose such cases by the “Split sign” which shows cyst dissociation from the ovary upon pushing the probe, thus, distinguishing them from ovarian masses [7]. Ultrasound features of tubal torsion include visualization of the twisted vascular pedicle and dilated tube with thick echogenic walls and internal debris/haemorrhage [8]. Colour Doppler is also helpful, which may show a high impedance waveform with reversal of diastolic flow in the affected tube [5]; however, definitive diagnosis is usually confirmed during laparoscopy or laparotomy [9].
Surgical management of torsion of Para ovarian cysts should be by de-torsion in early cases as ovarian function is usually preserved in 88% to 100% of cases [10]. Agarwal et al. [11], reported their experience in managing 46 cases of ovarian torsion and found that cases with benign pathology and ischemia are not a contraindication for ovarian preservation. In fact Dunckley et al. [12] reported successful decompression, de-torsion and excision of paraovarian cysts laparoscopically in two adolescent girls with preservation of the intact ipsi-lateral ovary; however, this was not possible in the current case as the both the tube and ovary were gangrenous; therefore, unilateral salpingo-oophorectomy was done, which does not appear to affect the prognosis in patients with germ cell tumours (the most common type in this age group) and tumours with low malignant potential; however, if histopathological examination had shown malignancy, which is not the case in this patient; she should have undergone complete surgical staging even if she chooses to preserve the uterus and remaining ovary [13].
ovary; however, this was not possible in the current case as the both the tube and ovary were gangrenous; therefore, unilateral salpingo-oophorectomy was done, which does not appear to affect the prognosis in patients with germ cell tumours (the most common type in this age group) and tumours with low malignant potential; however, if histopathological examination had shown malignancy, which is not the case in this patient; she should have undergone complete surgical staging even if she chooses to preserve the uterus and remaining ovary [13].
Conclusion
Laparoscopy is preferred over laparotomy in the management of torsion of paraovarian cysts as it is associated with shorter hospital stay and less patient discomfort.
De-torsion of the twisted paraovarian cyst should be done in early cases as ovarian function is usually preserved in 88% to 100% of cases, while salpingo-ophorectomy should be reserved to late gangrenous cases.
References
- Kiseli M, Caglar GS, Cengiz SD, Karadag D, Yilmaz MB (2012) "Clinical diagnosis and complications of paratubal cysts: Review of the literature and report of uncommon cases". Arch Gynecol Obstet 285: 1563-1569.
- Barloon TJ, Brown BP, Abu-Yousef MM, Warnock NG (1966) "Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginalsonography." J Clin Ultrasound 24: 117-122.
- Varras M, Akrivis C, Polyzos D, Frakala S, Samara C (2003) "A voluminous twisted paraovarian cyst in a 74-year-old patient: case report and review of the literature". Clin Exp Obstet Gynecol 30: 253-256.
- Genadry R, Parmley T, Woodrdruff JD (1977) The origin and clinical behavior of the paraovarian tumor. Arch Gynecol Obste 129: 873-880.
- Perlman S, Hertweck P, Fallat ME (2005) Paratubal and tubal abnormalities. SeminPedSurg 14: 124-134.
- Sokalska A, Timmerman D, Testa AC, Von Holsbeke C, Lissoni AA, et al. (2009) Diagnostic accuracy of transvaginal ultrasound examination for assigning a specific diagnosis to adnexal masses. Ultrasound ObstetGynecol 34: 462-470.
- Savelli L, Ghi T, De Iaco P, Ceccaroni M, Venturoli S, et al. (2006) Paraovarian/paratubal cysts: comparison of transvaginalsonographic and pathological findings to establish diagnostic criteria. Ultrasound Obstet Gynecol 28: 330-334.
- Dietrich JE, Heard MJ, Edwards C (2005) Uteroovarian ligament torsion due to a paratubal cyst. J Pediatr Adolesc Gynecol 18: 125-127.
- Suñer DB, Amorós EC, Ayala AU, Salais SF, Díaz-García C (2009) Torsion of a giant para-ovarian cyst. Conservative laparoscopic treatment. Gynecological Surgery6: 67-69.
- Oelsner G, Shashar D (2006) Adnexal torsion. Clin Obstet Gynecol 49: 459-463.
- Agarwal P, Agarwal P, Bagdi R, Balagopal S, Ramasundaram M, et al. (2014) Ovarian preservation in children for adenexal pathology, current trends in laparoscopic management and our experience. J Indian Assoc Pediatr Surg;19: 65-69.
- Dunckley MG, Wright N, Healy C, Mahomed AA (2014) Laparoscopic Management of Torted Paraovarian Cysts in Adolescent Girls. Videoscopy 24: 26-32.
- Graham L (2008) ACOG Releases Guidelines on Management of Adnexal Masses. Am Fam Physician 77: 1320-1323.
- Darwish AM, Amin AF, Mohammad SA (2003) Laparoscopic Management of Paratubal and Paraovarian Cysts. Journal of the society of Laparoendoscopic Surgeons 7: 101-106.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences