Knowledge, Attitude and Bioethical Dilemmas in Community and Hospital Pharmacy Practice in Port Harcourt, Nigeria.
Ifeoma Cynthia Ekenna1* and Lucky Legbosi Nwidu2
1Department of Pharmaceutics and Pharmaceutical Technology, University of Port Harcourt, Port Harcourt, Nigeria
2Department of Experimental Pharmacology and Toxicology, University of Port Harcourt, Port Harcourt, Nigeria
- *Corresponding Author:
- Ifeoma Cynthia Ekenna
Department of Pharmaceutics and Pharmaceutical Technology,
University of Port Harcourt, Port Harcourt,
Nigeria,
E-mail: ifeoma.ekenna@uniport.edu.ng
Received date: April 05, 2023, Manuscript No. IPPPE-23-16298; Editor assigned date: April 07, 2023, PreQC No. IPPPE-23-16298 (PQ); Reviewed date: April 18, 2023, QC No. IPPPE-23-16298; Revised date: April 28, 2023, Manuscript No. IPPPE-23-16298 (R); Published date: June 06, 2023, DOI: 10.36648/ipppe.6.1.068.
Citation: Ekenna IC, Nwidu LL (2023) Knowledge, Attitude and Bioethical Dilemmas in Community and Hospital Pharmacy Practice in Port Harcourt, Nigeria. J Pharma Prac Edu Vol.6 No.1: 068.
Abstract
Background: As a community, hospital, or clinical pharmacist, a pharmacist's job is to provide medication-related healthcare services. There have been more ethical challenges as pharmacy practice has shifted from being product-focused to patientoriented, however, the pharmacist must follow applicable laws or good pharmacy practices. Generally speaking, community and hospital pharmacists must constantly strike a balance between patient autonomy rights guaranteed by law and interventions meant to enhance patient outcomes. This study aims to investigate bioethical worries and ethical dilemmas among community and hospital pharmacists in Port Harcourt, Nigeria. Considering these moral conundrums will undoubtedly aid in addressing the difficulties pharmacists encounter in their line of work.
Methods: The data was gathered using a questionnaire. The participants were those who attended the Mandatory Continuous Professional Development (MCPD) training that was held in 2019 by the Pharmacists Council of Nigeria and the Faculty of Pharmaceutical Sciences, University of Port Harcourt. For inferential analysis, statistical techniques like Chi square analysis, cross tabulations and Cronbach’s reliability tests were applied. Modes, frequency and percentages were used for descriptive analysis.
Findings: Participants were made up of males and females (52.4% and 47.6% respectively, p>0.05) and the majority of them practiced community pharmacy (70.7%, p<0.05) and had B.Pharm degrees as highest level of education (69.5%, p<0.05). Most had between 11 years and 20 years of experience (38.46%, p<0.05). Even though they generally had a positive attitude toward bioethics and promoted good bioethical practices (93.02%, p<0.05), the study showed that they frequently encountered ethical issues in their practice (48.84%, p<0.05). Additionally, it was noted that community pharmacists deal with more ethical challenges than hospital pharmacists (p<0.05).
Conclusion: This study reveals the gaps in Port Harcourt's pharmacy practice, particularly with regard to bioethics in pharmacy practice and offers recommendations for how to make it healthier, especially for community and hospitalbased pharmacy practice.
Keywords
Bioethical dilemma; Ethical dilemma; Pharmacy practice; Community pharmacy; Hospital pharmacy; Pharmacist; Health care
Introduction
Pharmacists habitually provide integrated, accessible, accountable healthcare services in a variety of practice settings such as community and hospital and clinical [1,2], in dissimilar operational areas in different countries [3,4]. Pharmacy profession is practiced in three main areas of pharmacy practice: Community, clinical and hospital; though other practice areas abound. Every place (including community pharmacy) where medication is used for the prevention, diagnosis and treatment of any clinical condition, that is considered to be the interface of pharmacist and patient, should be recognized as the pharmacist's clinic [5].
Community pharmacists are the most accessible healthcare professionals [6,7], the third largest healthcare professional group in the world after physicians and nurses [8] with multifaceted pharmaceutical services and multidisciplinary responsibilities in a complex healthcare system. As pharmacy practice is transiting from product-oriented to patient-oriented health care services, the community pharmacists are inundated with myriads of roles. Community pharmacist diverse role includes medication reviews, minor/common ailment management, pharmacist prescribing for existing prescriptions, smoking cessation counseling and administration of injectable drugs and vaccinations [9], patientoriented medication counseling activities [10]; medication of veterinary patients [11]. Others may include emergency medication refills, renewals/extensions of prescriptions, changes to doses or formulations, therapeutic substitution, prescribing for minor ailments, initiation of prescription drug therapy, ordering and interpreting laboratory tests and administering drugs by injection [12]. Community pharmacists assess the appropriateness of prescriptions, educate patients about the medications and disease states prior to releasing the prescriptions, monitor the effectiveness and safety of prescription medications and encourage patients to engage in self-management with nonpharmacologic strategies. A systematic review of community pharmacist’s healthcare roles includes playing a major role in the health outcomes of patients by their interventions in medication adherence and quality use of medicines [13,14]. In public health, the community pharmacists evaluate the effectiveness, accessibility and the quality of personal and population-based health services [15,16]. They are capable of developing and sustaining partnership with patients and other providers with increased emphasis on collaborative and patient-centered care [1,4].
These responsibilities of community and hospital pharmacists revolves round pharmaceutical care, the main practice, in which the pharmacists are held accountable for drug therapy, achievement of optimal health outcome and maximizing quality of life of the patients [17]. The paradigm shift in roles of community pharmacist from product-oriented to patient-centered services is challenged by ethical issues [18]. Therefore the pharmacist is expected to adhere to national regulation or good pharmacy practice. This is the basis of ethical guidance in health governance [19]. Professional ethics are necessary as it is based on sound moral principle [20,21]. The dynamic force controlling ethical behavior for a pharmacist is professionalism [22,23]. Every health jurisdiction has its own code of ethics that guide the practice of pharmacy [24]. This protects the profession and individual from misconduct and offer standard for professional judgment against misconduct [25,26].
The patient-centered approach imposes a professional duty of care on the pharmacists to identify patients’ concerns and needs and collaborate closely with other health professionals to ensure effective and safe use of medicines to optimize the health of patients [27]. Pharmacists are compelled to be responsible for helping patients to achieve definite health outcomes [28]. How many health system pharmacists recognize that the health and wellbeing of the consumer of their services should be prioritized; that they should utilize the pharmaceutical knowledge to provide compassionate care in an appropriate and professional manner? That they should assist in ensuring that medicines are administered in the safest and most effective way possible?
However, because earnings are made from selling pharmaceuticals, the profession, particularly community pharmacy, sits at the crossroads of health and business in their professional relationship with their client. Moreover health professionals' authority to act in the best interests of society and the individual patient is challenged by economic and legal restraints, as well as demanding patients [29,30]. Besides, pharmacists are challenged with stringent regulations, financial pressure and increased competition [31]. At the same time, the demand for health services is growing as a result of population ageing, more chronic illnesses and increased healthcare consumerism [32,33]. This creates a slew of ethical issues, as well as a pressing need for decision-making rules based on moral commitments and virtues [34].
In either the community or hospital practice setting, pharmacists are frequently confronted with moral dilemmas [32,35,36] arising from conflicting personal, professional, institutional or societal values of the different parties involved [27,37,38]. An “ethical dilemma” is operationalized as a “situation in which there is a choice between at least two courses of action, neither of which is morally correct” [7,33]; in general, community and hospital pharmacists constantly face dilemmas in balancing the patients’ legal rights to autonomy against making interventions toward quality health outcomes [32].
Evaluating these moral dilemmas will no doubt help to address the challenges pharmacists face in their professional role [39-42]. There have been few international studies of the moral dilemmas experienced by community and hospital pharmacists and existing studies vary widely in aim, method and presentation of results [7,43,44]. Hospital pharmacists work in a hospital environment, represent a significant sector of practicing pharmacists and the hospital pharmacist can be defined by his/her competences and tasks. Hospital pharmacists and especially clinical pharmacists are in direct contact with medical doctors and their tasks concern mainly hospitalised patients. Differences between hospital and community pharmacists are to be expected in several areas of practice such as patient care and pharmaceutical technology. Community pharmacists are in direct contact with patients and are councillors of ambulatory patients; treatment is frequently symptomatic, based on prescriptions and discussions with the patient and concerns chronic illness. “The overarching goal of hospital pharmacists is to optimize patient outcomes through the judicious, safe, efficacious, appropriate and cost effective use of medicines” and “the ‘five rights’ (the right patient, right medicine, right dose, right route and right time)” [45]. Hospital pharmacist roles include participating in medication management, which encompasses the entire way in which medicines are selected, procured, delivered, prescribed, administered and monitored [46,47].
Community pharmacy unlike hospital pharmacy practice varies in different countries; it is frequently confronted with diverse complex ethical dilemmas which challenge ethical pharmacy governance. The commodification of medicines has led to community pharmacy encountering lots of conflicts.
Considering the enormous transition in practice and the challenges pharmaceutical services delivery in a milieu of ever burgeoning pharmacist’s responsibilities, ethical conflicts from moral dilemmas are bound to abound. In Nigeria, most especially in Port Harcourt, Rivers state, Nigeria no reports to our knowledge exist evaluating bioethical issues confronting pharmacists. Therefore the aim of this study is to investigate bioethical issues and ethical dilemmas among community and hospital pharmacists practicing in Port Harcourt, Nigeria.
Materials and Methods
Study setting, design and period
Qualified registered practicing pharmacists, comprising of community pharmacist and hospital pharmacist attending Mandatory Continuous Professional Development (MCPD) training organized by the Faculty of Pharmaceutical Sciences, University of Port Harcourt in conjunction with the Pharmacists Council of Nigeria at the University of Port Harcourt Teaching Hospital in January 2019 were recruited for the study.
Inclusion and exclusion criteria
Only pharmacists that gave their consent and are practicing in community pharmacy or in the hospital pharmacy were included in the study. The academic and industrial pharmacists that participated in the 2019 MCPD programme in the University of Port Harcourt were excluded because the ethical issues they face in practice is different from that covered in this study.
Sampling
The questioner was distributed to all the MCPD 2019 participants that worked either in the community pharmacy or hospital pharmacy without sampling. Only the correctly filled questionners were used for the analysis.
Data collection procedure
A qualitative research method was used with the aid of structured closed end, multiple choice questionnaires that were used to interview the subjects. The participants were pharmacists practicing in community and hospital pharmacy in Port Harcourt, Rivers State, Nigeria. The population size was 86. The work places of some of the participants were visited who were unable to submit the filled questionnaire at the venue of MCPD in order to retrieve the filled questionnaire.
The questionnaire was divided into 3 sections-A,B,C which contained questions to demonstrate the demography of the study population, attitude of the pharmacists and the frequency of occurrence of bioethical dilemmas in their practices respectively. Section A was made up of 5 questions and asked questions on the gender, area of practice, highest educational status and years of practice. Section B consisted of 11 questions in a table using the dichotomous response of ‘yes’ and ‘no’ demonstrating the attitude of the participants to bioethics. Section C consisted of 10 questions in a table using 7 point-Likert scale as the responses, the response options includes: ‘I don’t know/not available’, ‘never’, ‘hardly ever’, ‘every few months’, ‘once or twice a month’, ‘’once or twice a week’ and ‘ at least once a day’.
Variables of the study
The demographic factors-gender, area of practice, highest educational qualification and years of practice were the independent varibles while attitude and the frequency of occurrence of bioethical issues were the dependent variables.
Reliability testing
Ms-excel LTSC 2019 was used for data entry. The SPSS version 23 was the statistical software utilized in the analyses of the responses. The mode, frequency and percentage of frequencies were all computed. Cross tabulations and chi-square (ê?2) analyses were used to analyse the responses from the questionnaire where a p-value less than <0.05 was considered significant. Pie charts and bar charts were utilized to show frequency.
Results
The result presented here are from 2 areas of practice only-the community pharmacy practice and the hospital pharmacy practice. Areas of practice not covered include-academia and industrial pharmacy practice. Results are presented as the demography of the participants, their attitude towards bioethics in pharmacy practice and the frequency of occurrence of the Bioethical Dilemma (BD)/issues during their practices. Cross tabulation and Chi-square analyses were used to test if the attitude to bioethical issues were dependent on the demographical factors. Also, using the Chi square test, this study further determined if there was a significant difference in the occurrence of bioethical dillemas in the two (2) areas of pharmacy practice (community and hospital) (Table 1).
| Variable | Frequency (%) | ê?2 | P-value | |
|---|---|---|---|---|
| Gender | Male | Female | ||
| N=84 | 44 (52.4) | 40 (47.6) | 0.19 | 0.663 |
| Area of practice | Community practice | Hospital practice | ||
| N=82 | 58 (70.7) | 24 (27.9) | 14.1 | <0.0001 |
Table 1: Demographics showing the gender and the area of practice of the participants.
Demographics
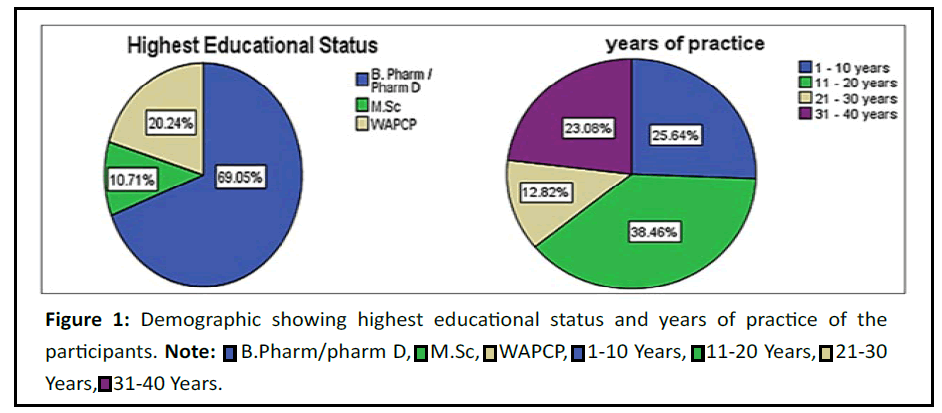
The participants were 86 in number. The participants constitute 52.4% males and 47.6% females. The population of the different gender was not significantly different (ê?2= 0.19, p>0.05) but their area of practice which had the community practice (70.7%) having a significant proportion of the population than the hospital practice (27.9%) (ê?2=14.1, p<0.05). This is because within the vicinity of Rivers State, Nigeria, there are more community pharmacy utlets than hospital pharmacies. Most of the participants had B.Pharm/Pharm. D as their highest qualification (69.05%) (ê?2=49.36, p<0.05) and most had 11 years-20 years of pharmacy practice (38.46%) (ê?2=10.41, p<0.05) (Figure 1).
Attitude
Section B has questions 1-12 in the questionnaire which evaluated the attitude of the participants to issues concerning bioethical research. To accertain the attitude, respondents were asked if they had knowledge of ethical dilemma, if they were willing to report and document on ethical dilemma, if they were willing to fund and collaborate on research pertaining to bioethics etc. Table 2 shows the questions and the responses, with answers with the highest frequency italicised. The p-values are provided to denote the significant differences between participants who answered yes and no to the various questions.
| Yes | No | ê?2 | P-value (Chi-square test) | |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Knowledge of Bioethics bordering on ethical dilemma? N=85 | 36 (42.4) | 49 (57.6) | 1.988 | 0.159 |
| Interest to willingly document information on ethical dilemma' N=84 | 82 (97.6) | 2 (2.4) | 76.19 | <0.0001 |
| Interest to willingly report information on ethical dilemma' N=84 | 84 (100) | 0 (0) | - | - |
| Willingly available to participate in research collaboration on bioethics' N=82 | 77 (93.9) | 5 (6.1) | 63.22 | <0.0001 |
| Interest to co-author scientific publication on bioethics' N=79 | 65 (81.3) | 15 (18.8) | 31.25 | <0.0001 |
| Readily available to fund bioethics research' N=76 | 42 (55.3) | 34 (44.7) | 0.842 | 0.359 |
| Willingly interested to be mentored on bioethics research' N=81 | 72(88.9) | 9 (11.1) | 49 | <0.0001 |
| Willing to be a vanguard of bioethical interest group' N=81 | 70 (86.4) | 11 (13.6) | 42.975 | <0.0001 |
| Willing to be a whistle blower in bioethical issues in my environment' N=80 | 71 (88.8) | 9 (11.3) | 48.05 | <0.0001 |
| Willing to collaborate with other health professionals on bioethics' N=84 | 82 (97.6) | 2 (2.4) | 76.19 | <0.0001 |
| Willing to discuss with policy makers on bioethical issues affecting health institutions' N=83 | 29 (36.3) | 51 (63.7) | 67.771 | <0.0001 |
| Any bioethics unit for reporting ethical issues in your environment' N=80 | 29 (36.3) | 51 (63.7) | 6.05 | 0.014 |
| Note: p<0.05 is considered significant. Figures written in italics show the higher values. N= number of participants that answered each question. | ||||
Table 2: Attitude.
According to Table 2, the majority of participants (57.6%) had no knowledge of bioethics bordering on ethical dilemma, though this was not a significant difference (ê?2=1.988, p>0.05) when compared to people with bioethical knowledge (42.4%). This may impart due to large number of respondents (63.7%) who reported that there was no bioethics unit for reporting ethical issues in their environment.
Reliability test
The Cronbach’s alpha reliability test was used as a test of reliability to determine if the questions the participants were asked in section B could be a true test of the attitude of the pharmacists to bioethical issues. A score of 0.720 was obtained (Table 3) indicating significant reliability. Eleven (11) out of the twelve (12) questions asked were reliable; the question “where to report bioethics issues” was omitted because it does not reflect attitude of the participants.
| Cronbach's alpha | N of items |
|---|---|
| 0.72 | 11 |
Table 3: Reliability statistics for attitude to bioethical issues.
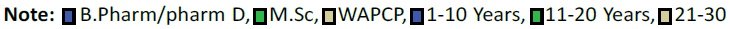
The participants’ responses to the questionnaire were converted to a continuous variable to determine the general attitude of the participants. The conversion indicate that the participant generally had a positive attitude (ê?2=94.698, p<0.05) to the promotion of bioethics as shown in Figure 2. In this study, the answer of yes is regarded positive response and the answer of no is regarded as negative response.
Frequency of occurrence of Bioethical Dilemma (BD)
Section C, questions 1-10 of the questionnaire dealt with the incidence of bioethical events relating to ethical dilemma. Scenerios were created bordering on ethical dilemmas suggesting to the participants how frequently they experienced such bioethical scenerios. The questions and the responses are shown in Table 4, the highest frequency for each answer is written in italics. The result indicate that the frequency of events bordering on Bioethical Dilemma (BD) in both areas of pharmacy practice were significantly high (mostly p<0.05). The responses in the questionnaire were summarized as answers such as; “Not Applicable (NA)” to “at least once a day” to reflect the frequency of events relating to bioethical dilemmas. These show how frequent such events happen.
| Questions | NA/I don’t know | Never | Hardly ever | Every few months | Once or twice a month | Once or twice a week | At least once a day | ê?2, (p-value) |
|---|---|---|---|---|---|---|---|---|
| You are presented with an unsigned prescription for drug mostly written on ordinary plain sheet of paper' N=82 | 0 (0) | 3 (3.7) | 7 (8.5) | 8 (9.8) | 14 (17.1) | 24 (29.3) | 26 (31.7) | 32.878 (<0.0001) |
| A customer demands an opioid antitussive or opioid analgesic without prescription (abuse of drug) N=80 | 1 (1.3) | 12 (15.0) | 9 (11.3) | 4 (5.0) | 12 (15.0) | 29 (36.3) | 13 (16.3) | 42.15 (<0.0001) |
| You are asked to supply emergency hormonal contraceptive over the counter N=81 | 1 (1.2) | 20 (24.7) | 5 (6.2) | 5 (6.2) | 5 (6.2) | 18 (22.2) | 27 (33.3) | 51.136 (<0.0001) |
| A patient hands you a prescription but you could not receive further clarification from the prescriber even though ideally you should N=82 | 0 (0) | 6 (7.3) | 13 (15.9) | 13 (15.9) | 21 (25.6) | 14 (17.1) | 15 (18.3) | 8.439 (0.134) |
| A customer asked for an over-the-counter treatment even though the treatment isn’t really needed but the treatment would cause no harm N=81 | 1 (1.2) | 6 (7.4) | 8 (9.9) | 12 (14.8) | 24 (29.6) | 18 (22.2) | 12 (14.8) | 30.395 (<0.0001) |
| A patient returns unused, unopened, in date medication for disposal one day after it has been dispensed N=82 | 0 (0) | 11 (13.4) | 22 (26.8) | 16 (19.5) | 20 (24.4) | 11 (13.4) | 2 (2.4) | 19.415 (0.002) |
| The prescription states a specific brand of drug. You do not have this in stock but you have the generic equivalent brand N=81 | 0 (0) | 1 (1.2) | 1 (1.2) | 6 (7.4) | 9 (11.1) | 22 (27.2) | 42 (51.9) | 94.333 (<0.0001) |
| Patient comes in to purchase his/her medicine for treatment but using an old prescription N=82 | 1 (1.2) | 2 (2.4) | 8 (9.8) | 20 (24.4) | 26 (31.7) | 20 (24.4) | 5 (6.1) | 52.024 (<0.0001) |
| After questioning a patient, she/he reveals she/he is going to use the medication she us asking to buy against guidelines e.g., hydrocortisone cream for the face N=82 | 0 (0) | 9 (11.0) | 19 (23.2) | 11 (13.4) | 21 (25.6) | 14 (17.1) | 8 (9.8) | 10.488 (0.063) |
| A customer asks to buy an over-the-counter medicine you suspect she/he might be abusing. The customer does not want an alternative N=82 | 1 (1.2) | 10 (12.2) | 12 (14.6) | 14 (17.1) | 16 (19.5) | 21 (25.6) | 8 (9.8) | 20.61 (0.002) |
| Note: Values highlighted in italics show highest values. | ||||||||
Table 4: Frequency of occurrence of events bordering on bioethical dilemma.
Reliability test
The Cronbach’s alpha reliability test was used as a test of reliability to determine if the questions the particpants’ were asked in section C could be a true test of the frequency of occurrence of Bioethical Dilemma (BD), A score of 0.834 was obtained (Table 5) indicating significant reliability. The ten (10) questions asked in section C were relevant.
| Cronbach's alpha | N of items |
|---|---|
| 0.834 | 10 |
Table 5: Reliability statistics for frequency of occurrence of bioethical dilemma.
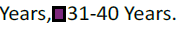
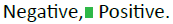
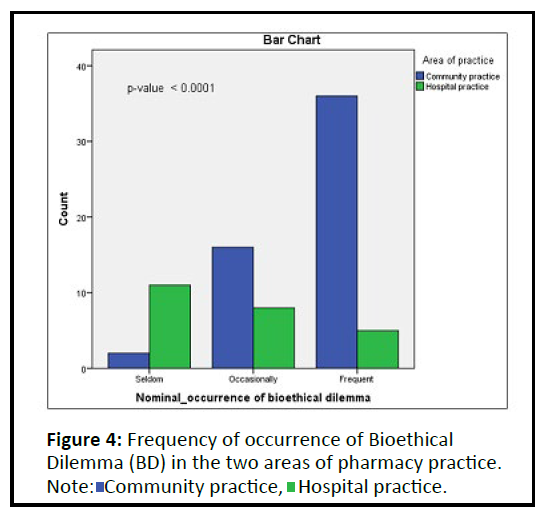
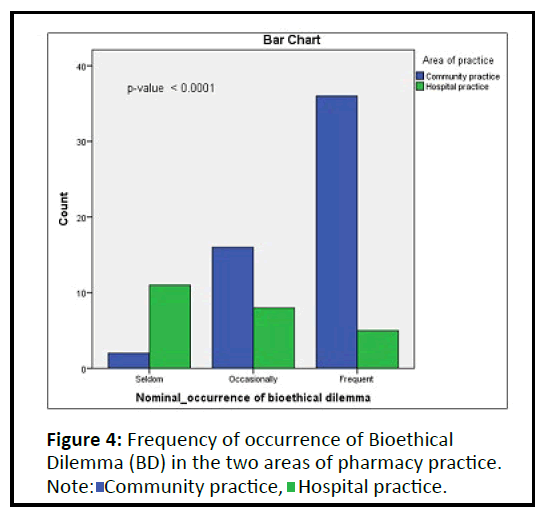
The participants’ responses in section C was converted to a continuous variable to determine the frequency of occurrence of Bioethical Dilemma (BD) in the 2 different areas of practice (hospital and community). The conversion indicated that the participants had frequent occurrences of BDs in their practices (48.84%) (Figure 3). The differences in answers were significant, (ê?2=14.439, p<0.05). A 7 point Likert scale was used to provide 7 responses as options for them to choose from; the responses were further classified to three (3) groups: “Frequent bioethical dilemma”, “occasional bioethical dilemma” and “seldom bioethical dilemma”.
Peasrson correlation was used to examine whether there was any correlation between the continuous variables, the attitude of particpants to bioethics and the occurence of events contiguous on ethical dilemma. Also Spearman’s correlation was used to evaluate if there was any correlation between the nominal variables of the attitude of participants’ and the frequencies of occurrence of Bioethical Dilemma (BD). The results are displayed on Table 6. The result reveal that there is no correlation existing between the attitude of participants’ and the frequencies of occurrence of bioethical dilemma (p>0.05, correlation <0.01). This indicates that the pharmacist positive attitude to propagating/ promoting bioethics does not affect the frequency of occurrence of BD in their practices. However, the scope of this study does not state how the participants handle bioethical dilemmas. For example, it does not state what the pharmacist does when confronted with BD such as when presented with an unsigned drug prescription, worse still, written on an ordinary sheet of paper.
| Occurrence_scale | Occurrence_nominal | ||
|---|---|---|---|
| Attitude_scale | Pearson correlation | -0.071 | |
| Sig. (2-tailed) | 0.524 | ||
| N | 82 | ||
| Attitude_nominal | Spearman’s rho | -0.059 | |
| Sig. (2-tailed) | 0.596 | ||
| N | 82 | ||
| Note: N=Population size, sig.=p-value | |||
Table 6: Pearson and Spearman’s correlations of attitude of the participants and the occurrence of bioethical dilemma in the two areas of practice.
Peasrson correlation was used to examine whether there was any correlation between the continuous variables, the attitude of particpants to bioethcs and the occurence of events contiguous on ethical dilemma. Also Spearman’s correlation was used to evaluate if there was any correlation between the nominal variables of the attitude of paticipants and the frequencies of occurrence of Bioethical Dilemma (BD). The results are displayed on Table 6. The result reveal that there is no correlation existing between the attitude of paticipants and the frequencies of occurrence of bioethical dilemma (p>0.05, correlation <0.01). This indicates that the pharmacist positive attitude to propagating/promoting bioethics does not affect the frequency of occurrence of BD in their practices. However, the scope of this study does not state how the participants handle bioethical dilemmas. For example, it does not state what the pharmacist does when confronted with BD such as when presented with an unsigned drug prescription, worse still, written on an ordinary sheet of paper.
Cross tabulations
Results shown in Table 7 indicate that gender, years of practice, highest educational qualification and area of practice did not influence the attitude of the participants to bioethical issues, p>0.05.
| Positive attitude% | Negative attitude% | ê?2 | p-value | ||
|---|---|---|---|---|---|
| Years of practice | 1-10 years | 25.641 | 0 | 1.988 | 0.575 |
| 11-20 years | 37.1795 | 1.2821 | |||
| 21-30 years | 11.5385 | 1.2821 | |||
| 31-40 years | 21.7949 | 1.2821 | |||
| Gender | Male | 48.8095 | 3.5714 | 2.828 | 0.093 |
| Female | 47.6191 | 0 | |||
| Area of practice | Community practice | 67.0732 | 3.6585 | 1.289 | 0.256 |
| Hospital practice | 29.2683 | 0 | |||
| Highest educational Status | B. Pharm/Pharm D | 66.6667 | 2.381 | 2.118 | 0.347 |
| M.Sc | 9.5238 | 1.1905 | |||
| PhD | 0 | 0 | |||
| WAPCP | 20.2381 | 0 |
Table 7: Cross tabulations of attitude vs demographic factors.
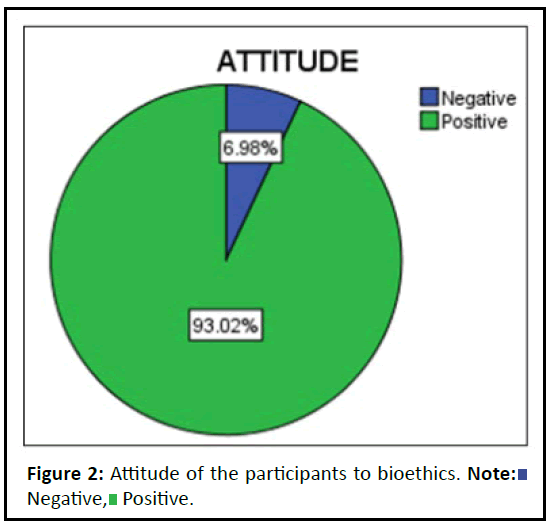
Table 8 shows that there is a significant difference in the frequency of occurrence of bioethical dilemma in the different areas of practice (community and hospital) (in most cases p<0.05). The result revealed that the community practice experiences more issues bordering on bioethical dilemmas than the hospital practice in River State, Nigeria. Figure 4 collaborates the result obtained in Table 8. Figure 4 indicates that the occurrence of BD is seldom in the hospital pharmacy practice and more frequent in the community pharmacy practice (ê?2 = 25.409, p<0.0001).
| Questions | Never | Hardly ever | Every few months | Once or twice a month | Once or twice a week | At least once a day | ê?2 (p-value) | |
|---|---|---|---|---|---|---|---|---|
| 1. You are presented with an unsigned prescription for drug mostly written on ordinary plain sheet of paper | Community practice | 67% | 43% | 71% | 77% | 61% | 80% | 4.79 (0.44) |
| Hospital practice | 33% | 57% | 29% | 23% | 39% | 20% | ||
| 2. A customer demands an opioid antitussive or opioid analgesic without prescription (abuse of drug) | Community practice | 0% | 22% | 100% | 100% | 86% | 92% | 48.7 |
| Hospital practice | 100% | 78% | 0% | 0% | 14% | 8% | (<0.0001) | |
| 3. You are asked to supply emergency hormonal contraceptive over the counter | Community practice | 21% | 60% | 75% | 100% | 88% | 92% | 35.4 |
| Hospital practice | 79% | 40% | 25% | 0% | 12% | 8% | (<0.0001) | |
| 4. A patient hands you a prescription but you could not receive further clarification from the prescriber even though ideally you should | Community practice | 45% | 69% | 85% | 64% | 80% | 69% | 8.24 |
| Hospital practice | 55% | 31% | 15% | 36% | 20% | 31% | -0.1 | |
| 5. A customer asked for an over-the-counter treatment even though the treatment isn’t really needed but the treatment would cause no harm | Community practice | 0% | 38% | 64% | 83% | 82% | 92% | 24 |
| Hospital practice | 100% | 63% | 36% | 17% | 18% | 8% | -0 | |
| 6. A patient returns unused, unopened, in date medication for disposal one day after it has been dispensed | Community practice | 60% | 77% | 73% | 74% | 50% | 50% | 3.45 |
| Hospital practice | 40% | 23% | 27% | 26% | 50% | 50% | -0.6 | |
| 7. The prescription states a specific brand of drug. You do not have this in stock but you have the generic equivalent brand | Community practice | 100% | 80% | 75% | 82% | 61% | 69% | 6.04 |
| Hospital practice | 0% | 20% | 25% | 18% | 39% | 31% | -0.3 | |
| 8. Patient comes in to purchase his/her medicine for treatment but using an old prescription. | Community practice | 100% | 71% | 70% | 79% | 50% | 80% | 5.77 |
| Hospital practice | 0% | 29% | 30% | 21% | 50% | 20% | -0.5 | |
| 9. After questioning a patient, s/he reveals s/he is going to use the medication she is asking to buy against guidelines e.g., hydrocortisone cream for the face. | Community practice | 44% | 80% | 80% | 93% | 88% | 69% | 19.1 |
| Hospital practice | 56% | 20% | 20% | 7% | 13% | 31% | -0 | |
| 10. A customer asks to buy an over-the-counter medicine you suspect s/he might be abusing. The customer does not want an alternative. | Community practice | 11% | 58% | 62% | 93% | 86% | 88% | 25.2 |
| Hospital practice | 89% | 42% | 38% | 7% | 14% | 13% | (<0.0001) | |
| Note: Comparison is made between the areas of pharmacy practice. | ||||||||
Table 8: Cross tabulation between area of practice and occurrence of ethical dillemas.
Discussion
Community pharmacists are confronted with numerous bioethical issues in work environment and are in ethical dilemmas to decide in complex situation [48]. This is complicated with inadequate knowledge in handling ethical dilemmas in their daily activities. It is recently reported that moral dilemmas arose during professional contacts, more frequently when professional autonomy is challenged by the behavior of patients and other healthcare professionals [32]. Most of the time the pharmacists are in dilemma whether to dispense a generic drug or a wellknown branded drug. Al-Qudah; Tuza, [24] reported all kind of conflicts, pharmacists encounter in a number of ways in their practice settings including: When deciding whether or not to sell over-the-counter treatments that are not needed; when deciding whether or not to recommend less expensive generic medications; or when deciding whether or not to report a colleague that they feel has acted unethically.
The socio-demographic characteristics reveal that the ratio of male to female respondents who took part in the study was not significant but the number of community to hospital pharmacist that participated was very significant (ê?2=14.1; 0.0001) as shown in Table 1 community pharmacies are primary healthcare outlets performing numerous healthcare functions and they are quite commonplace than hospital pharmacies who are performing secondary healthcare functions. The educational qualifications of the respondents were B.Pharm/Pharm. D as their highest qualification (69.05%) (ê?2=49.36, p<0.05) and with practice experience averaging 11 years-20 years (38.46%) (ê?2=10.41, p<0.05), as reveal in Figure 1.
According to our findings, practicing pharmacists do not have a sufficient understanding of bioethics. This is evidenced by the increased percentage of participants who responded “no” to the question of knowing about bioethics and ethical dilemmas. The investigation revealed that, the level of knowledge of respondents on bioethical issues is 42.4% (Table 2). This is quite below 82.0% [49] and 72.3% [7] reported in similar study in Ethiopia and central Saudi Arabia respectively. The low level of knowledge on bioethical issues may be as a result of dearth of exposure to courses of ethics at the undergraduate level. Pharmacy ethics has traditionally occupied a minor role in pharmaceutical education, limited to a formal discussion and distribution of copies of the code of ethics to new pharmacists prior to their induction [50]. This has caused pharmacists in Nigeria to frequently struggle to define ethical issues and also lack ethical analytical skills as evidenced by their answer to “knowledge of bioethics” in this study. In his report, Okoro, [51] showed that the pharmacy ethics content of the Nigerian pharmacy education curriculum is woefully inadequate and the teaching technique is far too didactic to appropriately train future pharmacists for more challenging patient-centred roles in an ethically complex practice environment. This abysmal lack of knowledge is compounded with the level of education, as 69% of the respondents possess B.Pharm as their highest qualification which might affect professional practicing knowledge on ethical issues.
Interestingly, the study revealed positive attitudes of community and hospital pharmacists in Port Harcourt towards bioethical issues. For example, the willingness of respondents to document ethical dilemmas (97.6%); willingness to report breaches of ethical dilemmas (84%); willingness to collaborate on research on ethical dilemmas (93.9%); interest to co-author scientific publications on ethical dilemmas (81.3%) and willingness to fund bioethics research (45%) and so on (Figure 2). Moreover, interest of respondents on being mentored on bioethics research was significantly high (89%; P<0.0001); willingness to be vanguards of bioethics interest group (86%, P<0.0001), willingness to become bioethics whistle blowers (88%, P<0.0001) and willingness on collaborate with other healthcare professional on bioethics (97%, P<0.0001). Besides, the readiness to engage policy makers on issues relating to bioethics by respondents was very significant (64%; P<0.0001). The attitudes of respondents in the promotion of bioethics evaluated on Cronbach’s alpha reliability test yielded a score of 0.720 conoting high reliability of the questions used to evaluate respondents attitude in this study (Table 3). In addition, on converting responses of respondents in the questionnaire to continuous variables to evaluate general attitude, it was observed that the participants generally had a positive bioethics attitude (ê?2=94.698, p<0.05) to the promotion of bioethics (Figure 2). Our study revealed that pharmacists have a very positive attitude toward promoting bioethics in pharmacy practice, despite the fact that most of them have limited knowledge of bioethics in pharmacy practice and most of them attested to not knowing of any bioethics unit for reporting ethical issues in their environments. The attitude of the participants to bioethics is not influenced by their gender, year of practice etc. but it seems to be embedded in the culture of pharmacy practice, notwithstanding the area of practice of the pharmacists. This demonstrates some fundamental obstacles in positive ethical behaviour from practicing pharmacists in Rivers State, Nigeria, as one cannot positively practice what one does not understand and how can they properly record and document bioethical situations if there is no known bioethics unit available?
Evaluating the frequency of occurrence of bioethical dilemma in professional pharmacy practice in Port Harcourt, different scenarios of likely quandary situations were simulated representing incidences of probable bioethical issues confronting community and hospital pharmacy settings (Table 4). The result showed that frequency of occurrence of simulated quandary scenario was significantly high (mostly p<0.05). Scenario one: The respondents were asked if they received prescription of drugs on unsigned piece of paper, denoting dilemma of dispensing or not dispensing an illegal prescription; the frequencies ranged from at least once daily (32%), once or twice a week (29%); once or twice a month (17%) (ê?2=32.88, p<0.05). Scenario two: Respondents were asked if they had dilemmas of patients requesting an opioid antitussive or opioid analgesic without a prescription. The frequencies of occurrence are: At least once daily (16%), once or twice a week (36%); once or twice a month (15%) (ê?2=42.15; p<0.0001). Scenarios three: Respondents were asked if they ever face dilemmas of supplying emergency hormonal contraceptive over the counter. The rate of occurrences of this dilemma varies from at least once daily (33.3%), once or twice a week (22.2%); once or twice a month (6.2%) (ê?2=51.1; p<0.0001). Scenarios four: The community and hospital pharmacists were questioned if they have ever had quandaries of receiving prescriptions requiring further clarification from the prescriber but could not contact him/her? The frequencies of dilemmas occurring varies from at least once daily (18%), once or twice a week (17%); once or twice a month (26%) (ê?2=8.44; P<0.134). Scenarios five: Respondents were asked if they have dilemmas of patients demanding over the counter treatment that were not really needed and if administered will cause no harm to the patients? The frequencies of dilemmas situation occurring varies from at least once daily (16%), once or twice a week (36%); once or twice a month (15%) (ê?2=30.4; p<0.0001). Scenarios six: Pharmacists were asked, if they have ever been confronted with the quandary of patients returning dispensed, unused, in date purchased drugs the next day to the pharmacy? The frequencies of responses to this dilemma varies from at least once daily (2.4%), once or twice a week (13.4%); once or twice a month (24.4%) (ê?2=19.4; p<0.002).
Scenarios seven: Respondent were interviewed if they have been confronted with quandary situation in which prescription of a branded drug was presented that was out of stock but there is a generic equivalent drug available for dispensing? The frequencies of occurrence of this dilemmas situation varies from at least once daily (51.9%), once or twice a week (27.2%); once or twice a month (11.1%) (ê?2=94.3; p<0.0001). Scenario eight: Whether respondents are ever faced with dilemmas of a patient coming to refill their prescription with an old out dated prescription? The frequencies of reports of this dilemmas situation varies from at least once daily (31.7%), once or twice a week (24.4%); once or twice a month (6.1%) (ê?2=52.0; p<0.0001). Scenarios nine: Respondents were questioned if they were ever confronted with the dilemmas of after rigorously questioning the patient; they have awareness that patients are going to use drugs they are purchasing against guidelines? The frequencies of his dilemma occurred varies from at least once daily (25.6%), once or twice a week (17.1%); once or twice a month (9.8%) (ê?2=10.49; p<0.063). Scenarios ten: Pharmacists were asked if they had quandaries of customers requesting for drugs suspected to be likely abused? The frequencies of the responses ranged from at least once daily (19.5%), once or twice a week (25.6%); once or twice a month (9.8%) (ê?2=20.61; p<0.002).
The above scenarios revealed that the dilemmas pharmacists encounter while providing care in a complex setting are with economic and legal constraints. Pharmacists are expected to assist patients to optimise their health outcome and this responsibility requires pharmaceutical care relationship with patients. In consideration of patients wellbeing and mutual trust existing between pharmacist and patients, pharmacists are often confronted with quandaries. Besides, the behaviours of patients are unpredictable and restrain the pharmacist from acting autonomously, hence the frequent exposures of pharmarmacist to bioethical situations during their professional contacts [32,52,53].
Testing with Cronbach’s alpha reliability test whether the questions posited to the respondents in the various dilemmas scenarios above are reliable, whether they reflect the true test of the frequencies of occurrence, the Cronbach’s alpha reliability test score of 0.834 was obtained indicating significant reliability (Table 5). On frequency of occurrence of ethical dilemmas in community pharmacies, it was reported by another investigator to occur at least once per week [35].
Besides, converting the participants’ responses to the various questions in the various dilemmas situations on the 7-point Likert scale to a continuous variable in three domains (Figure 3): Frequent [at least once a day and once or twice a week], occasional [once or twice a month and every few months] and seldom [Hardly ever, Never and not available/I don’t know) bioethical dilemmas; the results reveal revealed significant differences in response, frequent (48.84%); occasional (30.2%) and seldom (16.3%) (ê?2=14.439, p<0.05).
Deploying Pearson correlation test to explore probable correlation between the two continuous variables, the attitude of participants’ to bioethics and the frequency of occurrence of events contiguous on ethical dilemma, the results reveal (Table 6) no correlation (p>0.05, correlation <0.01). Also no correlation was observed while utilising Spearman’s correlation test to evaluate if there was any correlation between the nominal variables of the attitude of participants and the frequencies of occurrence of Bioethical Dilemma (BD). This indicates that the pharmacist positive attitude to propagating/promoting bioethics does not affect the frequency of occurrence of BD in their practices.
To summarize the pharmacist’s responses into three domains (frequent, occasional and seldom), the participants’ responses provided on a 7-point Likert scale was converted to a continuous variable (Figure 4), in the two different areas of practice, hospital and community. The responses in the three domains: Frequent (at least once a day and once or twice a week), occasional (once or twice a month and every few months) and seldom (Hardly ever, Never and not available/I don’t know). The results reveal significant occurrence of BD in Community Pharmacies (CP) than Hospital Pharmacies (HP).
To evaluate the scenarios of BD that were significant, cross tabulation analysis (Table 8) was executed between the areas of practice and scenarios of BD, the results reveal scenarios two, three, five, nine and ten were significant for CP practice only but not for HP practice. For example in scenario two in which respondents were asked if they had dilemmas of patients requesting an opioid antitussive or opioid analgesic without a prescription; cross tabulating this BD between HP and CP practice areas reveal that this BD occur significantly more in CP than in HP practice (ê?2=48.66; p<0.0001). Similarly, in scenario three in which respondents were asked if they ever faced dilemmas of supplying emergency hormonal contraceptive over the counter. Cross tabulating this BD between the areas of practice, reveal CP practice was significant compared to HP practice (ê?2=35.38; p<0.0001). Moreover, cross tabulating dilemmas in scenario five, of patients demanding over the counter treatment that were not really needed and if administered will cause no harm to the patients, to the two practice areas demonstrate CP practice was significant than HP practice (ê?2=23.95; p<0.001). Worst still, in scenario nine in which the response to “if they have ever confronted with the dilemma of, upon rigorous questioning, awareness of patients are going to use drugs they are purchasing against guidelines”. Cross tabulation of this BD against the areas of practice indicate significant engagement in CP than HP practice (ê?2=19.09; p<0.002). Finally in scenario ten in which respondents were asked if they encountered quandary of patients requesting for drugs suspected to be likely abused, the cross tabulation of this dilemma and two areas of practice, reveal significant occurrence in CP than HP practice (ê?2=25.15; p<0.001).
Similar result was obtained in London by Deans, et al. [54]. These BD scenarios were not significant in HP practice due to structured and often dogmatic pharmacy practice in the hospital than in the community. Moreover, in the hospital, each practitioner is strictly restricted to their areas of practice with dogmatic watch to prevent any encroachment which is not possible in community pharmacy practice. In other words, pharmacists will be restricted to dispensing of prescribed drugs on prescription from a medic unlike in the community pharmacy practice where the pharmacist is not under keen straight-jacketed interprofessional watch and restriction. Furthermore, the immediate presence of medical physicians in hospitals assures that all drug dispensing regulations are followed appropriately, if not religiously, between the prescribing and the dispensing of such medication. These bioethical difficulties in pharmacy practice are exacerbated by the supermarket model of consumerism that operates within community pharmacies. The consumerist model assumes an informed and self-directed client (patient) is capable of identifying and describing individual desires (including medications) as service options [30]. This can be seen too in the UK where the UK National Health Service has educated the patients to recognize themselves as customers [55]. Hibbert, et al. [29] in their discussion of pharmacy consumers' approaches to the purchase of medicines, they recognized and elaborated on a similar phenomenon, which they summarised as 'permissive' and 'challenging' consumer voices. Challenging customers are wary of being questioned; believing that their prior experience had provided them with sufficient understanding and their emphasis is on purchasing a product rather than receiving professional assistance from the pharmacist. No wonder the significance occurrence of BD in CP than HP practice.
The study was limited to community and hospital pharmacists and it was discovered that community pharmacists face greater ethical difficulties than hospital pharmacists. However, the limitation of this study is that it does not elaborate how the respondents handle bioethical dilemma when confronted with it. The disposition of the pharmacists to the various quandaries scenario were not investigated and reported.
Conclusion
This research though, introductory in nature, it vividly illustrates the critical need for increased knowledge, education and promotion of resources to promote bioethics knowledge in pharmacy practice. A situation in which bioethical difficulties arise frequently but there are no facilities, personnel, or other resources to deal with them begs for intervention in pharmacy practice in Rivers State. There is a pressing need to provide a comprehensive stand-alone pharmacy ethics course in the pharmacy curriculum of our Nigerian Universities. This research needs to be replicated in other parts of Nigeria and it needs to be broadened to include pharmacist behaviours in bioethical challenges.
References
- Fakeye TO, Adisa R, Olukotun RT, Morawo PK (2017) Hospital and community pharmacists' perception of the scope, barriers and challenges of pharmacy practice-based research in Nigeria. Pharm Pract (Granada) 15: 881.
[Crossref], [Google Scholar], [Indexed]
- Federation I (2000) FIP statement of policy on good pharmacy education practice.
- Bhuvan K, Alrasheedy AA, Leggat PA, Molugulu N, Ibrahim MIM, et al. (2022) Pharmacies in the airport ecosystem and how they serve travelers’ health and medicines need: Findings and implications for the future. Integr Pharm Res Pract 11: 9-19.
[Crossref], [Google Scholar], [Indexed]
- Habeeb IA, Jose D, Jegan R (2012) Pharmacists in the wider public health workforce-a review. Arch Pharm Pract 3: 166-169.
- Mohiuddin AK (2020) The excellence of pharmacy practice. Innov Pharm 11: 1-21.
[Crossref], [Google Scholar], [Indexed]
- Melton BL, Lai Z (2017) Review of community pharmacy services: What is being performed, and where are the opportunities for improvement? Integr Pharm Res Pract 6: 79-89.
[Crossref], [Google Scholar], [Indexed]
- Simegn W, Weldegerima B, Endeshaw A, Sisay G, Mohammed A, et al. (2021) Assessment of community pharmacy professionals’ attitude and perception towards ethical issues in Amhara Region, Ethiopia: A cross-sectional survey 2020. Risk Manag Healthc Policy 14: 4127-4139.
[Crossref], [Google Scholar], [Indexed]
- Mossialos E, Courtin E, Naci H, Benrimoj S, Bouvy M, et al. (2015) From “retailers” to health care providers: Transforming the role of community pharmacists in chronic disease management. Health Policy 119: 628-639.
[Crossref], [Google Scholar], [Indexed]
- Raiche T, Pammett R, Dattani S, Dolovich L, Hamilton K, et al. (2020) Community pharmacists' evolving role in Canadian primary health care: A vision of harmonization in a patchwork system. Pharm Pract (Grenada) 18: 2171.
[Crossref], [Google Scholar], [Indexed]
- Yang S, Kim D, Choi HJ, Chang MJ (2016) Comparison of patients’ and pharmacists’ satisfaction with medication counseling provided by community pharmacies: A cross-sectional survey. BMC Health Serv Res 16: 131.
[Crossref], [Google Scholar], [Indexed]
- Fredrickson ME, Terlizzi H, Horne RL, Dannemiller S (2020) The role of the community pharmacist in veterinary patient care: A cross-sectional study of pharmacist and veterinarian viewpoints. Pharm Pract (Granada) 18: 1928.
[Crossref], [Google Scholar], [Indexed]
- Goode JV, Owen J, Page A, Gatewood S (2019) Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharmacy (Basel) 7: 106.
[Crossref], [Google Scholar], [Indexed]
- Milosavljevic A, Aspden T, Harrison J (2018) Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int J Pharm Pract 26: 387-397.
[Crossref], [Google Scholar], [Indexed]
- Rajiah K, Sivarasa S, Maharajan MK (2021) Impact of pharmacists’ interventions and patients’ decision on health outcomes in terms of medication adherence and quality use of medicines among patients attending community pharmacies: A systematic review. Int J Environ Res Public Health 18: 4392.
[Crossref], [Google Scholar], [Indexed]
- Agomo CO, Ogunleye J, Portlock J (2020) Enhancing the public health role of community pharmacists-a qualitative research utilising the theoretical domains framework. Innov Pharm 11: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Strand MA, Tellers J, Patterson A, Ross A, Palombi L (2016) The achievement of public health services in pharmacy practice: A literature review. Res Social Adm Pharm 12: 247-256.
[Crossref], [Google Scholar], [Indexed]
- Grey E, Harris M, Rodham K, Weiss MC (2016) Characteristics of good quality pharmaceutical services common to community pharmacies and dispensing general practices. Int J Pharm Pract 24: 311-318.
[Crossref], [Google Scholar], [Indexed]
- Zunic L, Masic I (2014) What pharmacy practitioners need to know about ethics in scientific publishing. J Res Pharm Pract 3: 112-116.
[Crossref], [Google Scholar], [Indexed]
- LeBlanc AB, Williams-Jones B, Aenishaenslin C (2022) Bio-ethics and one health: A case study approach to building reflexive governance. Front Public Health.
[Crossref], [Google Scholar], [Indexed]
- Ayala FJ (2010) The difference of being human: Morality. Proc Natl Acad Sci USA 107: 9015-9022.
[Crossref], [Google Scholar], [Indexed]
- Monsudi KF, Oladele TO, Nasir AA, Ayanniyi AA (2015) Medical ethics in sub-Sahara Africa: Closing the gaps. Afr Health Sci 15: 673-681.
[Crossref], [Google Scholar], [Indexed]
- Javadi M, Ashrafi N, Salari P (2018) Assessment of pharmacists experiences and attitudes toward professionalism and its challenges in pharmacy practice. Iran J Pharm Res 17: 168-177.
[Google Scholar], [Indexed]
- Pellegrino ED (2002) Professionalism, profession and the virtues of the good physician. Mt Sinai J Med 69: 378-384.
[Google Scholar], [Indexed]
- Al-Qudah RA, Tuza O, Tawfiek H, Chaar B, Basheti IA (2019) Community pharmacy ethical practice in Jordan: Assessing attitude, needs and barriers. Pharm Pract (Granada) 17: 1386.
[Crossref], [Google Scholar], [Indexed]
- Erstad BL, Stratton TP (2022) The importance of teaching ethics in pharmacy education. Am J Pharm Educ 86: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Zeeman JM, Kiser SN, Steeb DR, Hubal R (2020) Identifying priority student leadership and professionalism attributes among faculty, preceptors and students via modified Delphi. Am J Pharm Educ 84: 8076.
[Crossref], [Google Scholar], [Indexed]
- Ismail S, Osman M, Abulezz R, Alhamdan H, Quadri KHM (2018) Pharmacists as inter-professional collaborators and leaders through clinical pathways. Pharm 6: 24.
[Crossref], [Google Scholar], [Indexed]
- Bronkhorst E, Gous AG, Schellack N (2020) Practice guidelines for clinical pharmacists in middle to low income countries. Front Pharmacol 11: 978.
[Crossref], [Google Scholar], [Indexed]
- Hibbert D, Bissell P, Ward PR (2002) Consumerism and professional work in the community pharmacy. Sociol Health Illn 24: 46-65.
[Crossref], [Google Scholar], [Indexed]
- Stevenson FA, Leontowitsch M, Duggan C (2008) Over-the-counter medicines: Professional expertise and consumer discourses. Sociol Health Illn 30: 913-928.
[Crossref], [Google Scholar], [Indexed]
- Kho BP, Hassali MA, Lim CJ, Saleem F (2017) Challenges in the management of community pharmacies in Malaysia. Pharm Pract (Granada) 15: 933.
[Crossref], [Google Scholar], [Indexed]
- Kruijtbosch M, Göttgens-Jansen W, Floor-Schreudering A, van Leeuwen E, Bouvy ML (2018) Moral dilemmas of community pharmacists: A narrative study. Int J Clin Pharm 40: 74-83.
[Crossref], [Google Scholar], [Indexed]
- Kruijtbosch M, Göttgens-Jansen W, Floor-Schreudering A, van Leeuwen E, Bouvy ML (2019) Moral dilemmas reflect professional core values of pharmacists in community pharmacy. Int J Pharm Pract 27: 140-148.
[Crossref], [Google Scholar], [Indexed]
- Yolanda S (2019) Ethics in pharmacy. News-Medical. Australia: AZoNetwork
- Rajiah K, Venkataraman R (2018) Community pharmacists’ perceptions on ethical dilemmas, pharmacy values and decision-making. Indian J Pharm Pract 11: 5-10.
- Rodríguez JV, Juricic Ž (2018) Perceptions and attitudes of community pharmacists toward professional ethics and ethical dilemmas in the workplace. Res Social Adm Pharm 14: 441-450.
[Crossref], [Google Scholar], [Indexed]
- Cipolle RJ, Strand LM, Morley PC (2012) Pharmaceutical care practice: The patient-centered approach to medication management services. (3rd ed), McGraw Hill Education, LLC, New York City, USA.
- Moltó-Puigmartí C, Vonk R, van Ommeren G, Hegger I (2018) A logic model for pharmaceutical care. J Health Serv Res Policy 23: 148-157.
[Crossref], [Google Scholar], [Indexed]
- Kheir N, Awaisu A, Ibrahim S, Al-Dulaimi SM, Gad H (2019) Perspectives of pharmacy graduates toward an undergraduate ethics course and its potential impact on their professional practice. Adv Med Educ Pract 10: 1047-1056.
[Crossref], [Google Scholar], [Indexed]
- Orayj K, Alahmari K, Alasiri M (2022) The concept of pharmacy ethics and the examples of ethical dilemmas encountered by pharmacists in the Asir Region, Saudi Arabia: A qualitative study. Int J Gen Med 15: 4985-4996.
[Crossref], [Google Scholar], [Indexed]
- Popattia AS, Winch S, La Caze A (2018) Ethical responsibilities of pharmacists when selling complementary medicines: A systematic review. Int J Pharm Pract 26: 93-103.
[Crossref], [Google Scholar], [Indexed]
- Schlesselman LS (2014) A cross-sectional study of applied bioethical reasoning in pharmacy students and preceptors. Pharm Pract 12: 401.
[Google Scholar], [Indexed]
- Hirota N, Okamura N (2020) Patients’ attitudes, awareness and opinions about community pharmacies in Japan: Next steps for the health support pharmacy system. Integr Pharm Res Pract 9: 243-256.
[Crossref], [Google Scholar], [Indexed]
- Sepp K, Cavaco AM, Raal A, Volmer D (2021) Profession driven improvement of the quality of pharmacy practice-implementation of community pharmacy services quality guidelines in Estonia. Healthcare (Basel) 9: 804.
[Crossref], [Google Scholar], [Indexed]
- Atkinson J, Pozo AS, Rekkas D, Volmer D, Hirvonen J, et al. (2016) Hospital and community pharmacists’ perceptions of which competences are important for their practice. Pharmacy (Basel) 4: 21.
[Crossref], [Google Scholar], [Indexed]
- Lopes H, Lopes AR, Farinha H, Martins AP (2021) Defining clinical pharmacy and support activities indicators for hospital practice using a combined nominal and focus group technique. Int J Clin Pharm 43: 1660-1682.
[Crossref], [Google Scholar], [Indexed]
- Onatade R, Appiah S, Stephens M, Garelick H (2018) Evidence for the outcomes and impact of clinical pharmacy: Context of UK hospital pharmacy practice. Eur J Hosp Pharm 25: e21-e28.
[Crossref], [Google Scholar], [Indexed]
- Albadr Y, Khan TM (2015) Factors influencing community pharmacist decision to dispense generic or branded medicines; eastern province, Alahsa, Saudi Arabia. Saudi Pharm J 23: 143-146.
[Crossref], [Google Scholar], [Indexed]
- Al-Arifi MN (2014) Community pharmacist perception and attitude toward ethical issues at community pharmacy setting in central Saudi Arabia. Saudi Pharm J 22: 315-325.
[Crossref], [Google Scholar], [Indexed]
- Okoro RN, Jamiu MO (2020) Ethics education for contemporary clinical pharmacy practice in Africa. Indian J Med Ethics 6: 1-7.
[Crossref], [Google Scholar], [Indexed]
- Okoro RN (2019) Ethics education for contemporary clinical pharmacy practice in Nigeria: Shortfalls and needs. Bangladesh J Bioeth 10: 1-5.
[Crossref], [Google Scholar]
- Kasher A (2005) Professional ethics and collective professional autonomy: A conceptual analysis. Ethical Perspect 12: 67-97.
[Crossref], [Google Scholar], [Indexed]
- Worley MM, Schommer JC, Brown LM, Hadsall RS, Ranelli PL, et al. (2007) Pharmacists' and patients' roles in the pharmacist-patient relationship: Are pharmacists and patients reading from the same relationship script? Res Social Adm Pharm 3: 47-69.
[Crossref], [Google Scholar], [Indexed]
- Deans Z (2010) Ethics in pharmacy practice. (1st ed), Pharm Pract Res Trust, 1 Lambeth High Street, London.
- Fairhurst K, May C (1995) Consumerism and the consultation: The doctor's view. Fam Pract 12: 389-391.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences