J Pouch - How to Gain Length
Fazl Q Parray*
Department of General and Minimal Invasive Surgery, Sher-i-Kashmir Institute of Medical Sciences, Jammu and Kashmir, India
- *Corresponding Author:
- Parray FQ
Department of General and Minimal Invasive Surgery
Sher-i-Kashmir Institute of Medical Sciences, Srinagar-190011
Jammu and Kashmir, India
Tel: 9419008550
E-mail: fazlparray@rediffmail.com
Received Date: November 01, 2016; Accepted Date: November 02, 2016; Published Date: November 03, 2016
Citation: Parray FQ (2016) J Pouch-How to Gain Length. J Surgery Emerg Med 1:1.
Copyright: © 2016 Parray FQ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Editorial
Colorectal surgery in the last 2 decades has seen a great deal of growth owing to technical advances like introduction of staplers, energy sources, laparoscopic and robotic surgery. The new technology has made more technically demanding procedures more acceptable and hence more colorectal centers all over the world are now performing more volume of technically demanding surgeries and increasing their expertise with each passing year.
Our centre is a tertiary care institute catering to a population of 10 million people in the valley of Kashmir. Diseases like colorectal cancer (CRC), Ulcerative colitis (UC) and Familial adenomatous polyposis (FAP) constitute a significant volume of our colorectal surgery; hence surgeries like low anterior resection (LAR), ultra-low resection (ULAR), intersphincteric resection (ISR), total proctocolectomies (TPC) by open or laparoscopic means are frequently performed. After performing these surgeries, all such patients suffer from loss of rectum or whole colon and rectum and their reservoir function or the water absorption function is lost. Such patients may suffer from problems like Anterior resection syndrome (ARS) or Low anterior resection syndrome ((LARS). This syndrome may present with increased stool frequency, increased urge, difficulty in evacuation of stools, increased soiling of under garments, feeling of incomplete evacuation and many associated functional disorders. The resultant anorectal dysfunction as a result of this syndrome is quite frustrating in the adaption period which is usually the first year post surgery [1,2]. Even though this syndrome is a known entity for many years but still lacks a standard definition. Bryant et al defined it as “disordered bowel function after rectal resection, leading to a detriment in quality of life (QOL)” [3].
In most patients the symptoms gradually start improving towards the completion of one year and a steady state is achieved by 1-2 years after surgery. This syndrome has a significant impact on QOL in many patients. In many studies severe bowel function disorder was observed in up to 75% patients on a long follow up after low anterior resection (LAR) [3-5].
To understand the pathogenesis of this symptom complex, anorectal manometry was used to as an investigative tool for studying these patients. The three most frequent findings were reduced anal tone, loss of rectoanal inhibitory reflex (RAIR) and reduced rectal compliance [6,7]. Many studies in the literature have tried to investigate the urgency and incontinence in these patients; which reported a large variation of 4-68% [8]. Bryant, et al. [3], report evacuation difficulties, incomplete emptying and clustering in the range of 2-74%. Better QOL was observed in patients of sphincter saving surgery than in patients subjected to a permanent stoma [9]. These observations, however, on QOL did change in anastomosis as low as 6 cm from anal verge; even though in areas of body image and sexual performance, sphincter saving procedures still scored better but these lower scores are balanced better in symptom, cognitive and social scores [10].
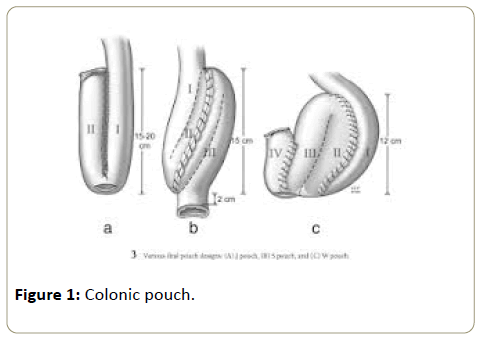
In order to save patients from the misery of development of this symptom complex, our department has a protocol to construct a J Pouch (neorectal reservoir) in these patients which really is of great benefit in markedly decreasing the symptoms of ARS/LARS [11,12]. Neo rectal reservoir is created to replace the natural reservoir. It can be a Colonic Pouch or an Ileal Pouch, design can be J, S, W, K, H, B and U (Figure 1). Neo rectal reservoir can also be constructed by coloplasty instead of a J Pouch but leak rates with coloplasty at times may be more in some studies but is not proved in randomized controlled studies [13]. Colonic J Pouch after LAR was introduced by Lazorthes to create a neorectum and since then it is being practiced worldwide [14].
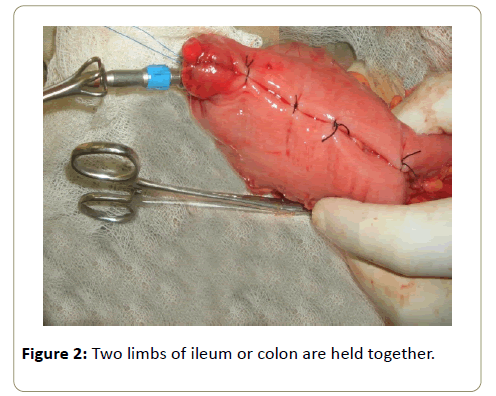
J Pouch is the commonest pouch for colon or ileum. It is quite popular with surgeons as compared to other pouches because it is technically easy to learn and construct. Colonic pouch is made after LAR or ULAR. Ileal pouch is made after TPC for FAP or UC. Each limb of Colonic J Pouch is 5-7 cms long. Each limb of Ileal Pouch is 12-15 cms long. The pouch is constructed in the shape of “J”. Two limbs of ileum or colon are held together by 3 or 4 stay sutures (Figures 2 and 3). A small enterotomy is made at the distal end of J and 2 limbs are stapled with 2-3 fires of advent 55 mm cartridge and converted into an artificial reservoir. The staple line is checked for any oozers which are suture ligated. The same end is then used to place the anvil of circular stapler before anastomosing the J Pouch to the anal canal.
Pouch will invariably reach pelvis comfortably but in some patients you observe difficulty because of obesity, adhesions, inadequate mobilization, thick mesentery, short vessels and small gut resection. Apex of Pouch 6 cms below pubic symphysis means adequate length and this will ensure a tension free anastomosis. Pouch in most cases will reach to low rectum or anus quite comfortably but in certain patients you find the length quite short and you may have to resort to some of the maneuvers mentioned below in order to ensure a tension free anastomosis.
For performing any TPC, divide terminal ileum flush with cecum or at the most 2-3 cms from cecum for constructing an ileal J Pouch (Figure 4). If you are a little liberal in taking more length of ileum along with the resection specimen of TPC, you will invariably fall short of length after pouch construction which can reach the low rectum or anal canal comfortably.
Another important thing to do is to divide all adhesions of small gut mesentery, also divide peritoneum on both sides of mesentery.
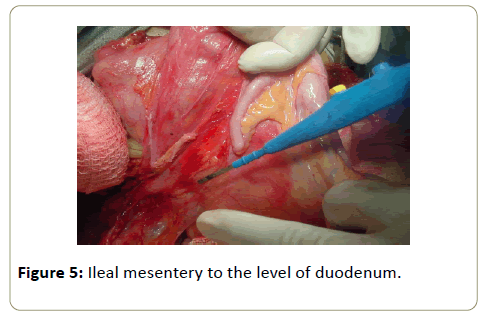
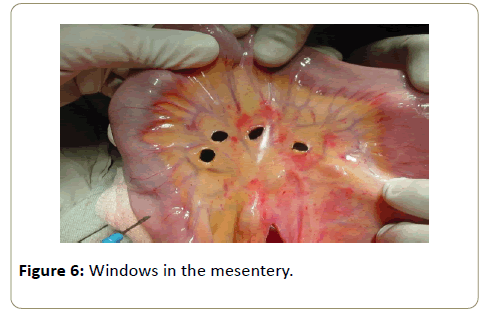
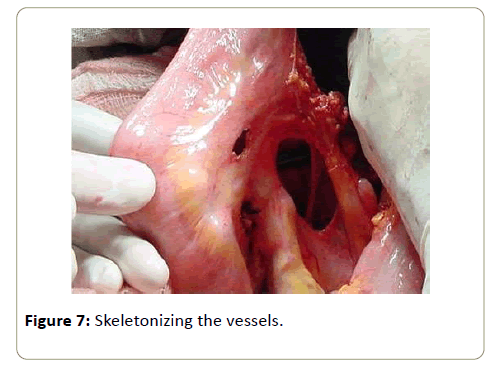
Mobilize terminal ileal mesentery to the level of duodenum (Figure 5). Make windows in the mesentery (Figure 6) and if length is still shorter, then skeletonize the vessels (Figure 7).
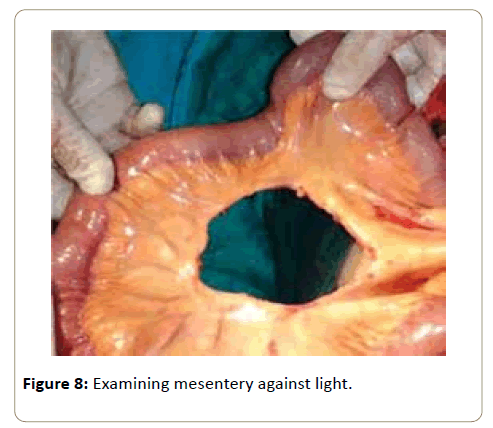
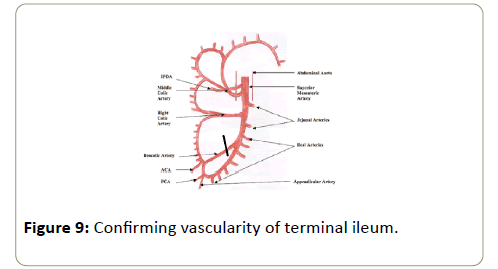
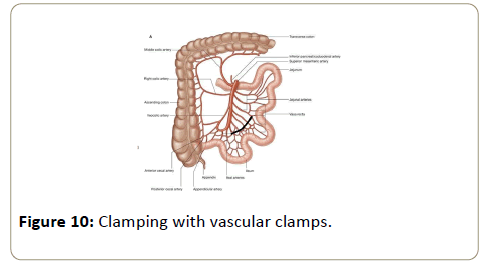
The additional maneuvers for gaining further length are that you can also cut smaller arcades after examining mesentery against light in case the length is still shorter (Figure 8). One can even go for the division of ileocolic artery (ICA) after confirming vascularity of terminal ileum, it may give you 3-7 cm length (Figure 9). If still you are not satisfied with the length of J for a tension free anastomosis, then go for the division of terminal divisions of superior mesenteric artery (SMA) after clamping with vascular clamps for 15 minutes and ensuring a good blood supply (Figure 10).
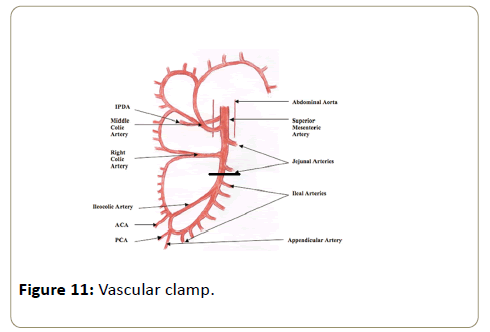
You can even go for the superior mesenteric artery pedicle division at the level of last jujenal branch but this maneuver should be practiced with extreme caution after again clamping with a vascular clamp for 15 minutes and ensuring that there are no color changes (Figure 11).
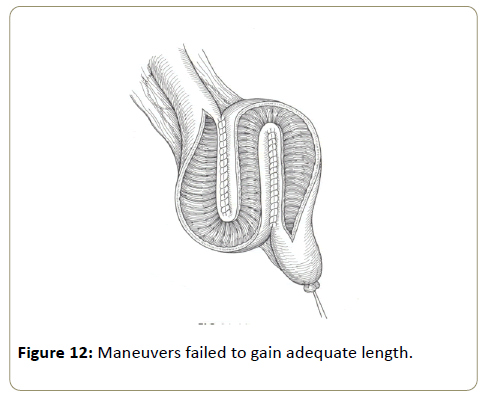
Use of S Pouch may add 2-3 cm more length in case all other maneuvers have failed to gain adequate length (Figure 12). Complete mobilization of splenic flexure after construction of colonic J pouch gives usually an adequate length for anastomosis.
A Proper, relaxed and a tension free anastomosis will ensure proper healing of the anastomosis. If all maneuvers fail, then it is better to make a stoma as a last resort to save life. Pouches preferably should be preferably covered with a covering or a temporary stoma for at least 6-12 weeks so that pouches heal well.
Pouchogram is a must before closure of the stoma to rule out any obstruction in the distal segment. Digital rectal examination is also a must before stoma closure to rule out any anastomotic stenosis.
References
- Lewis WG, Martin IG, Williamson ME, Stephenson BM, Holdsworth PJ, et al. (1995) Why do some patients experience poor functional results after anterior resection of the rectum for carcinoma. Dis Colon Rectum 38: 259-263.
- Miller AS, Lewis WG, Williamson ME, Holdsworth PJ, Johnston D, et al. (1995) Factors that influence functional outcome after colo-anal anastomosis for carcinoma of the rectum. Br J Surg 82: 1327-1330.
- Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL (2012) Anterior resection syndrome. Lancet Oncol 13: 403-408.
- Hallbook O, Sjodahl R (2000) Surgical approaches to obtaining optimal bowel function. Semin Surg Oncol 18: 249-258.
- Fazio VW, Zutshi M, Remzi FH, Parc Y, Ruppert R, et al. (2007) A randomized multicenter trial to compare long-term functional outcome, quality of life, and complications of surgical procedures for low rectal cancers. Ann Surg 246: 481-488.
- Iwai N, Hashimoto K, Yamne T, Kojima O, Nishioka B, et al. (1982) Physiologic states of anorectum following sphincter saving resection for carcinoma of the rectum. Dis colon rectum 25: 625-629.
- Batignani G, Monaci I, Ficari F, Tonelli F (1991) What affects continence after anterior resection of the rectum. Dis colon rectum 34: 329-335.
- Oya M, Komatsu J, Takase Y, Nakamura T, Ishikawa H (2002) Comparison of defecatory function after colonic J-pouch anastomosis and straight anastomosis for stapled low anterior resection: results of a prospective randomized trial. Surg Today 32: 104-110.
- Pachler J, Wille-Jorgensen P (2005) Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev.
- How P, Stelzner S, Branagan G, Bundy K, Chandrakumaran K, et al. (2012) Comparative quality of life in patients following abdominoperineal excision and low anterior resection for low rectal cancer. Dis Colon Rectum 55: 400-406.
- Parray FQ, Farouqi U, Chowdri NA (2011) Is neo-rectum a better option for low rectal cancers. In: Santoro GA (ed.) Rectal cancer-a multidisciplinary approach to management. InTech, Rijeka, Croatia.
- Parray FQ, Farouqi U, Wani ML, Chowdri NA, Shaheen F (2014) Colonic J pouch neo-rectum versus straight anastomosis for low rectal cancers. Indian J Cancer 51: 560-564.
- Parray FQ, Magray JA, Dar MA, Chowdri NA, Wani RA, et al. (2014) Coloplasty neorectum versus straight anastomosis in low rectal cancers. ISRN Surgery.
- Lazorthes F, Fages P, Chiotasso P, Lemozy J, Bloom E (1986) Resection of the rectum with construction of a colonic reservoir and coloanal anastomosis for carcinoma of the rectum. Br J Surg 73: 136-138.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences