Isolated Medial Cuneiform Fracture: A Case Report and Review of the Literature
Department of Orthopedics and Traumatology, Queen Elizabeth Hospital, Hong Kong
- *Corresponding Author:
- Dr Diane Hei-yan Tai
Department of Orthopedics and Traumatology
Queen Elizabeth Hospital, Hong Kong
Tel: (852)35068888
E-mail: dianetai510@yahoo.com
Received date: January 13,2017; Accepted date: February 27,2017; Published date: March 1,2017
Citation: Tai Hei-Yan D. Isolated Medial Cuneiform Fracture: A Case Report and Review of the Literature. J Emerg Trauma Care 2017. 2:1.
Abstract
We report a case of isolated medial cuneiform fracture in a 53-year-old gentleman. He presented with left foot dorsum pain after blunt injury to the foot. Plain X-ray showed widening between the medial and middle cuneiforms. Computerized tomography (CT) showed displaced intra-articular fracture of medial cuneiform. The fracture was anatomically reduced and internally fixed. Implants were removed at 3 months’ after operation. He regained full range of movement of the foot and ankle at 6 months.
Keywords
Isolated; Cuneiform; Fracture
Introduction
Isolated medial cuneiform fracture is a rare injury. It accounts for 1.7% of all tarsal fractures [1]. There were only a few case reports in the literature. It is often difficult to diagnose with plain X-ray. CT or magnetic resonance imaging (MRI) is helpful in diagnosing the fracture when there is clinical suspicion. The mechanism of injury is usually direct blow to the foot dorsum. It is frequently associated with other midfoot fractures. It could also be associated with tarsometatarsal fracture dislocation [2].
Clinical signs include tenderness over the talo-navicular and naviculo-cuneiform joints with inversion of the foot, resistive motion of the tibialis anterior and on direct palpation [3].
Case Report
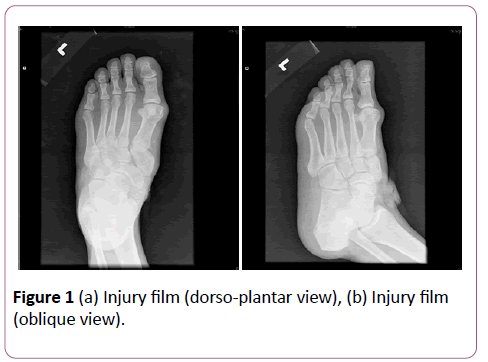
A 53-year old gentleman presented with left foot pain after blunt injury by a metallic board. On physical examination, there was an open wound, irregularly shaped, measured 4 cm × 4 cm, over left foot dorsum. The extensor halluces longus tendon was exposed but intact. X-ray of the left foot showed widening between the medial and middle cuneiforms, with suspicious fracture of the medial cuneiform (Figure 1a and 1b).
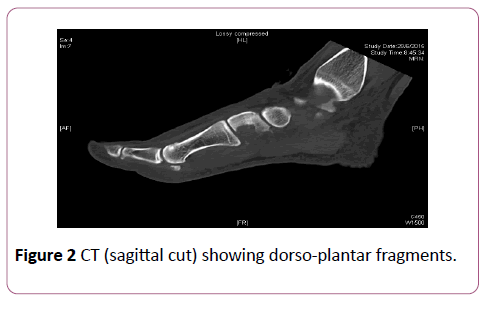
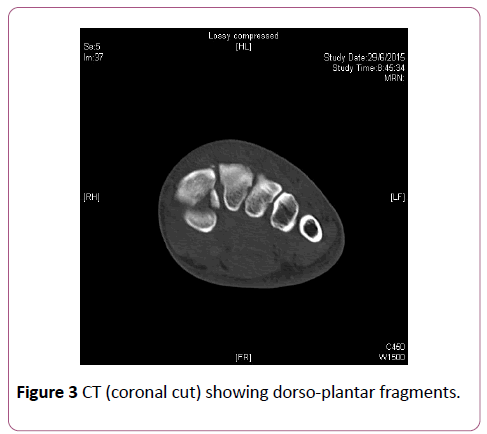
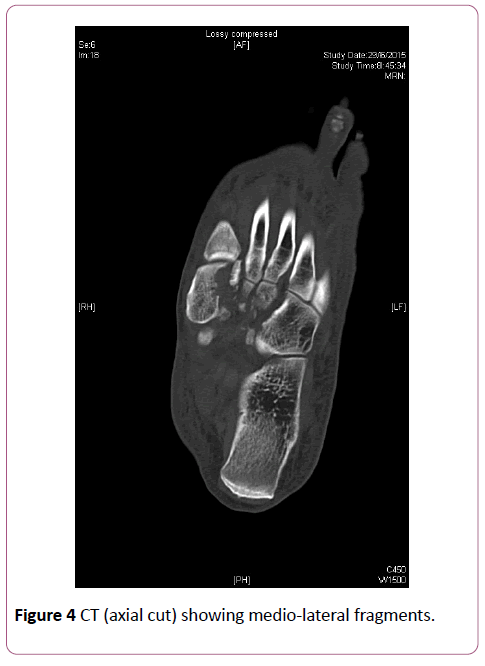
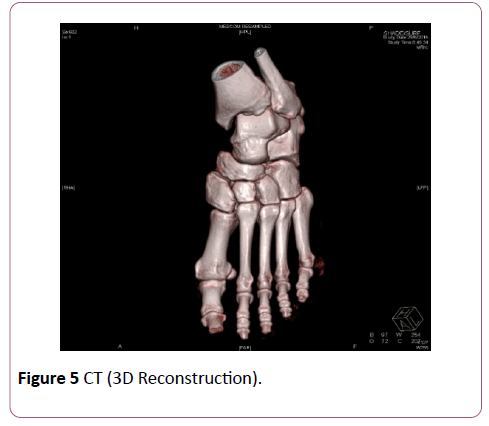
The patient underwent emergency operation for wound exploration and suturing. CT of the foot was arranged to rule out underlying Lisfranc injury and showed that there was comminute fracture of the latero-plantar aspect of medial cuneiform with displacement and extension to the tarsometatarsal joint; there was mild subluxation of medial cuneiform with separation between the medial and middle cuneiforms, there were tiny bone chips along the dorsal aspect of cuneiforms, which could be due to [2] avulsion associated with the dorsal inter-tarsal ligaments; there were also small 38 avulsion bone chips along plantar aspect of middle and lateral cuneiforms. The alignment of tarso-metatarsal joints was satisfactory (Figures 2-5).
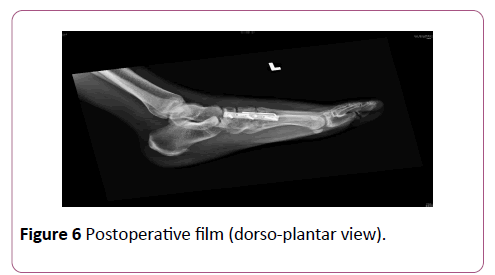
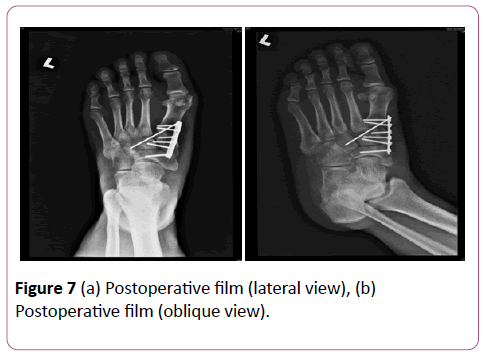
The fracture was fixed with one 2.7 mm 6-hole Titanium plate. One 1.6 mm K-wire was inserted across the midfoot for augmentation of the fixation (Figures 6 and 7). He was given an ankle-foot-orthosi sand started heel walking postoperatively.
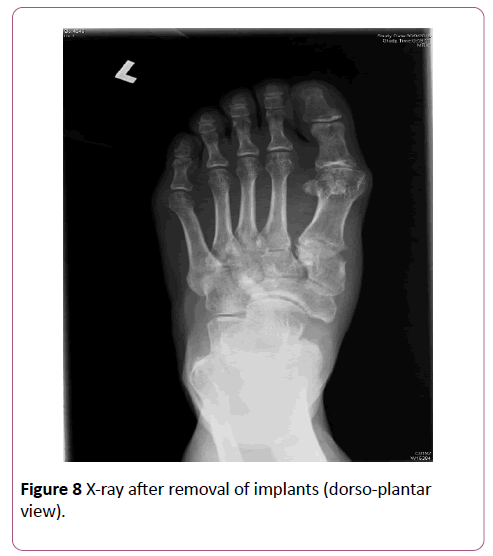
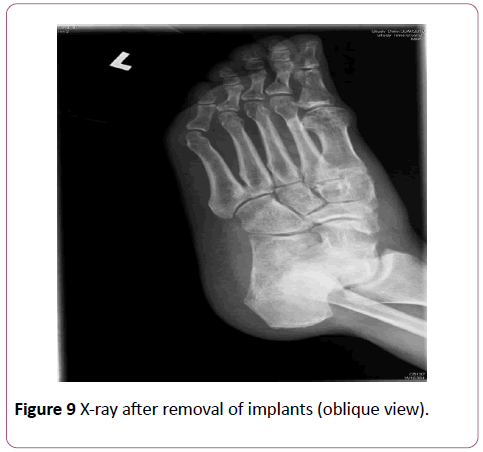
Implants were removed at 3 months after operation (Figures 8 and 9). He regained full range of movement of the foot and ankle at 6 months. However, he complained of some residual left foot pain. The visual analogue scale was 2 out of 10 at 10 months after operation.
Discussion
Isolated medial cuneiform fracture is a rare injury. X-ray findings could be subtle reported two cases with delayed diagnosis beyond 6 weeks [4] Diagnosis is delayed or missed due to difficulty in evaluating the fracture pattern with plain Xrays. It may also be missed because it is not considered in the differential diagnosis. A delay in diagnosis could make anatomical reduction impossible [5] CT or MRI is suggested if there is clinical suspicion. Associated mid-foot fractures must be excluded. Our patient presented with left midfoot pain and an open wound after blunt injury. X-ray showed widening between the medial and middle cuneiforms, with suspicious fracture of the medial cuneiform. It was also worried that there might be underlying injury to the Lisfranc ligament. However, CT showed that the alignment of tarso-metatarsal joints was satisfactory; and intra-operatively it was found that the Lisfranc ligament was stable.
It was also suggested in the literature that bipartite cuneiform should be ruled out, which is considered a variant of normal anatomy [6] Fracture could be either along the orizontal or coronal plane; whereas bipartite cuneiform is usually along the horizontal plane, i.e. dorso-plantar [7]. The fracture pattern in our patient was mainly dorso-plantar fragments with some comminution over the lateral aspect reported two cases of isolated medial cuneiform fracture treated 76 conservatively with cast [3]. They recommended non-displaced fractures should be treated with non-weight bearing cast for 6 weeks. Patterson et al reported one case of isolated medial cuneiform fracture. They recommended that this type of fracture should be anatomically fixed like any other displaced intra-articular fractures, to preserve the naviculocuneiform and tarsometatarsal joints [8]. However, there was no recommended measurement of displacement indicated for operative treatment. The author’s understanding is that any intra-articular fracture displacement of 2 mm would warrant operative management for this type of fracture.
Concerning the surgical technique for reduction, most authors suggested one single longitudinal incision over the medial cuneiform. Sangeorzan et al. recommended a combination of medial and dorsal approach [9]. It was because the medial cuneiform is draped by the anterior tibial tendon (ATT) on the medial side and obscured by the dorsal neurovascular bundle on the lateral side, dissection should be done with caution. The medial approach is directly medial overlying the ATT and dorsal to the posterior tibial tendon. The dorsal approach is medial to the neurovascular bundles. Complication of this fracture is extremely rare. There were two reports on non-union of the medial cuneiform fracture. Bryant et al reported one case of non-union in 1993 [10]. Alemdar reported one case of non-union in 2013 [11]. He suggested that displacement of the fracture fragments, instability of the fracture line, and soft tissue between might all contribute to non-union. Patients with non-union might complain of persistent midfoot pain.
Conclusion
Isolated medial cuneiform fracture is rare. Plain X-ray may not be sufficient to make diagnosis. CT or MRI should be done upon clinical suspicion. Like any intra-articular fractures this type of fracture should be anatomically fixed to retain the joint congruency. Complications include non-union are extremely rare.
References
- Wilson PD (1933) Fracture and dislocations of the tarsal bones. SouthMed J 131: 833.
- Cain PR, Seligson D (1981) Lisfranc’s fracture-dislocation with inter-cuneiformdislocation: Presentation of two cases and a plan for treatment.Foot Ankle 2:156-160.
- Olson RC, Mendicino SS, Rockett MS(2000) Isolated medial cuneiform fracture: Review of the literature and report of two cases.Foot & Ankle Int 21:150-153.
- Dysek M (1975) An isolated dislocation of the second cuneiform bone. Acta Chir Orthop TraumatolCech 42:390-392.
- Sanders JO, McGanity PLJ (1990) Intermediate cuneiform fracture-dislocation. J Orthop Trauma 4: 102-104.
- O’Neal ML, Ganey TM,Odgen JA (1995) Fracture of a bipartite medial cuneiform synchondrosis. Foot and Ankle Int 16:37-40.
- Guler F, Baz AB, Turan A, Kose O, Akalin S (2011) Isolated medial cuneiform fractures: Report of two cases and review of the literature. Foot and Ankle Spec 4:306-309.
- Patterson RH, Petersen D, Cunningham R(1993)Isolated fracture of the medial cuneiform. J Orthop Trauma 7:94-95.
- Sangeorzan BJ, Mayo KA Hansen ST (1993) Intra-articular fractures of the foot. Clin Orthop and Rel Res292:135-141.
- Bryant MJ, Baird DS(1993) A case of non-union of the medial cuneiform. Injury 24:207-208.
- Celil A, Yavuz UB, Azad Y, Ahmet K (2013) Non-union of the medial cuneiform: A rare case. Case Rep Med 2.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences