Is the Target therapy have a role in the treatment of Metastatic lung cancer in patients who is not fit for chemotherapy? Case Report
1Oncology Department, King Saud Medical City, Riyadh-KSA
2Oncology Department, Zagazig University, Zagazig-Egypt
3Microbiology Department, Faculty of Medicine, Fayoum University, Egypt
- *Corresponding Author:
- Ayman Rasmy
Consultant Medical Oncology, King Saud Medical City
Riyadh- Saudi Arabia
Tel: +00966-541899333
E-mail: a.rasmy@ksmc.med.sa
Received Date: April 24, 2018 Accepted Date: June 07, 2018 Published Date: June 26, 2018
Citation: Rasmy A, Mashiaki M, Ameen A (2018) Is The Target Therapy Have a Role in The Treatment of Metastatic Lung Cancer in Patients Who is Not Fit for Chemotherapy? Case Report. J Med Oncol. Vol.1 No.2:8
Abstract
Introduction: Lung cancer is the most common cause of cancer death worldwide, with an estimated 1.6 million deaths each year. Approximately 85% of patients have a group of histological subtypes collectively known as NSCLC, of which lung adenocarcinoma (LUAD) and lung squamous cell carcinoma (LUSC) are the most common subtypes.
Epidermal growth factor receptor (EGFR) and its mutations are found to have an important role in this cancer. Therefore, EGFR tyrosine kinase inhibitors (TKIs) can work effectively against NSCLC. Gefitinib and Erlotinib, which are a first generation TKI, and Afatinib, which is a second-generation TKI, are effective as a first-line therapy for advanced NSCLC.
Case report: We describe here a case of a 52 years old Saudi female nonsmoker who was diagnosed as a case of adenocarcinoma of lung origin with brain and inguinal lymph node metastasis. The patient underwent urgent brain surgery, received palliative radiotherapy and due to his poor general condition, she cannot received chemotherapy and started on Erlotinb before molecular study results and fortunately, the patient get excellent clinical response with good radiological response.
Keywords
Lung cancer; Non-small cell Lung cancer; Adenocarcinoma; Target therapy; Erlotinib
Introduction
Lung cancer is the main cause of cancer-related death worldwide, despite considerable progress in diagnostic and therapeutic approaches; people who smoke have the greatest risk of lung cancer. The risk of pulmonary adenocarcinoma increases substantially after a long duration of tobacco smoking, with a previous smoking duration of 30-40 years giving a relative risk of approximately 2.4 compared to never-smokers, and duration of more than 40 years giving a relative risk of approximately 5. This cancer is usually seen peripherally of the lungs [1-3].
Lung cancer typically doesn't cause signs and symptoms in its earliest stages. Signs and symptoms of lung cancer typically occur only when the disease is advanced which include a new cough that doesn't go away, coughing up blood, even a small amount, shortness of breath, chest pain, Hoarseness, weight lost and Bone pain [4].
Initial Diagnosis is by CT scan, sputum cytology, bronchoscopy, transthoracic needle aspiration (TTNA), or biopsy with histologic reference [5].
Adenocarcinoma of the lung is the most common type of lung cancer, and is characterized by distinct cellular and molecular features including gland and/or duct formation and/or production of significant amounts of mucus, so it is tends to stain as mucin positive and can also be distinguished by staining for TTF-1, a cell marker for adenocarcinoma.
Over the past 20 years, treatment has evolved from the empiric use of cytotoxic therapies to effective and better tolerated regimens that are targeted to specific molecular subtypes in LUAD, and therapies in development to target LUSC [1].
Case Report
A 52 years female with history of DM type II, complained of headache and dizziness for one month. 3 days after she started to experience increase in severity associated with neck pain radiating to the left arm. On the day of presentation she started having slurred speech. Upon examination, she was not in pain, conscious, alert, oriented and vitally/hemodynamically stable. Her systemic examinations were all unremarkable other than an ataxic gait on neurological examination with normal tone, power and sensory exam.
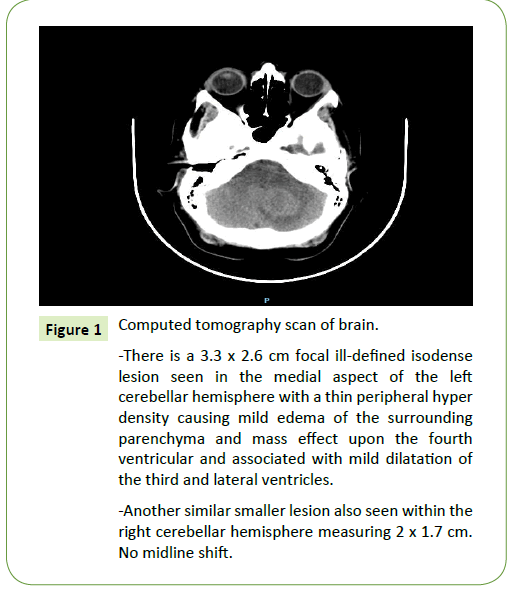
Her brain CT showed a 3.3 x 2.6 cm focal ill-defined isodense lesion seen in the medial aspect of the left cerebellar hemisphere with a thin peripheral hyper density causing mild edema of the surrounding parenchyma and mass effect upon the fourth ventricular and associated with mild dilatation of the third and lateral ventricles. Another similar smaller lesion also seen within the right cerebellar hemisphere measuring 2 x 1.7 cm. No midline shift (Figure 1).
Figure 1: Computed tomography scan of brain.
-There is a 3.3 x 2.6 cm focal ill-defined isodense
lesion seen in the medial aspect of the left
cerebellar hemisphere with a thin peripheral hyper
density causing mild edema of the surrounding
parenchyma and mass effect upon the fourth
ventricular and associated with mild dilatation of
the third and lateral ventricles.
-Another similar smaller lesion also seen within the
right cerebellar hemisphere measuring 2 x 1.7 cm.
No midline shift.
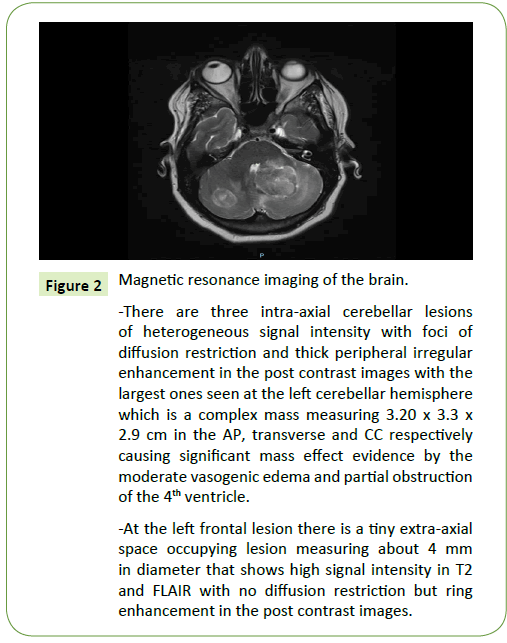
Her brain MRI showed three intra-axial cerebellar lesions of heterogeneous signal intensity with foci of diffusion restriction and thick peripheral irregular enhancement in the post contrast images with the largest ones seen at the left cerebellar hemisphere which is a complex mass measuring 3.20 x 3.3 x 2.9 cm in the AP, transverse and CC respectively causing significant mass effect evidence by the moderate vasogenic edema and partial obstruction of the 4th ventricle. At the left frontal lesion there is a tiny extra-axial space occupying lesion measuring about 4 mm in diameter that shows high signal intensity in T2 and FLAIR with no diffusion restriction but ring enhancement in the post contrast images (Figure 2).
Figure 2: Magnetic resonance imaging of the brain.
-There are three intra-axial cerebellar lesions
of heterogeneous signal intensity with foci of
diffusion restriction and thick peripheral irregular
enhancement in the post contrast images with the
largest ones seen at the left cerebellar hemisphere
which is a complex mass measuring 3.20 x 3.3 x
2.9 cm in the AP, transverse and CC respectively
causing significant mass effect evidence by the
moderate vasogenic edema and partial obstruction
of the 4th ventricle.
-At the left frontal lesion there is a tiny extra-axial
space occupying lesion measuring about 4 mm
in diameter that shows high signal intensity in T2
and FLAIR with no diffusion restriction but ring
enhancement in the post contrast images.
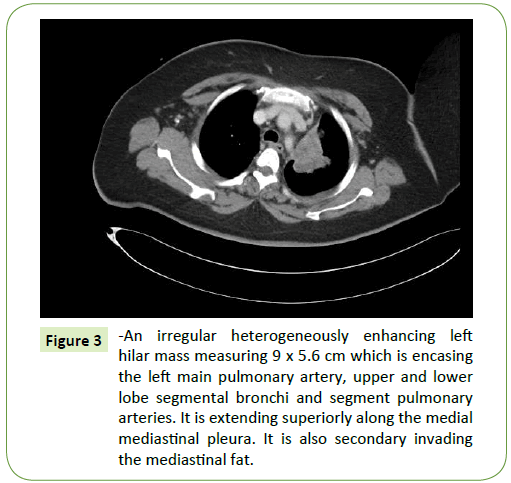
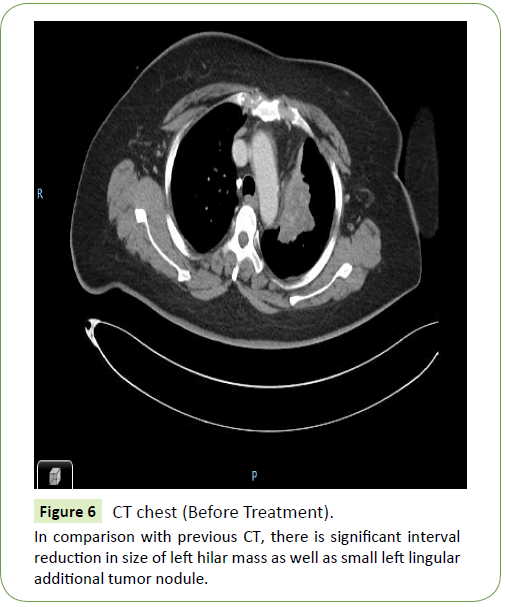
Her chest CT showed an irregular heterogeneously enhancing left hilar mass measuring 9 x 5.6 cm encasing the left main pulmonary artery, upper and lower lobe segmental bronchi and segment pulmonary arteries. It is extending superiorly along the medial mediastinal pleura invading the mediastinal fat. A small separate tumor nodule is noted at the medial aspect of the anterior segment of the left upper lobe which is closely abutting the mediastinal pleura. A few calcified small mediastinal lymph nodes are noted however no significant abnormal enlarged mediastinal lymph nodes. The right lung parenchyma is grossly unremarkable with exception of few calcific foci (Figure 3).
Figure 3: -An irregular heterogeneously enhancing left hilar mass measuring 9 x 5.6 cm which is encasing the left main pulmonary artery, upper and lower lobe segmental bronchi and segment pulmonary arteries. It is extending superiorly along the medial mediastinal pleura. It is also secondary invading the mediastinal fat.
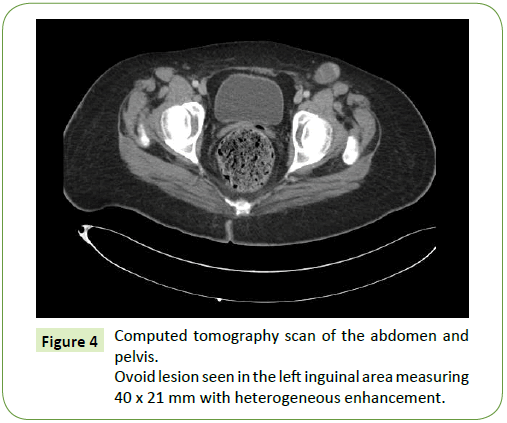
Her abdomen/pelvic CT showed a 3.2 cm anterior intramural uterine fundal lesion likely representing fibroid. No free fluid seen in the abdomen or pelvis. An ovoid lesion was seen in the left inguinal area measuring 40 x 21 mm with heterogeneous enhancement. Another small well-defined oval-shaped vertebral body lesions involving L3 and L5 probably hemangiomas. No destructive lesions seen in the lumbar vertebrae or pelvic bones (Figure 4).
Initially, she was managed conservatively by steroids. For her other radiological finding patient was referred to chest surgeon, for possible lung biopsy but an inguinal lymph node biopsy was taken instead due to its bigger size. The biopsy came as positive for adenocarcinoma (moderately differentiated); the tumour cells were positive for CK7 and TTF1, negative for CK20, ER, PR, Napsin A1, CDX2, and GCDP5-15 concluding that the primary origin is most likely the lungs.
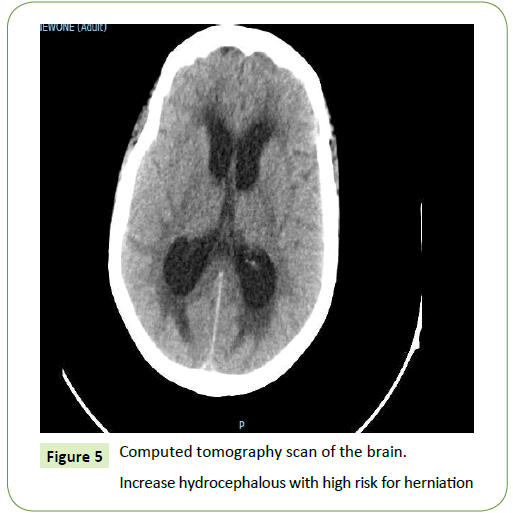
Before release of the pathology result, the patient had two episodes of falling in the ward; she was evaluated by neurosurgeon and neurologist. Urgent brain CT was requested revealing acute hydrocephalous with high risk for herniation (Figure 5). Patient was taken to Emergency OR for External Ventricular Drain (EVD).
Patient was shifted to ICU post EVD as she was on mechanical ventilator. However after stabilisation patient was shifted to General ward. Five days later, the patient underwent craniotomy and debunking of left cerebellar mass lesion. The excised cerebellar mass showed morphological features identical to those seen in the previous inguinal lymph node biopsy confirming the suspicion of metastatic adenocarcinoma of lung origin.
Patient post operatively was empirically started on meropenem and vancomycin, as before closure of EVD, CSF analysis was requested which showed WBC count rising to 95.000.
Patient was followed by neurosurgery, infectious disease team and primary team. Post removal of EVD, she complained of headache, therefore a new brain CT was requested revealing no new intracranial radiologic changes. Sutures were removed 5 days later. She was asked to continue antibiotics for 21 days. Patient was started on Erolitinib 150 mg OD
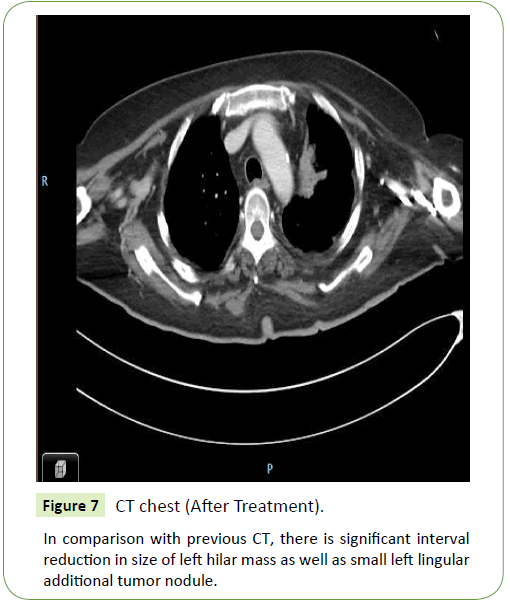
Throughout her hospital stay she was followed by physiotherapists and started to improve, she was able to sit on the edge of bed without support at the end however not ambulating. Patient was accepted for radiotherapy at KFMC from 8 November 2017. She was discharged in a stable state to home on 2/11/2017. With an advice to follow Oncology OPD and to continue Targeted therapy. Post targeted therapy her lung lesion started to shrink with no other abnormal findings in CT Brain.
In comparison with previous CT (Figure 6), there is significant interval reduction in size of left hilar mass as well as small left lingular additional tumor nodule (Figure 7).
Discussion
The high lung cancer mortality is due to the presence of metastatic disease at the time of diagnosis in most patients, indicating that improvements in long-term survival will require more effective systemic therapies. Molecularly targeted therapies in patients with NSCLC were initially used in the late 1990s with the introduction of gefitinib, an oral EGFR tyrosine kinase inhibitor (TKI). In unselected populations, the response rates were approximately 10%, with increased frequency of responses noted in females, never smokers, and patients of Asian populations [1].
Erlotinib, is TKI against EGFR, was associated with improved survival compared to the best supportive care in patients with previously treated advanced-stage NSCLC. In our case, as the patient not fit for chemotherapy, we have only two options, either no treatment with best supportive care only and we did not prefer this option because we want to treat patient with least toxic medication, so we go to second option with Erlotinib which is good tolerable, easy to use medication with fortunately excellent clinical response to the patient.
Conclusion
Although the treatment of patients with metastatic NSCLC has long been considered palliative and in case of patients who is not fit for chemotherapy, before to go to best supportive care, the target therapy is a good choice for the treatment of Metastatic lung cancer with good tolerance and minimal side effect. Furthermore, the use of new therapeutic modalities including immunotherapy may have a role in near future.
References
- Herbst RS, Morgensztern D, Boshoff C (2018) The biology and management of non-small cell lung cancer. Nature 553: 446-454.
- Rasmy A, Fotih S, Selwi W, Amal A (2016) Tyrosine Kinase Inhibitors in Advanced Adenocarcinoma of Lung Cancer: Are able to fight the disease or not? J. Canc. Stud. Ther. 1: 1-6.
- Alberg AJ, Brock MV, Stuart JM (2005) Epidemiology of lung cancer: Looking to the future. J. Clin. Oncol. 23: 3175-3185.
- Yang P, Allen MS, Aubry MC, Wampfler JA, Marks RS, et al. (2005) Clinical features of 5,628 primary lung cancer patients: experience at Mayo Clinic from 1997 to 2003. Chest. 128: 452-462.
- Rivera MP, Mehta AC, americans college of chest physicians (2007) Initial diagnosis of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 132: 131S–148S.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences