Increase In Metabolic Rate And Related Parameters During An Antigravity Treadmill Exercise Program In Neurological Patients
Anna Prunerova1*and Eldar Vinarov2
1Head of Rehabilitation at Spa Jánské Lázně, Jánské Lázně, Czech Republic
2Physiotherapist at Cerebrum Clinic, Tashkent, Uzbekistan
- *Corresponding Author:
- Anna Prunerová
Head of Rehabilitation at Spa Jánské Lázně, Janské Lázně,
Czech Republic
E-mail: prunerovaa@janskelazne.com
Received: June 01, 2023, Manuscript No. IPJNDD-23-16886; Editor assigned date: June 05, 2023, PreQC No. IPJNDD-23-16886 (PQ); Reviewed date: June 16, 2023, QC No. IPJNDD-23-16886; Revised date: June 23, 2023, Manuscript No. IPJNDD-23-16886 (R); Published date: June 30, 2023, DOI: 10.36648/ipjndd.6.4.4
Citation: Prunerová A, Vinarov E (2023) Increase in Metabolic Rate and Related Parameters during an Antigravity Treadmill Exercise Program in Neurological Patients. J Neurodegenero Dis Disord Vol.6 No.4: 4.
Abstract
Background: Neurological diseases and postoperative/post injury states are often associated with gait disorders requiring long-term rehabilitation. Controlled walking with fully or partially unloaded body weight represents a safe solution for gait impairment, preventing falls and excessive loading of the weakened segment.
Aim: The goal of this clinical trial is to evaluate and mutually compare the progress achieved during antigravity treadmill therapy in patients with various neurological conditions.
Methods: Fifty-six male and female participants recovering from neurological conditions experiencing gait impairment underwent six 20-minute treatment sessions scheduled two days apart. Treatment parameters such as speed, inclination and weight loading were reported during each session and their values were used for the calculation of the metabolic rate. The progress achieved between the first and the last treatment was evaluated.
Results: A significant increase in all therapy parameters was observed for all neurological indications. A comparison between-indication groups revealed a significant difference in metabolic rate, speed and inclination enhancement between postoperative/post injury states of the central nervous system, peripheral nervous system, and paresis after stroke.
Conclusion: Neurological patients with impaired gait experienced significant progress as part of an antigravity treadmill therapy exercise. Early integration of walking into rehabilitation programs promises an early return to home care and daily activities.
Keywords
Antigravity treadmill; Post-Stroke recovery; Postoperative/post injury states of CNS and PNS; Neurological conditions; Metabolic rate; Gait speed
Introduction
Neurological conditions are among the most common causes of disability. From the point of view of the years of life lived with a disability indicator, it is even among the top two most widespread. Stroke, cerebral palsy, Alzheimer’s disease, dementia and traumatic brain injuries are the most represented [1].
The clinical and social impact of disability is crucial and can severely affect a patient's autonomy. Patients with neurodegenerative diseases or after acute neurological conditions, including stroke and brain or spinal cord injuries can experience a progressive or long-term form of impairments [2]. These are often associated with immobility and gait disorders representing a large interference in patients’ daily activities [3] affecting about 60% of hospitalized neurological patients [4].
Neurological diseases and injuries can represent a directly life-threatening condition. In order to reduce patients’ mortality rate, a larger focus is brought on acute care than subsequent rehabilitation. Stroke reported the second highest mortality rate worldwide and most stroke survivors are experiencing disability in daily activities months after release into home care [2].
Depending on pathology and impairment, abnormal or reduced walking can be an indicator of disability or disease progression [3]. Predominant gait symptom is determined by the severity and extent of impaired segment or disease [4]. Parkinson’s disease is characterized by freezing of gait occurring in 38.2% of patients on medication while 32%-47% of stroke patients require supervision weightdue to increased risk of falls [4] and experience reduced mobility due to limited gait speed [5]. Spinal cord injury patients’ walking disability is due to lower limb paresis, increased spasticity, poor coordination and impaired postural control [6].
Restoration of locomotor function, capacity and speed is a high priority in integrating neurological patients into the community [4-6] and thus locomotor training promoting recovery of the central nervous system, muscle strength and spatiotemporal gait parameters should become an essential part of rehabilitation routine [6]. Walking exercise might become problematic in the case of neurological patients due to reduced balance and a high risk of falls and therefore a controlled weight-supported approach should be considered [4-6]. Antigravity treadmill training enables in-office walking or running exercise with partially unloaded body weight and enhanced safety preventing injuries caused by loss of balance and falls.
Clinical evidence describing the impact of antigravity treadmill exercises on patients recovering after neurological conditions is insufficient. Despite relatively satisfactory research on the effect on patients with Parkinson's disease, clinical evidence of its impact on other neurological diseases is lacking.
Miyai, et al., evaluated the immediate and long-term impact of treadmill training with body weight support in patients suffering from Parkinson’s disease [7,8]. Significantly greater improvement, when compared to conventional physiotherapy, has been reported. Similar results were concluded by Ganesan, et al., comparing standard gait training and partial weight-supported treadmill gait training with the control group [9]. Partial weightsupported training was considered a better treatment alternative for gait and balance rehabilitation in patients with Parkinson’s disease. Significant improvement of freezing of gait in patients with Parkinson’s disease has been concluded by Baizabal-Carvallo, et al., [10]. Plummer, et al., reported a significant impact of body weight supported treadmill on gait speed in post-stroke patients. Furthermore improved balance and walked distance have been noted [5]. Improvement in standing balance after a body weightsupported treadmill training program was also proved in patients with chronic spinal cord injury [6].
Basically, all studies focus specifically on one disease and the effect of therapy on parameters assessing the extent of health impairment. Research that would compare progress in antigravity treadmill therapy in patients with different indications is missing. The goal of this clinical trial is to evaluate and mutually compare progress achieved during antigravity treadmill therapy in patients with different neurological indications. Metabolic rate as a complex indicator of the therapy difficulty represents the primary outcome measure while remaining therapy parameters (speed, inclination and weight loading) will be evaluated as secondary outcomes.
Materials and Methods
The current trial was conducted at the medical Spa Jánské Lázně between September 2022 and March 2023. Patients requiring recovery after surgery or with a progressive disease completed the program in order to improve movement abilities to the extent of enabling discharge to home care. Participants recovering from neurological diseases or injuries requiring neuromuscular re-education who were considered suitable for antigravity treadmill therapy were assigned. Pregnant, noncooperative, and those diagnosed with severe cardiovascular disease, bronchial asthma or angina pectoris, severe disc herniation, epilepsy and conditions where increased abdominal pressure is contraindicated were excluded. Prior to the beginning of the treatment program, participants were informed about the course of the study and existing safety precautions. They signed an agreement with study participation and possible results publication. The study was designed in accordance with the 1975 Declaration of Helsinki ethical guidelines adopted by the General Assembly of the World Medical Association (1997-2000) and by the Convention on Human Rights and Biomedicine of the Council of Europe (1997) [11]. All patients underwent a 20 min antigravity treadmill exercise program followed by conventional rehabilitation. The antigravity treadmill parameters (speed, inclination, weight loading) were gradually increased based on the health capabilities of each patient. The therapy program consisted of 6 therapies scheduled 2 days apart (Figure 1).
Prior to the beginning of every treatment session, the antigravity treadmill system has to be precisely set and calibrated. The patient puts on shorts equipped with a half zipper allowing a sealed attachment to the inflatable bag forming an air-tight enclosure surrounding both the lower half of the patient's body and the treadmill itself. Next, the system is calibrated based on the patient's weight and therapy parameters are set. Speed (min: -8 km/h, max: 25 km/h), inclination (min: 0%, max: 15%) and weight unloading (min: 0%, max: 100%) determine how demanding the therapy will be. Weight unloading is controlled via air pressure created inside the inflatable bag- the higher the pressure, the higher the upward force offloading the patient's weight. This enables incorporating walking and running with a decreased percentage of body weight even in the early stages of recovery when patients are prone to impaired gait and falls [12,13].
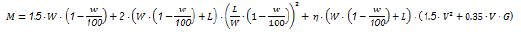
In order to estimate metabolic cost during partially weight unloaded exercise the adjusted equation by Pandolf, et al., [14] was used. Walking speed (V), treadmill inclination (G) and patient’s weight (W) lowered by the portion unloaded by the antigravity treadmill (w) were considered in the calculation. Terrain factor (η) was determined to be 1.0 for the treadmill surface and as patients had no additional load, carried load (L) equaled 0.
The secondary outcome measure comprises speed, inclination and weight loading parameters evaluation during the course of the study. Outcomes were reported during each treatment session, and a final assessment and comparison were prepared from data obtained during the first and the last exercise.
As, for the need of antigravity treadmill therapy, an adjusted metabolic rate equation was used, an estimate of sample size from previously published papers would be inaccurate. Hence parameter speed has been used instead. Based on existing clinical evidence evaluating gait speed in neurologic patients it was estimated that at least eight patients in each indication group would give 80% power to detect a significant (p<0.05) difference between the groups.
Data processing for statistical and visualization purposes was performed using a custom-written script (MatLab R2010b, Mathworks, Inc., Narick, MA, USA). Outcome measure data were evaluated for normality by the Shapiro-Wilk test. Non-parametric Wilcoxon sign rank test was used for the evaluation of statistical significance as normal data distribution has been rejected.The between-group comparison was performed by the Mann- Whitney U test. Data were expressed as median with Interquartile Range (IQR) and P<0.05 was considered significant.
Results
A total of 56 neurological patients, aged 60.55 ± 11.62, were assigned. Twenty-two participants were recovering after injury or surgery of the Central Nervous System (CNS) or Peripheral Nervous System (PNS), aged 52.57 ± 10.43, 13 were post-stroke patients, aged 67.31 ± 7.60 and the remaining 21 had other neurological conditions (Parkinson’s disease, neuromuscular disease, inflammation of CNS, infantile cerebral palsy, polyneuropathy or radicular syndromes), aged 64.18 ± 10.56. The study was generally well tolerated with no adverse events reported.
Metabolic rate
Before and after metabolic rate values with respective statistical significance for individual neurological conditions and their between-indication group comparison is summarized in Table 1.
| No of patients | Wilcoxon P (0.05) | Metabolic rate before | Metabolic rate after | Improvement | |
|---|---|---|---|---|---|
| Neurological conditions | 56 | <0.001 | 54.49 (20.49) | 104.69 (54.21) | 92% |
| Postoperative/postinjury states of CNS and PNS | 22 | <0.001 | 47.96 (16.43) | 130.52 (80.48) | 172% |
| Paresis after stroke | 13 | <0.001 | 54.22 (16.47) | 84.47 (48.40) | 56% |
| Other | 21 | <0.001 | 57.16 (24.93) | 97.52 (39.83) | 71% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative/postinjury states of CNS and PNS vs Paresis after stroke | 0.697 | 0.006 | ||
| Postoperative/postinjury states of CNS and PNS vs Other | 0.096 | 0.061 | |||
| Paresis after stroke vs Other | 0.167 | 0.120 | |||
Table 1: Metabolic rate values in W obtained during the first (before) and the last (after) treatment as Median (IQR). Statistical analysis comparing before and after (Wilcoxon) and between-indication group values is included (Mann-Whitney). Statistical tests reaching P<0.05 were considered significant.
All indications groups reported statistically significant enhancement of metabolic rate during the trial. Poststroke patients gained the least progress while patients in postoperative/post injury states of CNS and PNS showed the highest improvement of all indications groups. Between-group comparisons confirmed a significant difference in after-data between the postoperative/post injury states of CNS and PNS and post-stroke patients. A mutual comparison of initial data was left with no statistical significance.
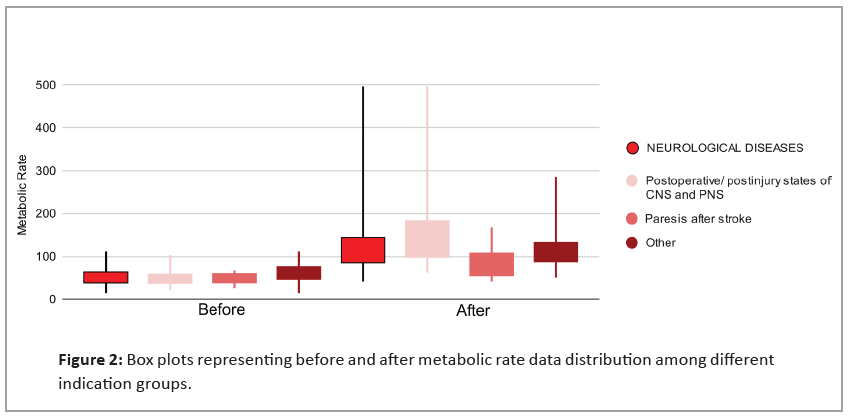
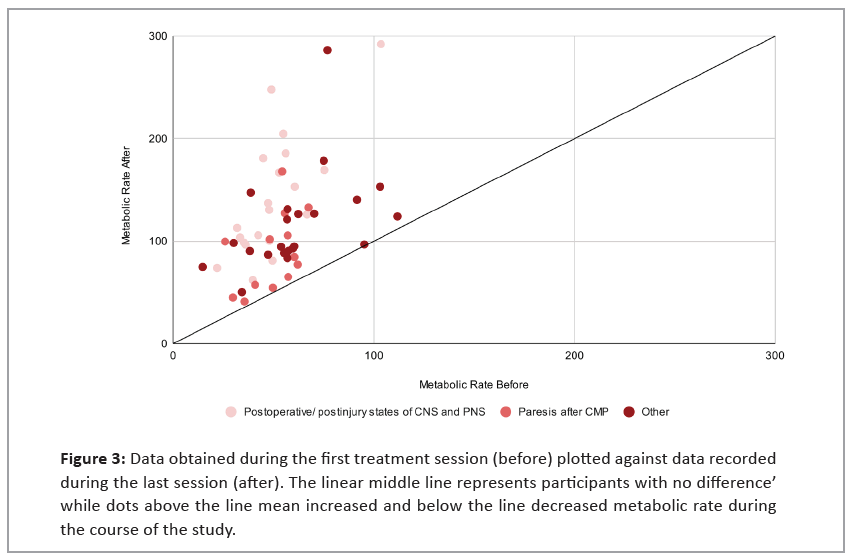
Figure 2 focuses on between groups data distribution and displays an increase in metabolic rate for all indication groups achieved between the first and the last treatment session. The significant difference between post-stroke patients and those recovering after surgery or injury of CNS and PNS is remarkable. Figure 3 visualizes differences achieved during the treatment program. There was only a single patient who did not gain any improvement.
Figure 3: Data obtained during the first treatment session (before) plotted against data recorded during the last session (after). The linear middle line represents participants with no difference’ while dots above the line mean increased and below the line decreased metabolic rate during the course of the study.
Before and after speed values with respective statistical significance for individual neurological conditions and their between-indication group comparison is summarized in Table 2.All indications groups reported statistically significant enhancement of speed during the trial. Patients recovering after surgery or injury of CNS and PNS made the biggest progress while post-stroke patients were left with minimal improvement. This was confirmed by Mann-Whitney test which revealed statistical significance in mutual after data comparison.
| No of patients | Wilcoxon P (0.05) | Speed before | Speed after | Improvement | |
|---|---|---|---|---|---|
| Neurological conditions | 56 | <0.001 | 1.20 (0.70) | 2.00 (1.05) | 67% |
| Postoperative/postinjury states of CNS and PNS | 22 | <0.001 | 1.20 (1.00) | 2.90 (1.00) | 142% |
| Paresis after stroke | 13 | 0.009 | 1.20 (0.40) | 1.40 (0.60) | 17% |
| Other | 21 | <0.001 | 1.1 (0.70) | 1.75 (0.88) | 59% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative/postinjury states of CNS and PNS vs Paresis after stroke | 0.129 | <0.001 | ||
| Postoperative/postinjury states of CNS and PNS vs Other | 0.358 | 0.041 | |||
| Paresis after stroke vs Other | 0.335 | 0.003 | |||
Table 2: Speed values in km/h obtained during the first (before) and the last (after) treatment session represented as Median (IQR). Statistical analysis comparing before and after (Wilcoxon) and between-indication group values are included (Mann-Whitney). Statistical tests reaching P<0.05 were considered significant.
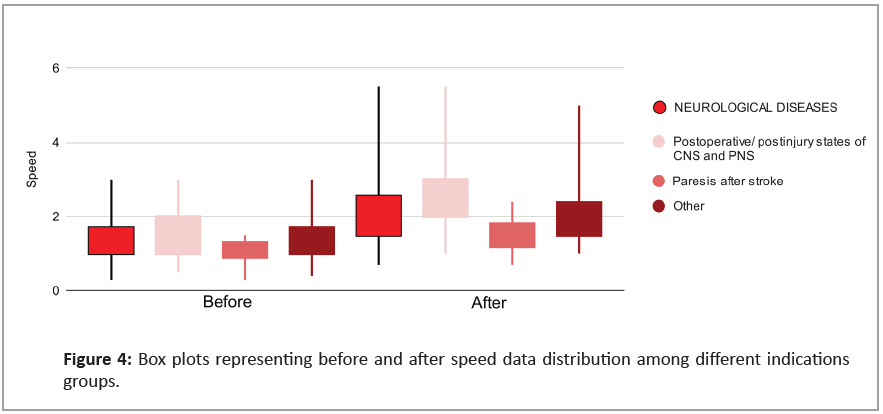
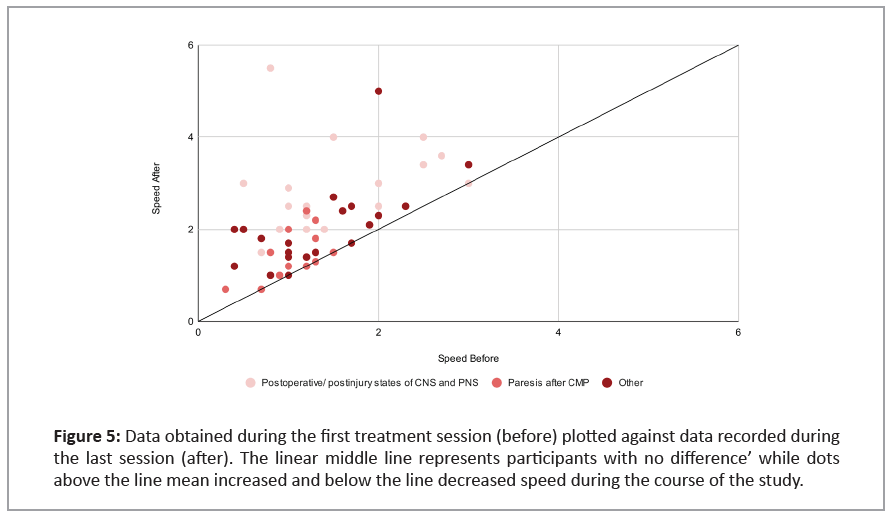
Figure 4 focuses on between groups data distribution and displays an increase in speed for all indication groups achieved between the first and the last treatment session. Significantly bigger progress achieved by postoperative/post injury of CNS and PNS patients are visible. A total of 7 patients did not experience any progress in terms of speed. Most of them were post-stroke patients (Figure 5).
Figure 5: Data obtained during the first treatment session (before) plotted against data recorded during the last session (after). The linear middle line represents participants with no difference’ while dots above the line mean increased and below the line decreased speed during the course of the study.
Inclination
Before and after inclination values with respective statistical significance for individual neurological conditions and their between-indication group comparison is summarized in Table 3.
| No of patients | Wilcoxon P (0.05) | Inclination before | Inclination after | Improvement | |
|---|---|---|---|---|---|
| Neurological conditions | 56 | <0.001 | 0.00 (3.00) | 5.00 (4.00) | NA |
| Postoperative/postinjury states of CNS and PNS | 22 | <0.001 | 0.00 (3.00) | 6.00 (7.00) | NA |
| Paresis after stroke | 13 | 0.014 | 0.00 (0.00) | 3.00 (3.00) | NA |
| Other | 21 | 0.008 | 0.00 (3.75) | 5.00 (1.75) | NA |
| Between-indication group Mann-Whitney P (0.05) | Postoperative/postinjury states of CNS and PNS vs Paresis after stroke | 0.191 | 0.03 | ||
| Postoperative/postinjury states of CNS and PNS vs Other | 0.851 | 0.391 | |||
| Paresis after stroke vs Other | 0.124 | 0.021 | |||
Table 3: Inclination values in % obtained during the first (before) and the last (after) treatment session represented as Median (IQR). Statistical analysis comparing before and after (Wilcoxon) and between-indication group values are included (Mann-Whitney). Statistical tests reaching P<0.05 were considered significant.
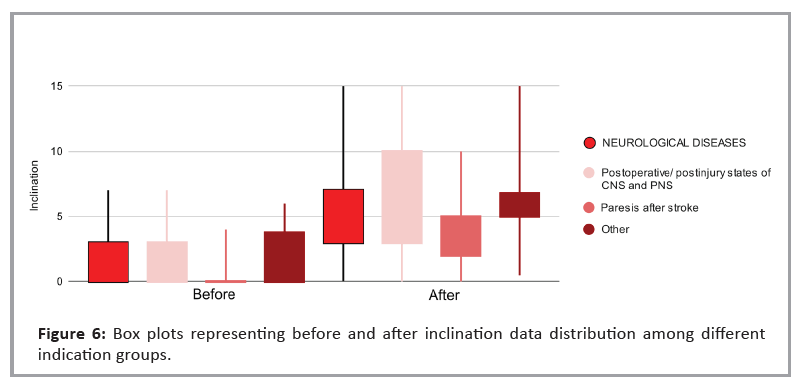
All indications groups reported statistically significant enhancement of inclination during the trial. A difference of statistical significance was found between after data of poststroke patients and remaining indications groups as visualized in between-groups data distribution (Figure 6).
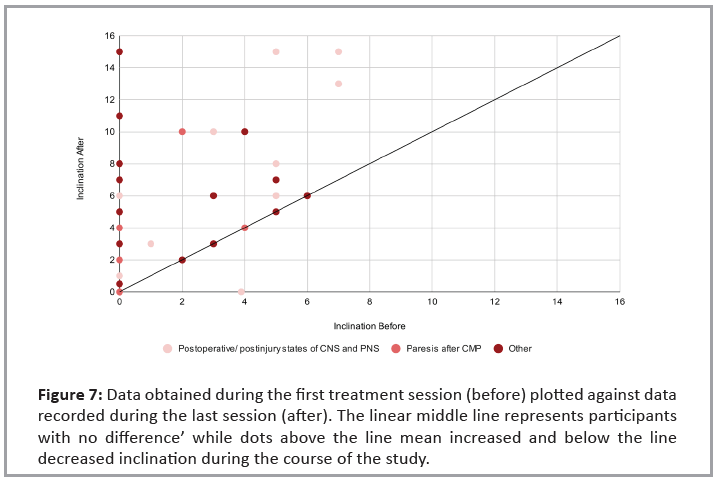
Six patients did not experience any change during the course of the study (Figure 7).
Figure 7: Data obtained during the first treatment session (before) plotted against data recorded during the last session (after). The linear middle line represents participants with no difference’ while dots above the line mean increased and below the line decreased inclination during the course of the study.
Weight loading
Before and after weight loading values with respective statistical significance for individual neurological conditions and their between-indication group comparison is summarized in Table 4.
| No of patients | Wilcoxon P (0.05) | Weight loading before | Weight loading after | Improvement | |
|---|---|---|---|---|---|
| Neurological conditions | 56 | <0.001 | 47.50 (10.00) | 52.50 (11.25) | 10% |
| Postoperative/postinjury states of CNS and PNS | 22 | <0.001 | 45.00 (15.00) | 50.00 (10.00) | 11% |
| Paresis after stroke | 13 | 0.014 | 50.00 (10.00) | 60.00 (10.00) | 20% |
| Other | 21 | 0.003 | 50.00 (10.00) | 50.00 (13.75) | 0% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative/postinjury states of CNS and PNS vs Paresis after stroke | 0.349 | 0.492 | ||
| Postoperative/postinjury states of CNS and PNS vs Other | 0.528 | 0.899 | |||
| Paresis after stroke vs Other | 0.682 | 0.621 | |||
Table 4: Weight loading values in % obtained during the first (before) and the last (after) treatment session represented as Median (IQR). Statistical analysis comparing before and after (Wilcoxon) and between-indication group values are included (Mann-Whitney). Statistical tests reaching P<0.05 were considered significant
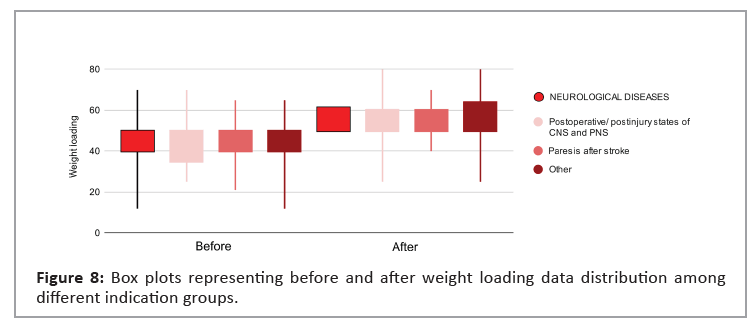
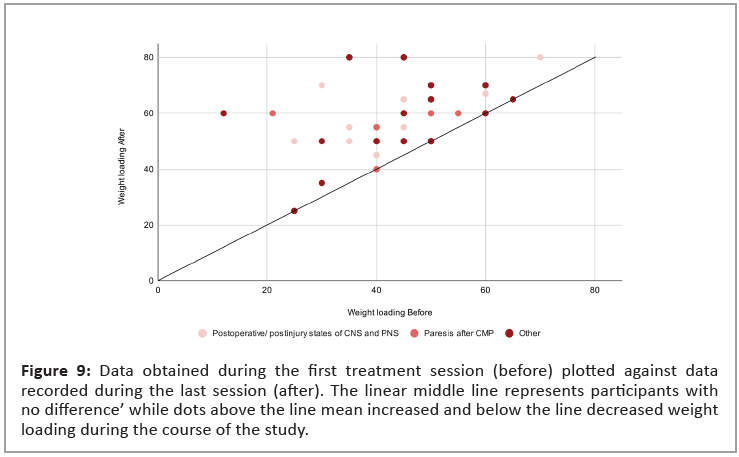
All indications groups reported statistically significant enhancement of weight loading during the trial. No significant difference was revealed by mutual between-indication group comparison as displayed in Figure 8 via indications groups data distribution visualization.
Five patients, the majority with other indications, were left with no improvement in the weight loading parameter (Figure 9).
Figure 9: Data obtained during the first treatment session (before) plotted against data recorded during the last session (after). The linear middle line represents participants with
no difference’ while dots above the line mean increased and below the line decreased weight loading during the course of the study.
Discussion
This is the first trial monitoring achieved progress during antigravity treadmill exercise in neurological patients of various indications. The research took place in a spa facility for patients requiring recovery after surgery or with progressive disease. The main goal of the program was to improve movement abilities to the extent of allowing discharge to home care. For this reason, patients were included in the early recovery stage and their condition did not allow them full weight loading during the course of the study. Hence, the locomotion enhancement was achieved mainly through increasing the remaining therapy parameters (speed, inclination).
A significant difference was reported in all therapy parameters including speed, inclination, weight loading and metabolic rate calculated by adjusted Pandolf, et al., equation [14]. This is in accordance with Plummer et al., who proved a significant impact of weight-supported treadmill therapy on gait speed in poststroke patients [5]. Remaining studies involving neurological patients focused rather on parameters assessing the extent of health impairment than therapy progress [6-10]. However, it can be assumed that the improvement in a patient's disability is closely related to the progress achieved during the exercise. Thus current findings could be considered as expected as the beneficial impact of an antigravity treadmill was proved by existing clinical evidence in patients with Parkinson’s disease [7-10], spinal cord injury and post-stroke patients [5,6].
Mutual between-indication group comparisons revealed significant differences between post-stroke patients and patients in postoperative/post injury states of CNS and PNS in metabolic rate, speed and inclination. There are several possible explanations. Probably the simplest reason is the significant age difference between the patients of both groups. While the average age of patients recovering after surgery or injury of CNS and PNS was 52.57 years of age, post-stroke patients were more than two decades older with an average age of 67.31. According to the existing clinical evidence, this age difference corresponds to population incidence as the mean age of post-stroke patients was 69.2 [15] and 83% of patients with peripheral nerve injury were under 55 years old [16]. Aging leads to a decrease in walking performance in terms of speed and the number of steps [17] and thus, treatment progress is limited. This assumption is consistent with the paper of Scivoletto, et al., describing a strong relationship between a patient's age and ability to walk after a spinal cord injury [18].
Another possible explanation of the significant betweenindications groups comparison is based on the difference between the recovery of a central and peripheral nerve injury. Unlike axons located in the central nervous system, peripheral nervous system axons readily regenerate enabling spontaneous recovery after peripheral nerve damage [19]. However, due to slow regeneration and misdirected reinnervation of motor axons, the functional outcomes even after peripheral nerve injury remain insufficient. English, et al., findings suggest a striking increase in peripheral nerve axon regeneration after a treadmill training program in terms of both speed and proper reinnervation [20]. On the contrary, a stroke represents serious damage to the CNS, and recovery of the disease in survivors is a lengthy process with slow progress, especially in terms of speed [5-21]. Limited improvement in gait speed during the rehabilitation process in post-stroke patients has been confirmed by multiple studies [21,22]. The indication group including patients with peripheral nervous system injury achieved the highest improvement while post-stroke patients reported the lowest enhancement in speed, inclination, and subsequently in metabolic rate.
The major limitation of the current trial is the low number of participants with certain indications. Due to this fact, the group “other” consists of patients with various neurological conditions, which significantly invalidates the recorded data and practically makes it impossible to draw any conclusions about this group. Other limitations include a missing control group for a better assessment of achieved progress, lack of parameters determining healing of impaired segments or disease progression and absence of follow-up. Instead of calculating metabolic rate from available therapeutic parameters, measurement tools providing more accurate outcomes could be used. Though, for the purpose of mutual comparison of indications groups, the estimated relative value is absolutely sufficient. Despite these shortcomings, the study can be considered beneficial as it is the first to compare the progress achieved during antigravity treadmill therapy in patients with different neurological indications. In the future, it would be appropriate to expand this study with other neurological diseases such as Parkinson's disease, multiple sclerosis, polyneuropathy, CNS inflammation and others.
Conclusion
Neurological patients with a gait impairment experienced significant progress as part of an antigravity treadmill therapy exercise. Although patients among all indication groups achieved significant results, a mutual data comparison revealed that participants after CNS and PNS injury/surgery experienced faster recovery than post-stroke patients. Early incorporation of walking into rehabilitation program promises a fast return to home care and daily activities in patients with various neurological conditions.
References
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, et al. (2021) Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396: 2006-2017.
[Crossref], [Google Scholar], [Indexed]
- Baricich A, Spitoni GF, Morone G (2022) Editorial: Long term disability in neurological disease: A rehabilitation perspective. Front Neurol 13: 964664.
[Crossref], [Google Scholar], [Indexed]
- Pearson OR, Busse ME, Deursen RWMV, Wiles CM (2004) Quantification of walking mobility in neurological disorders. QJM 97: 463-475.
[Crossref], [Google Scholar], [Indexed]
- Allali G, Blumen HM, Devanne H, Pirondini E, Delval A, et al. (2018) Brain imaging of locomotion in neurological conditions. Neurophysiol Clin 48: 337-359.
[Crossref], [Google Scholar], [Indexed]
- Plummer P, Behrman AL, Duncan PW, Spigel P, Saracino D, et al. (2007) Effects of stroke severity and training duration on locomotor recovery after stroke: A pilot study. Neurorehabil Neural Repair 21: 137-151.
[Crossref], [Google Scholar], [Indexed]
- Covarrubias-Escudero F, Rivera-Lillo G, Torres-Castro R, Varas-Díaz G (2017) Effects of body weight-support treadmill training on postural sway and gait independence in patients with chronic spinal cord injury. J Spinal Cord Med 42: 57-64.
[Crossref], [Google Scholar], [Indexed]
- Miyai I, Fujimoto Y, Ueda Y, Yamamoto H, Nozaki S, et al. (2000) Treadmill training with body weight support: its effect on Parkinson's disease. Arch Phys Med Rehabil 81: 849-852.
[Crossref], [Google Scholar], [Indexed]
- Miyai I, Fujimoto Y, Yamamoto H, Ueda Y, Saito T, et al. (2002) Long-term effect of body weight-supported treadmill training in Parkinson's disease: A randomized controlled trial. Arch Phys Med Rehabil 83: 1370-1373.
[Crossref], [Google Scholar], [Indexed]
- Ganesan M, Sathyaprabha TN, Gupta A, Pal PK (2014) Effect of partial weight-supported treadmill gait training on balance in patients with Parkinson disease. PMR 6: 22-33.
[Crossref], [Google Scholar], [Indexed]
- Baizabal-Carvallo JF, Alonso-Juarez M, Fekete R (2020) Anti-gravity treadmill training for freezing of gait in Parkinson's disease. Brain Sci 10: 739.
[Crossref], [Google Scholar], [Indexed]
- Council of Europe (1997) Convention for protection of human rights and dignity of the human being with regard to the application of biology and biomedicine: Convention on human rights and biomedicine. Kennedy Inst Ethics J 7: 277-290.
[Crossref], [Google Scholar], [Indexed]
- Stockland J, Russell Giveans M, Ames P (2019) The effect of an anti-gravity treadmill on running cadence. Int J Sports Phys Ther 14: 860-865.
[Crossref], [Google Scholar], [Indexed]
- Vincent HK, Madsen A, Vincent KR (2022) Role of antigravity training in rehabilitation and return to sport after running injuries. Arthrosc Sports Med Rehabil 4: e141-e149.
[Crossref], [Google Scholar], [Indexed]
- Pandolf KB, Givoni B, Goldman RF (1977) Predicting energy expenditure with loads while standing or walking very slowly. J Appl Physiol Respir Environ Exerc Physiol 43: 577-581.
[Crossref], [Google Scholar], [Indexed]
- Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, et al. (2012) Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology 79: 1781-1797.
[Crossref], [Google Scholar], [Indexed]
- Taylor CA, Braza D, Rice JB, Dillingham T (2008) The incidence of peripheral nerve injury in extremity trauma. Am J Phys Med Rehabil 87: 381-385.
[Crossref], [Google Scholar], [Indexed]
- Aoyagi Y, Park H, Watanabe E, Park S, Shephard RJ (2009) Habitual physical activity and physical fitness in older Japanese adults: The Nakanojo Study. Gerontology 55: 523-531.
[Crossref], [Google Scholar], [Indexed]
- Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M (2014) Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Front Hum Neurosci 8: 141.
[Crossref], [Google Scholar], [Indexed]
- Huebner EA, Strittmatter SM (2009) Axon regeneration in the peripheral and central nervous systems. Results Probl Cell Differ 48: 339-51.
[Crossref], [Google Scholar], [Indexed]
- English AW, Wilhelm JC, Sabatier MJ (2011) Enhancing recovery from peripheral nerve injury using treadmill training. Ann Anat 193: 354-361.
[Crossref], [Google Scholar], [Indexed]
- Gelaw AY, Balamurugan J, Teshome A, Ravichandran H (2019) Effectiveness of treadmill assisted gait training in stroke survivors: A systematic review and meta-analysis. Global Epidemiology.
[Crossref], [Google Scholar]
- Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, et al. (2011) Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med 364: 2026-2036.
[Crossref], [Google Scholar], [Indexed]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences