Heparin in Dialysis
Thomas Ryzlewicz*
Dialysis Centre, ViaMedis Riesa, Germany
- *Corresponding Author:
- Thomas Ryzlewicz
Dialysis Centre, ViaMedis Riesa, Germany
Tel: +49 172 836 66 25
E-mail: thomas.ryzlewicz@web.de
Received date: March 06, 2018; Accepted date: March 07, 2018; Published date: March 09, 2018
Citation: Ryzlewicz T (2018) Heparin in Dialysis. J Nephrol Transplant Vol.2: No.1: 1.
Abstract
In the 1930-ies, Strassmann and Hahn had done research for the nuclear decay of Uranium 238. The nuclear decay followed to an exponential function of natural logarithm. In the 1970ies, several medical doctors with facilities of mathematics while working in Nephrology, had developed the new discipline of Pharmacokinetics. Two of them were Dettli and Baethke. They recognized the same principle of decay in the drug elimination, the exponential function. They also introduced nearly the term, the biological half-life-time, in order to characterize the elimination of a drug
Editorial
In the 1930-ies, Strassmann and Hahn had done research for the nuclear decay of Uranium 238. The nuclear decay followed to an exponential function of natural logarithm. In the 1970- ies, several medical doctors with facilities of mathematics while working in Nephrology, had developed the new discipline of Pharmacokinetics. Two of them were Dettli and Baethke. They recognized the same principle of decay in the drug elimination, the exponential function. They also introduced nearly the term, the biological half-life-time, in order to characterize the elimination of a drug.
Heparin (regular, un-fragmented) had used for nearly every successful dialysis since Kolff and Alwall. Haas had tried without Heparin. There had been always thrombosis of the extracorporeal circuit. Heparin has a half-life-time of one hour, when it will used in i.v. supply. So this is a short half-life-time. Basics of Pharmacokinetics will tell, that a drug has disappeared clinically with the threefold half-life-time. With other words: Regarding clinical concentration, Heparin will be no longer present after three hours, when given in i.v. supply. Minimal rest concentrations will be present to 11-fold half-lifetime. But these, you never can use for clinical treatments.
Because of this short biological half-life-time of Heparin, the regular application of it had given nearly always in former times in a bolus at the start of the dialysis treatment and a continuous infusion with a pump. Today, a smaller number of dialysis centres does use only a bigger Heparin bolus at the start of dialysis and no longer a continuous Heparin infusion by a pump. Is this a problem?
With a bigger dosage of Heparin, this single bolus concept tries to overcome the realty of Pharmacokinetics: After one hour of dialysis treatment, there will be only half of this bigger dosage present, while the risk of clotting raises with the ongoing treatment time. Clearly spoken: There will be always a risk of clotting after hours of 3:30 h, growing the further dialysis treatment.
When clotting of the extracorporeal circuit hat appeared, today the EPO dosage will strongly elevated. This will also elevate the costs for the health insurances. But often, the way of settlement will differ in the way. Because of this, the enlargement of real world costs will not recognised. Savings of smaller costs, the Heparin perfusor syringe, can named for argumentations.
What is the best option of i.v. Heparin supply? At first, this remains the combination of a smaller bolus and a continuous infusion. At second (and this is the reason for this Editorial), a second bolus will be reasonable (instead of the continuous Heparin infusion) in order to prevent a frequent clotting of the extracorporeal unit. This does consider the short half-life-time of i.v. Heparin.
A last remark. In case of the target to use a minimal dosage of i.v. Heparin, you definitely should prefer the continuous Heparin infusion in order to avoid the pharmacokinetic saw tooth of this double bolus concept.
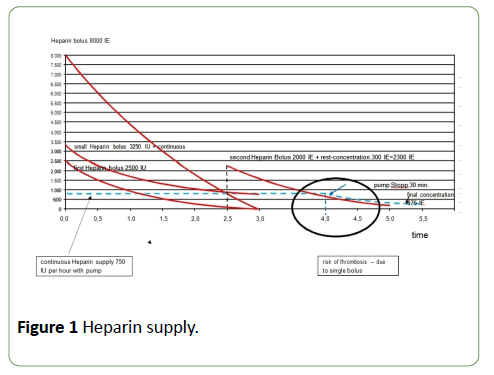
In the graph, you will see the different three concepts of i.v. Heparin supply as a principle:
1. Big single bolus.
2. Small bolus with continuous perfusor supply.
3. The second bolus concept expressed with the half-lifetime (Figure 1).
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences