ISSN : 2576-392X
Dentistry and Craniofacial Research
Have TADs Changed the Role of the Orthodontist in the Rehabilitation of the Degenerated Dentition?
Birte Melsen* and Morten Godtfredsen Laursen
Section of orthodontics,Department of Dentistry, Aarhus University, Vennelyst boulevard 9, 8000 Aarhus C
- *Corresponding Author:
- Birte Melsen
Department of Dentistry, Aarhus University. Holtevej 11, Denmark
Tel: +45 40646166
E-mail: birte@melsen.com
Received Date: August 01, 2017; Accepted Date: September 26, 2017; Published Date: October 04, 2017
Citation: Melsen B, Laursen MG (2017) Have TADs Changed the Role of Orthodontist in the Rehabilitation of the Degenerated Dentition? J Dent Craniofac Res. Vol. 2 No. 2:14. doi: 10.21767/2576-392X.100014
Abstract
The clinical routine has been undergoing continuous changes since it was defined by Angle[1]. Looking into the literature most changes occur following the presentation of a new approach. This was the case with the introduction of the skeletal anchorage by Creekmore [2] and Eklund. A hypothesis can be created based on single observations and research can be started. The present paper is a “story of the development of the skeletal anchorage and its usefulness” not only as an alternative to other anchorage approaches but when other types of anchorage were not available. Moreover, orthodontic temporary anchorage devices (TADs) can be used both to maintain and to build bone. This paper may not have the typical structure of a scientific paper, but gives a realistic image of how progress occur and how casual observations can lead to the establishment of a research protocol and the results of an animal study can lead to a new clinical procedure.
Keywords
Over jet; Lower denture; Periodontologist; Zygomatic bone
Introduction
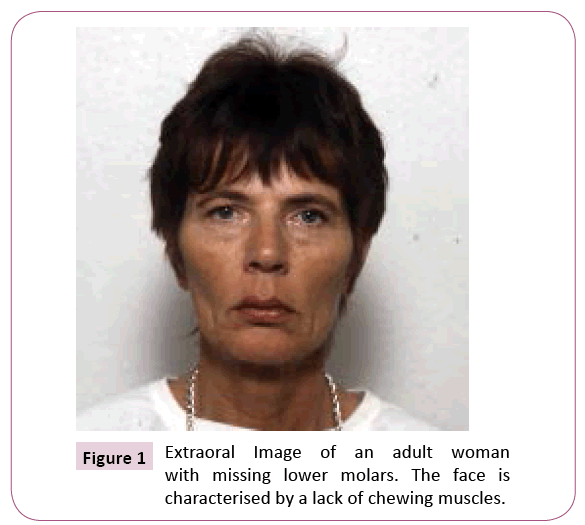
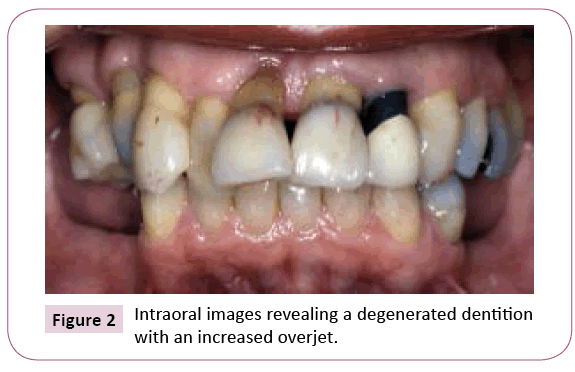
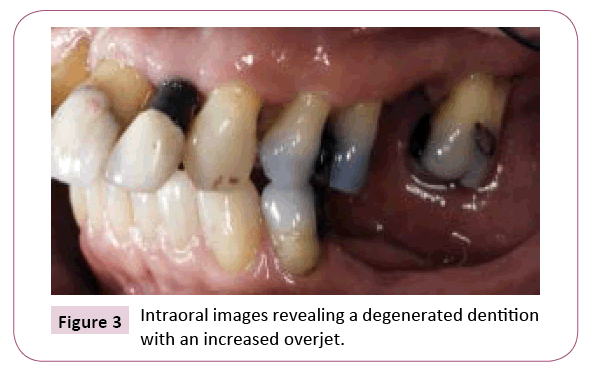
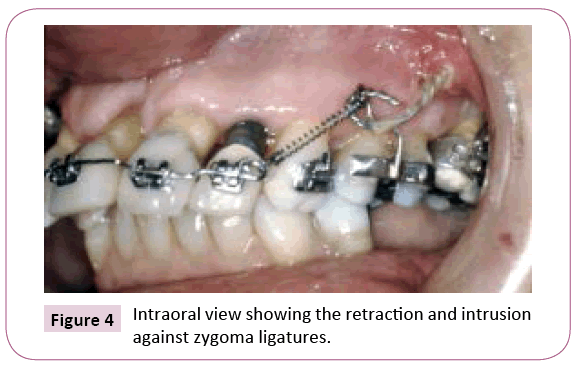
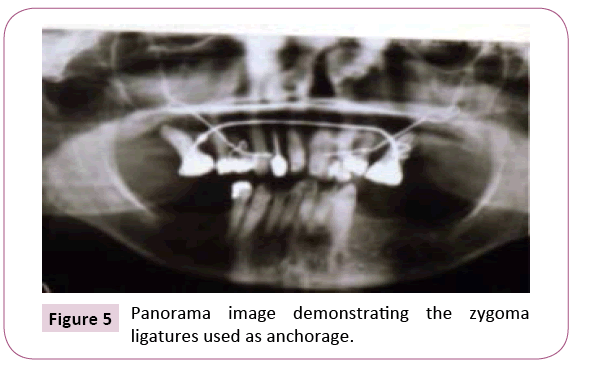
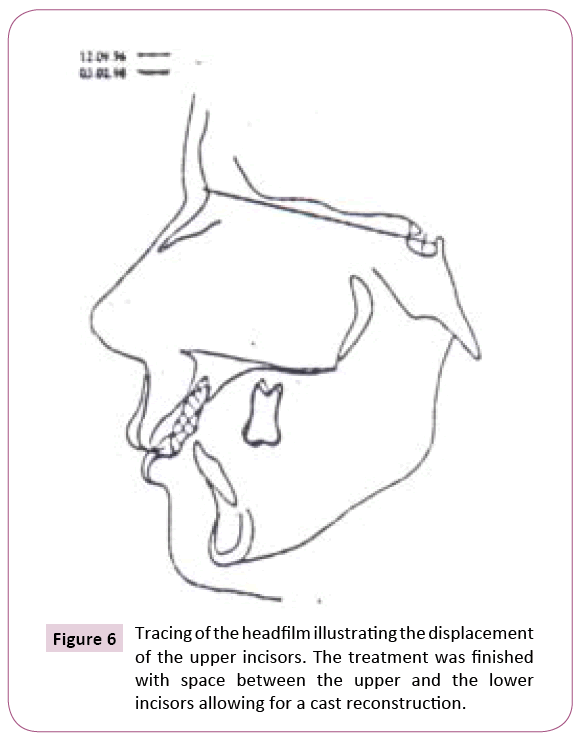
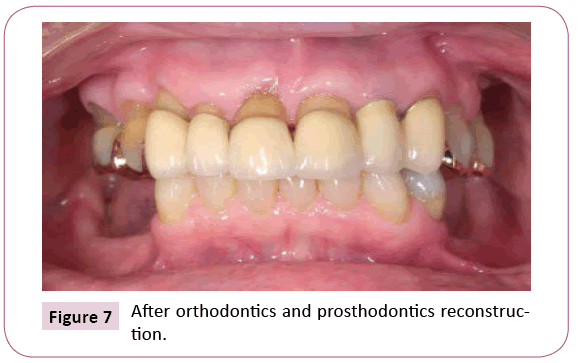
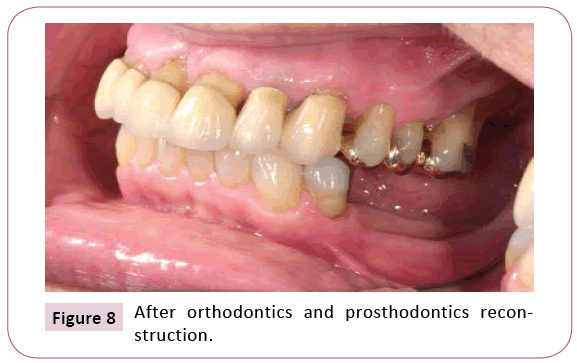
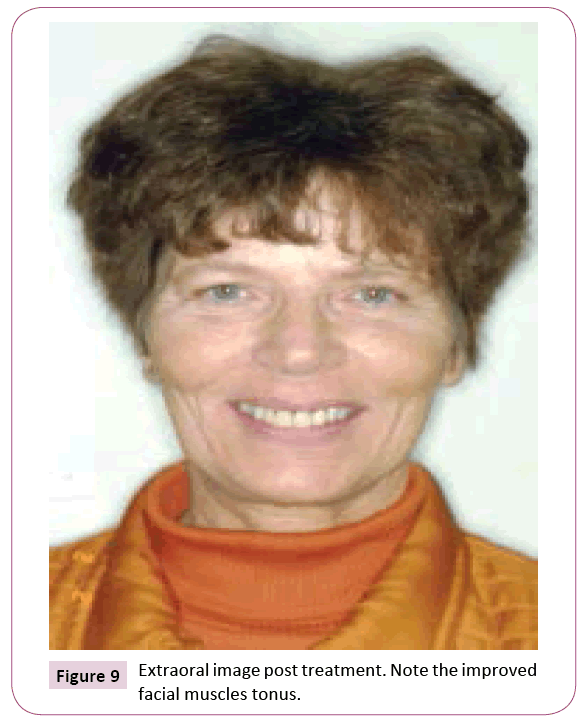
The progress of most disciplines occurs when faced with a problem considered impossible to solve. This happened in 1974 when a periodontist presented with a patient with a significantly degenerated and reduced dentition. The 53-year-old female patient had lost a considerable number of posterior teeth distal to the first premolars and she was wearing a removable lower denture. In the upper arch the first molars and the second right premolar were missing. The right central and the second left incisor were endodontically treated and all upper incisors exhibited more than 50% loss of marginal bone (Figures 1-9). The patient’s chief complaint was an increasing overjet and the periodontist requested a reduction of the overjet and the overbite [1]. “There is not enough anchorage” was my answer, being the orthodontist. The periodontist replied that this was my problem and it was decided to insert a piece of surgical wire through a drilled hole in the infrazygomatic crest and to use it as anchorage for the retraction and intrusion of the upper front teeth. A 0.018” x 0.025” stainless steel wire connecting the anterior teeth was connected to the zygoma wires with a force of 50 cN. Immediate loading was chosen as it was anticipated that the wire would move through the bone. This was based on the assumption that the load would be concentrated on a minute area [2]. In 30 patients treated over 15 years, 5 ligatures became loose as they did migrate through the zygomatic bone [3]. Care therefore had to be taken in order to place the ligature as deep as possible into the key ridge, the infrazygomatic crest.
Figure 6: Tracing of the headfilm illustrating the displacement of the upper incisors. The treatment was finished with space between the upper and the lower incisors allowing for a cast reconstruction.
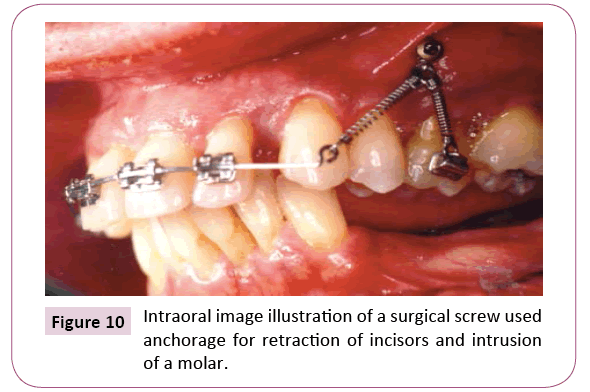
The next step in the development of skeletal anchorage occurred when a maxilla-facial surgeon (Dr. M. Raffaini) one day in the office of Dr. A. Costa had inadequate time scheduled to place the zygoma ligature and instead suggested to insert a surgical screw [4]. This was done on a patient who presented with an enlarged overjet due to flaring of the upper incisors as a consequence of aggressive periodontitis. Thus, a surgical screw was inserted into the infrazygomatic crest and served as anchorage for retraction and intrusion of the upper incisors on the left side while the occlusion was serving as anchorage on the right side (Figure 10). The idea of the surgical screw used as anchorage by Creekmore and Eklund [2] had been re-introduced.
Literature Review
Temporary anchorage devices (TADs) as anchorage
The surgical screws served as anchorage for retraction of upper teeth, and was used when conventional anchorage could not be applied. This was the case when there was a lack of anchorage teeth or when the effect of the force system on the anchorage unit was considered severely detrimental. Another indication would be when all teeth had to be moved in the same direction [5,6].
In the beginning the line of action of the force was the line between the “screw” and the teeth to be moved. However, the desired line of action of the force cannot always be generated between the active unit and the reactive unit, if for example the bone quality along the line of action of the force is not suited for the insertion of a “screw”. The solution may be the indirect application of the skeletal anchorage unit requiring a TADs with a bracket-like head. Thus, the screw can be inserted in an area, where the bone is adequate, and then be consolidated to a tooth, which then can serve as anchorage [7,8]. Another situation where indirect anchorage will be desirable is when the line of action of the force has to change during the progression of the treatment. This can be solved be placing the TADs in another localization or by using the TADs as indirect anchorage [9].
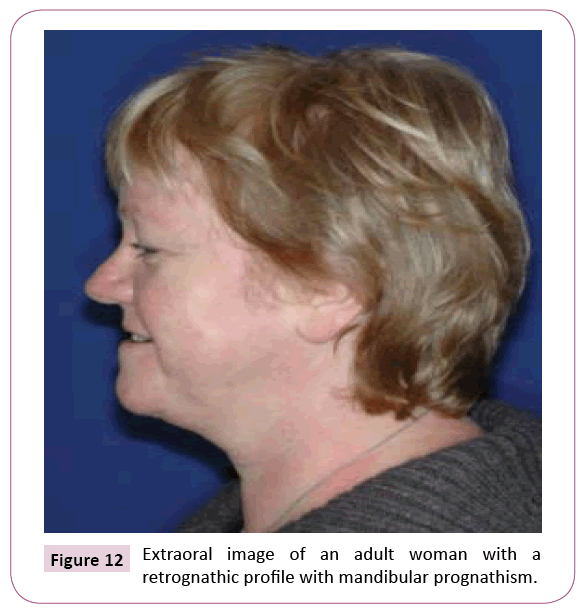
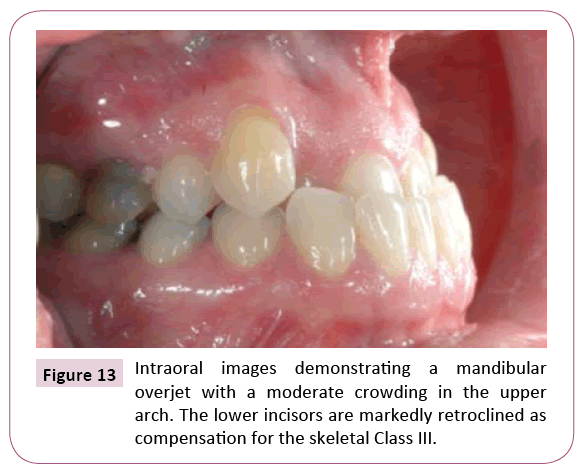
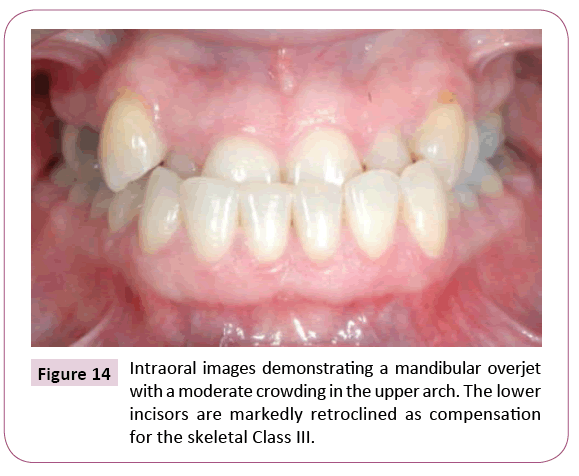
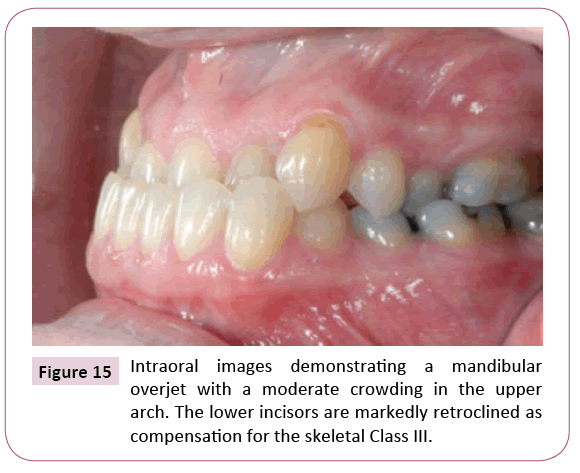
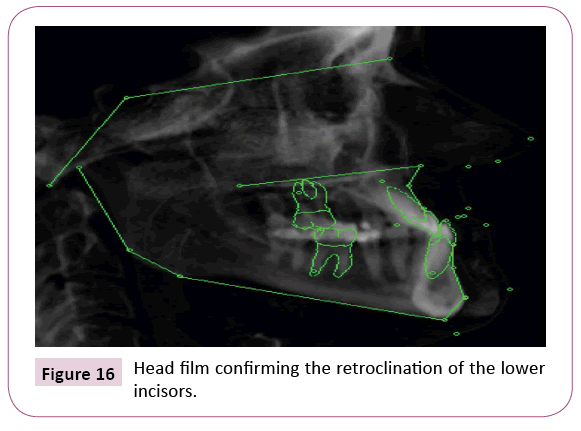
When the force needed is out of reach from both the TADs and the bracket, the desired resultant can be obtained by two vector mechanics [10]. One of these two force vectors may extend from a TADs. The patient presented in (Figures 11-15) presented with a mandibular overjet and moderate crowding in the upper arch. The CBCT image revealed a skeletal Class III and a correction of this malocclusion would customarily require surgery (Figure 16).
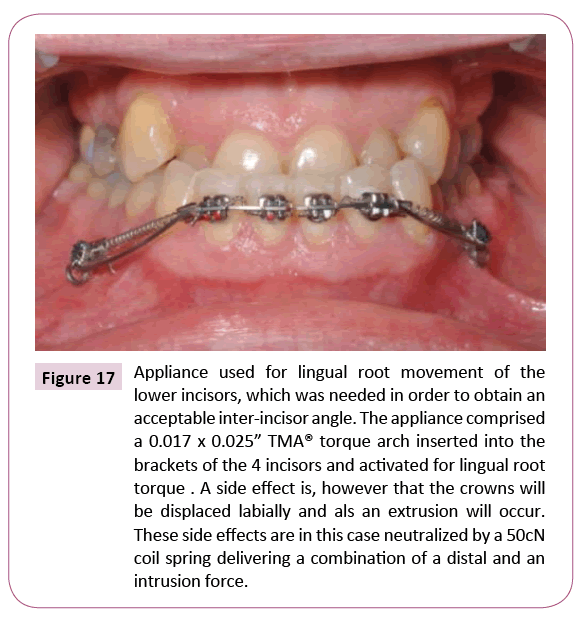
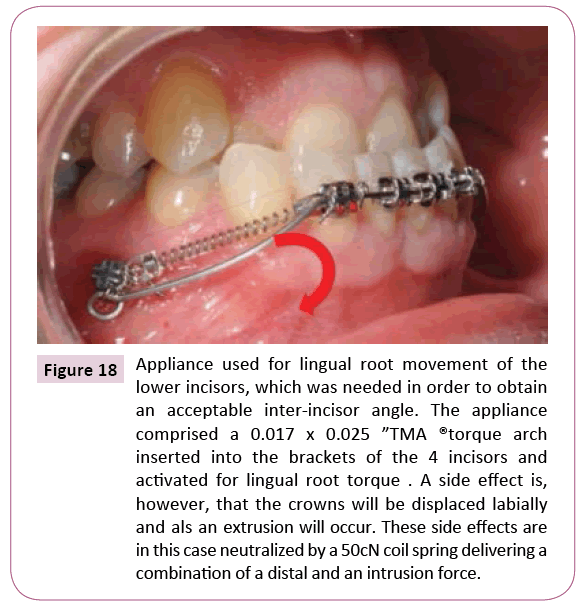
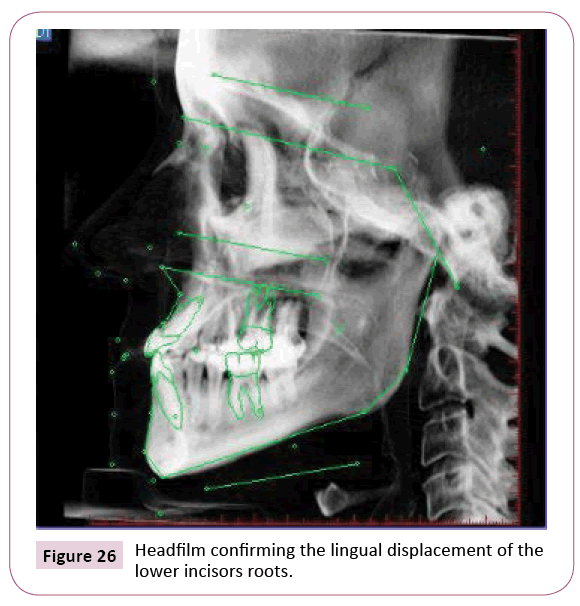
However, an orthognathic procedure was contraindicated due to health problems and it was decided to perform a dentoalveolar compensation in the upper arch and to correct the retroclined lower incisors by moving the roots lingually in order to finish with a good interincisal relation. The needed root movement of the lower incisors required a lingually directed force vector close to the apex. Such a force vector cannot be generated directly, but could be the result of lingual root torque combined with a force that would neutralize the side-effects of the torque arch, labial crown movement and extrusion (Figures 17 and 18).
Figure 17: Appliance used for lingual root movement of the lower incisors, which was needed in order to obtain an acceptable inter-incisor angle. The appliance comprised a 0.017 x 0.025” TMA® torque arch inserted into the brackets of the 4 incisors and activated for lingual root torque . A side effect is, however that the crowns will be displaced labially and als an extrusion will occur. These side effects are in this case neutralized by a 50cN coil spring delivering a combination of a distal and an intrusion force.
Figure 18: Appliance used for lingual root movement of the lower incisors, which was needed in order to obtain an acceptable inter-incisor angle. The appliance comprised a 0.017 x 0.025 ”TMA ®torque arch inserted into the brackets of the 4 incisors and activated for lingual root torque . A side effect is, however, that the crowns will be displaced labially and als an extrusion will occur. These side effects are in this case neutralized by a 50cN coil spring delivering a combination of a distal and an intrusion force.
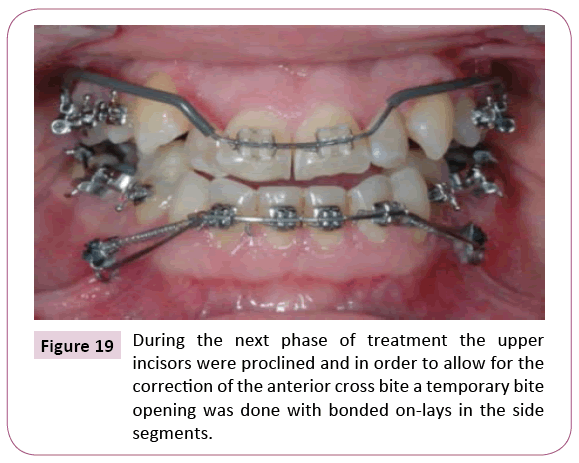
This force was generated by a closed coil spring extending from the incisor crowns to a TADs inserted between the roots of the two premolars. The coil-spring delivered 50 cN lingual and intrusion force thereby neutralizing the extrusion and buccal force from the torque arch which was also anchored to the TADs and thereby not delivering any undesired forces to the reactive unit. The effect of the appliance was monitored according to tooth movement observed. In the upper arch, a moderate expansion was obtained transversally with a quad helix and sagittally as a proclination delivered with a 0.017 x 0.025” TMA utility shaped base arch (Figure 19).
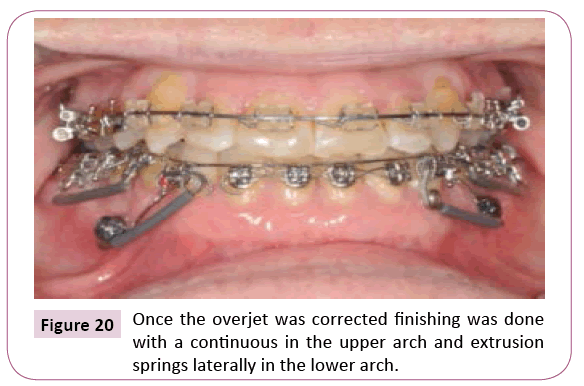
The finishing was performed with continuous arches (Figure 20).
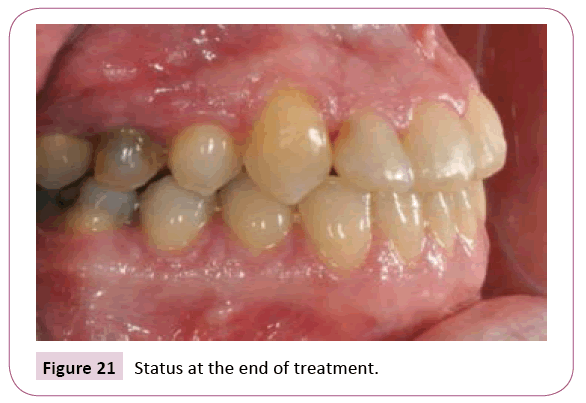
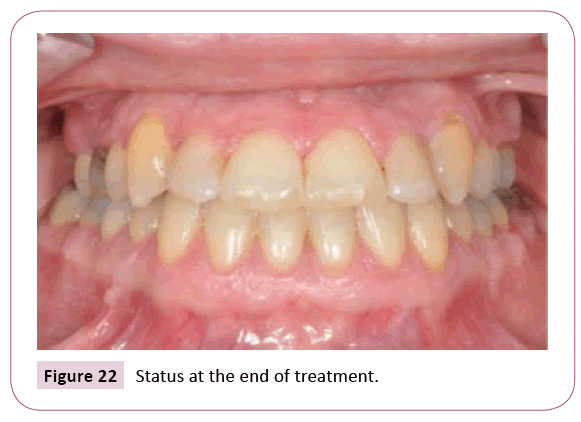
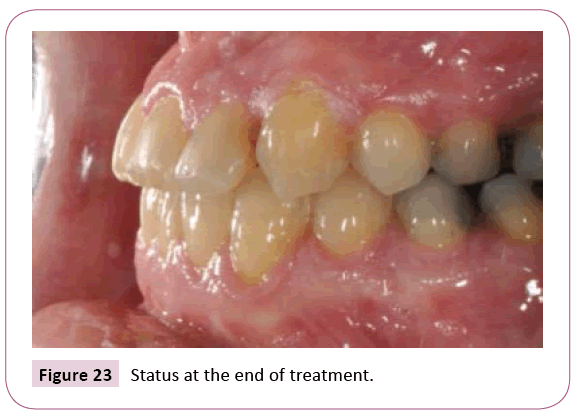
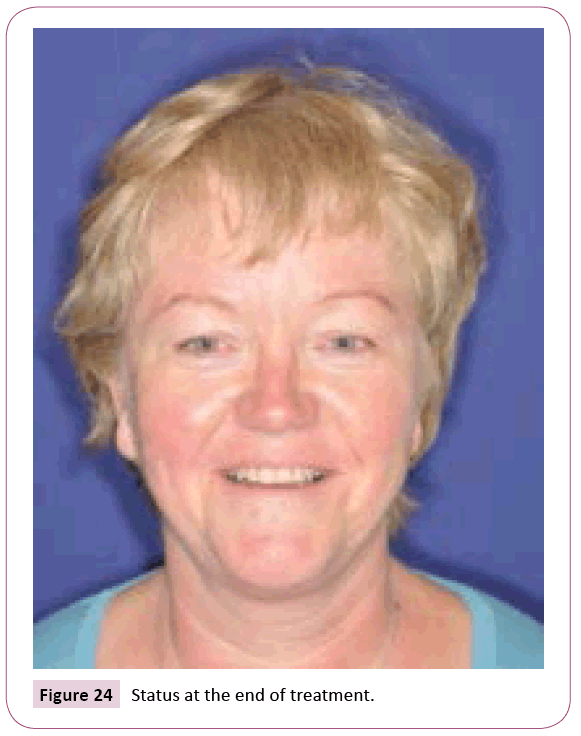
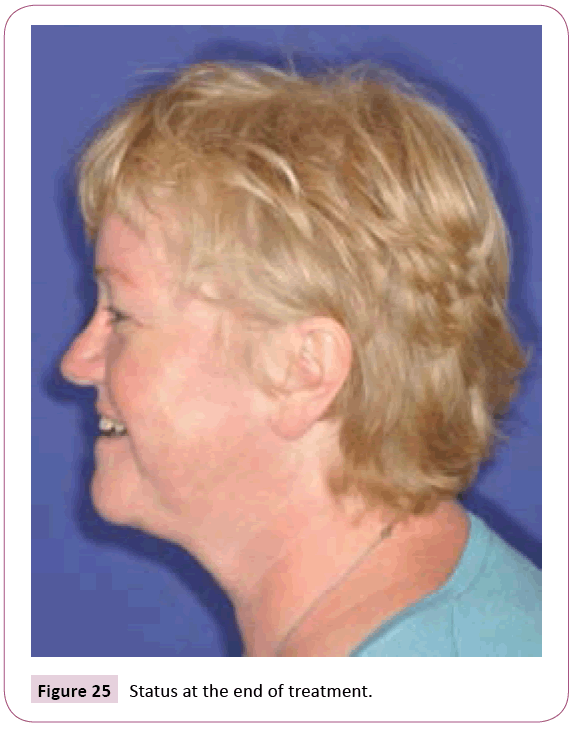
When the treatment result was analysed on the CBCT it was clearly demonstrated that the lingual root torque of the lower incisors had been obtained resulting in an improved inter-incisor inclination (Figures 21-26).
Building bone
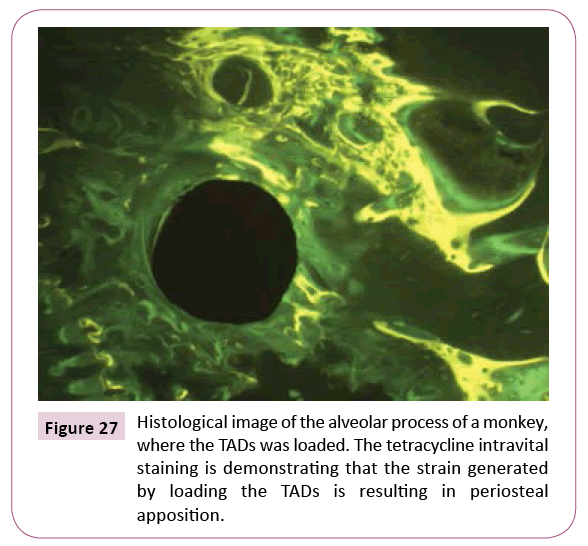
A different use of the TADs was a side product of a research with the purpose of describing the tissue reaction surrounding the screws with different coating. The histological analysis was performed on mini-implants coated with hydroxyl apatite, sandblasted or polished. They were inserted in the alveolar process of adult male macaca monkeys and observed for 12 weeks. It was found that all three types of TADs were osseo-integrated, but also that the bone density was increasing with time. The later was in contrast to what was originally described by the authors [11]. This can, however, be explained by the fact that the four monkeys involved in the study were pooled in the statistical comparison. When the bone density of the individual monkeys was compared there was a very large standard deviation as the bone turnover of the four monkeys were significantly different. This corroborated the results by Pilon et al. [12] that the individual pattern of bone turnover may overrule the effect of the externally added factors. The intravital staining with tetracycline and calcein evaluated histomorphometrically further demonstrated that the bone adjacent to the “screw” was characterized by a high turnover. This confirmed the results described by Dietrich et al. [13], but also led to another discovery. When a “screw” was loaded with a force against a tooth, the tooth was displaced, but the strain generated resulted in a periosteal apposition, which contributed to a modelling of the alveolar surface (Figure 27).
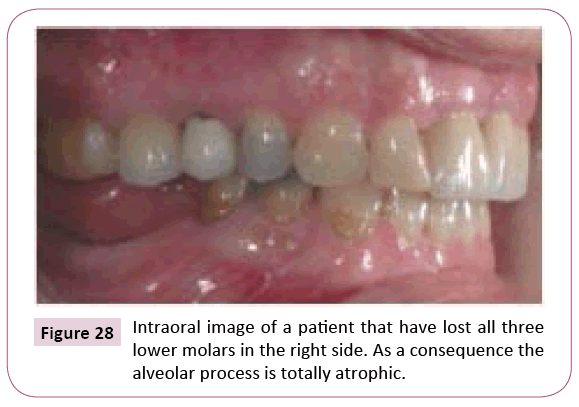
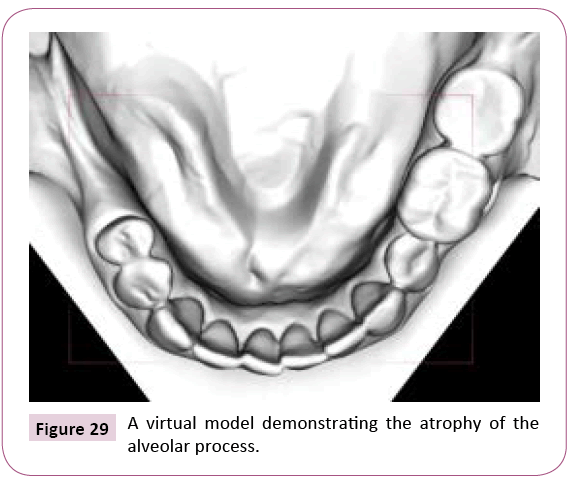
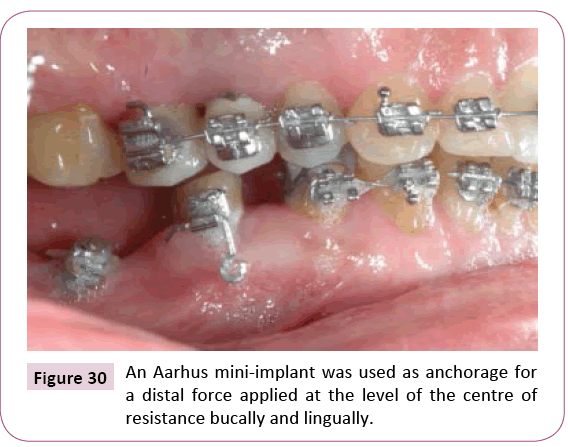
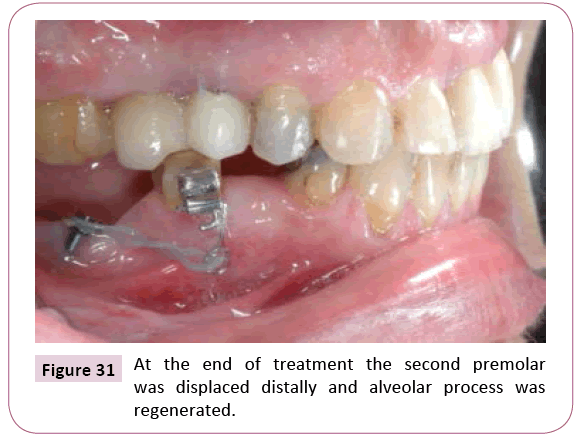
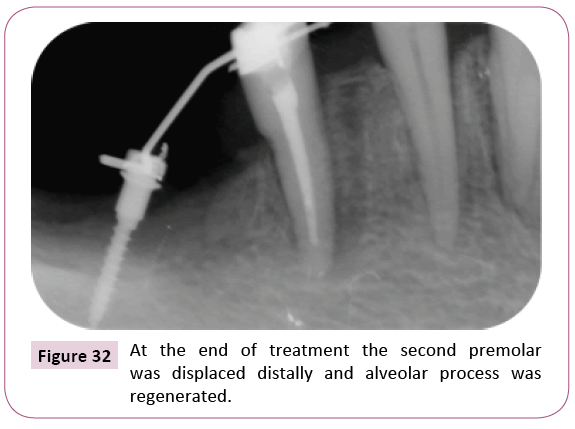
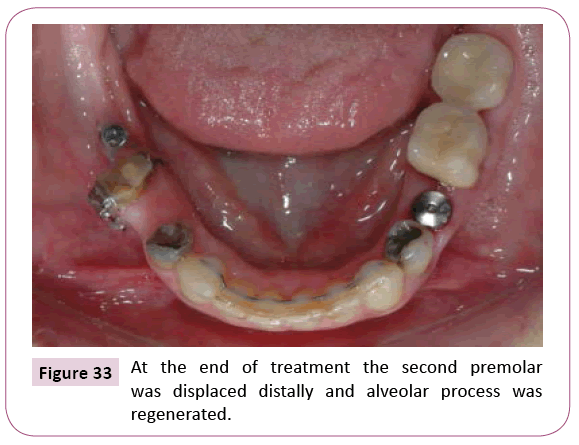
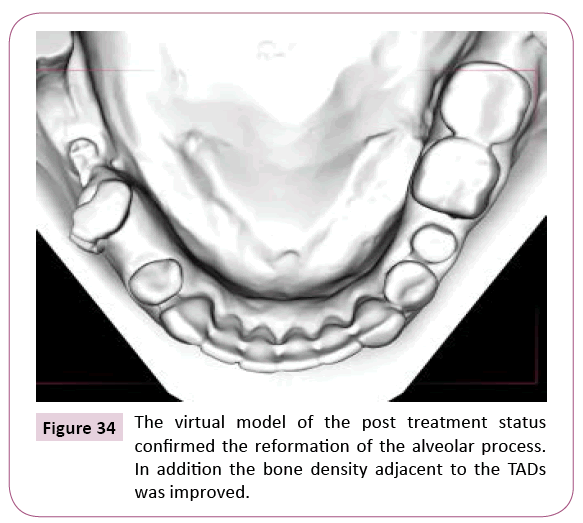
Tooth movement with the TADs as anchorage could also be performed with the purpose of regenerating an atrophic alveolar process. This was done in the treatment of a patient characterized by loss of all molars in the right side of the mandible (Figures 28-34). The alveolar process distal to the premolar was totally atrophic. A mini-implant was inserted on the anterior aspect of the ramus and a force at the level of the CR of the second premolar was generated between the TADs and the buccal and the lingual aspect of the first premolar. The premolar was translated distally and an implant site was thereby prepared between the second and the first premolar. The height and the width of the alveolar process was regenerated to a normal level.
Figure 29: A virtual model demonstrating the atrophy of the alveolar process.
Figure 34: The virtual model of the post treatment status confirmed the reformation of the alveolar process. In addition the bone density adjacent to the TADs was improved.
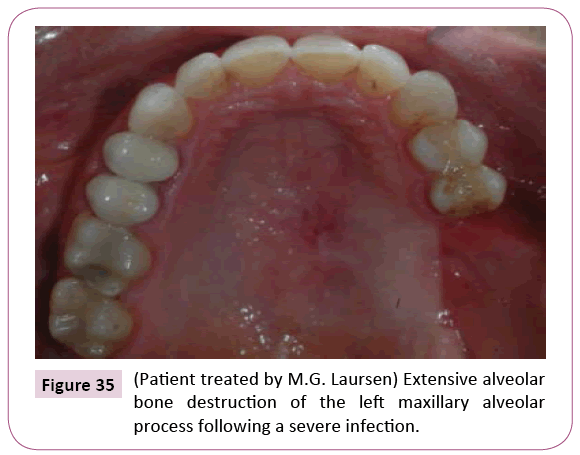
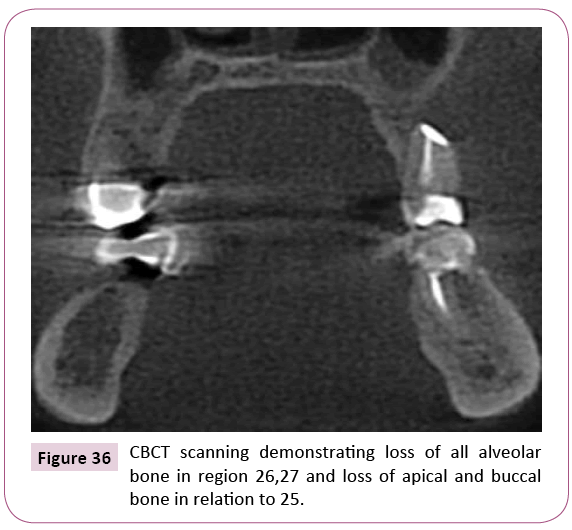
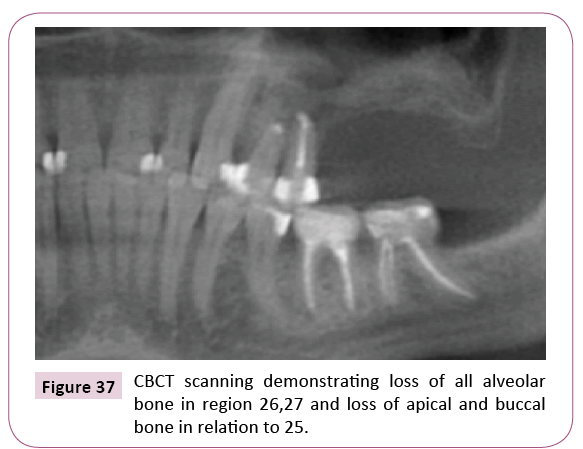
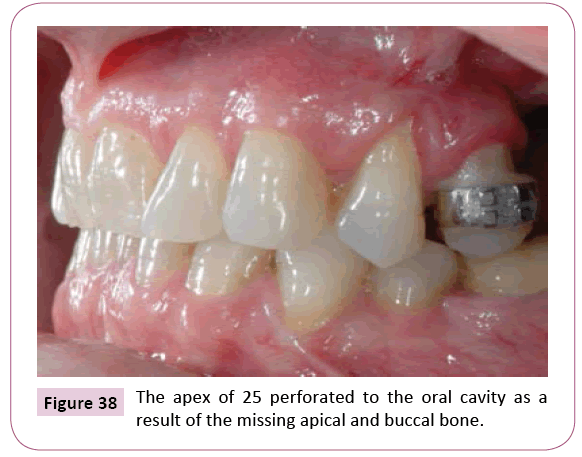
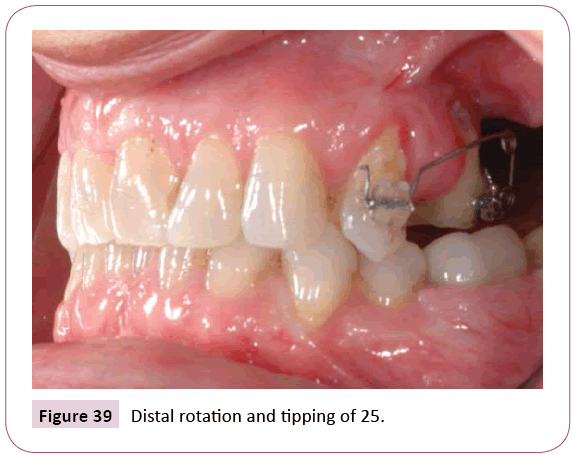
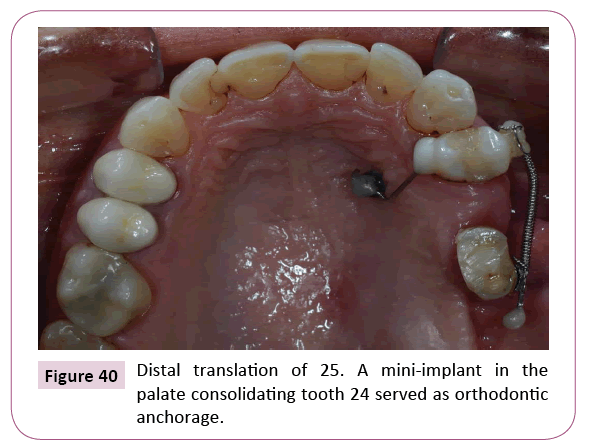
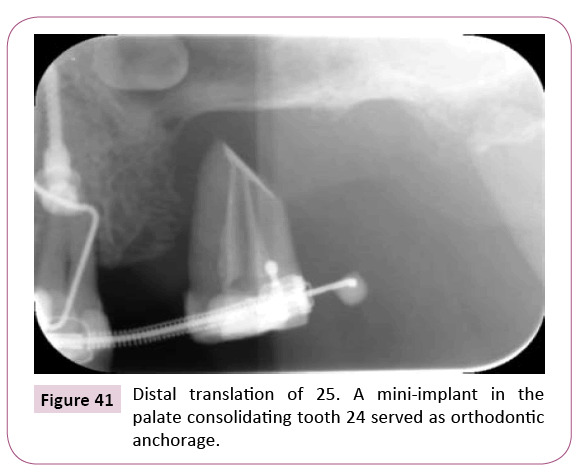
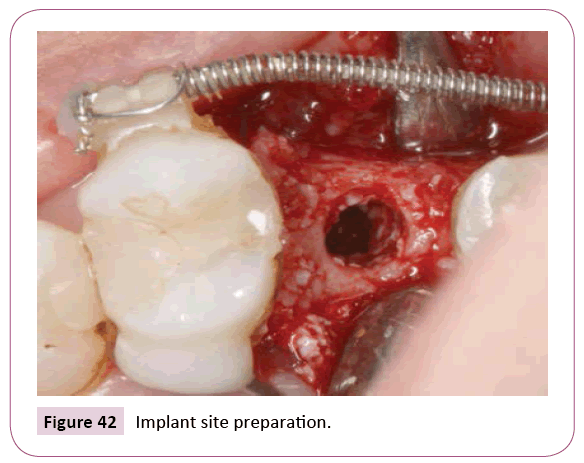
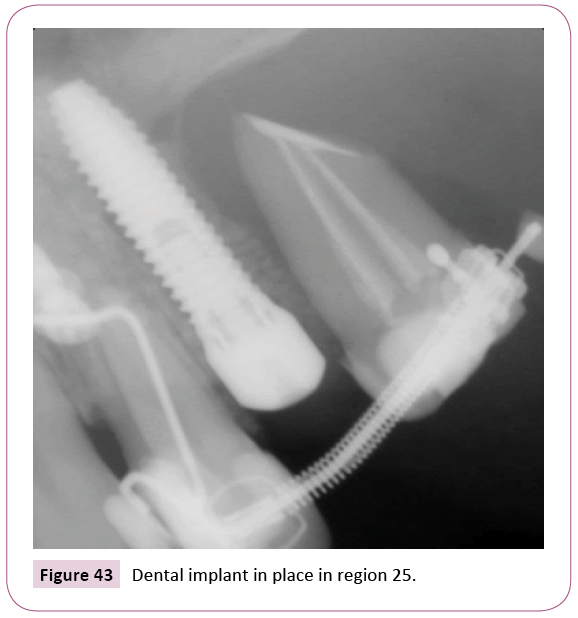
The loss of alveolar process was also the problem in the female patient aged 40 years (Figures 35-43). She was presenting with a total loss of the alveolar process distal to the left second premolar following a pathological process in the region. The apex of the second premolar perforated to the oral cavity as a result of the missing apical and buccal bone. The prognosis of the tooth was therefore very poor and the loss of the premolar would lead to extensive bone loss also in the second premolar region. The insertion of a dental implant in the region was considered impossible without extensive surgical bone augmentation. An orthodontic treatment plan was therefore established. It was decided to perform a distal rotation and distal translation of the premolar and thereby building bone for a single tooth implant replacing the second premolar. In the first phase of treatment a cantilever spring generated a distal rotation and tipping of the second premolar in order to build sufficient bone at the buccal aspect of the alveolar process. Light forces were used to perform tooth movement “with bone” and the crown of the second premolar was reduced to avoid occlusal interferences. After sufficient distal rotation an up righting of the second premolar was performed and a minor distal translation was produced with a light open coil spring on a passive 0.018 x 0.022 SS segment. A mini-implant placed in the palate consolidated the first premolar, which served as anchorage for the orthodontic displacement of the second premolar. At the end of orthodontic treatment sufficient bone for implant placement had been built although the remaining attachment of the second premolar was minimal. Before implant placement the implant site preparation was carefully probed and demonstrated a complete bony support without fenestrations of the walls.
TADs used for bone preservation
The above cases described how existing periodontium can be used in order to generate bone, but also that the density of the bone adjacent to the TADs in Figure 45 was increasing during the observation period.
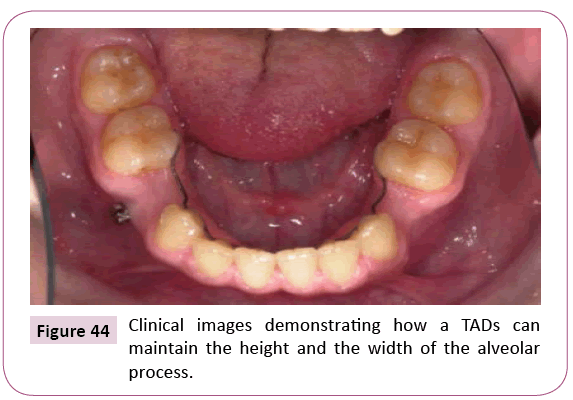
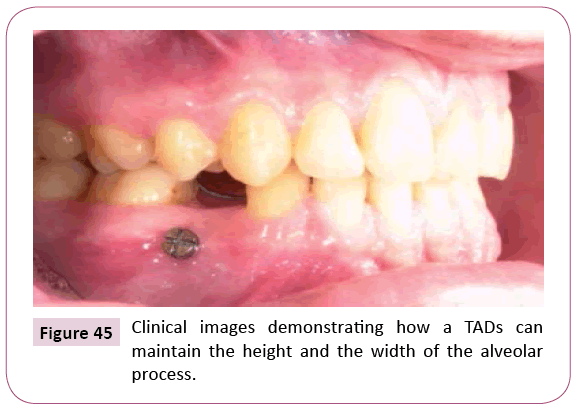
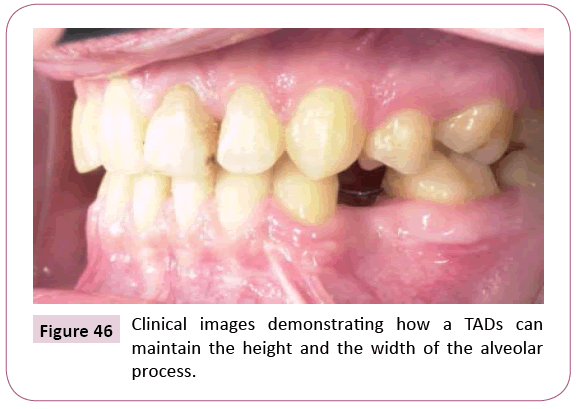
An unintended omission to remove one mini-implant which had served as anchorage in a patient with bilateral agenesis of premolars led to the formulation of the hypothesis that the presence of a mini-implant would prevent atrophy in edentulous areas (Figures 44-46).
In the side where a horizontally inserted TADs was left in place both the height and the width of the alveolar process was better than on the contralateral side. On the mini-implant side, the future insertion of a dental implant may be possible without any built-up procedure. This would, on the other hand be necessary on the contralateral side where a clear reduction in both width and height of the alveolar process had taken place following the loss of the deciduous molar.
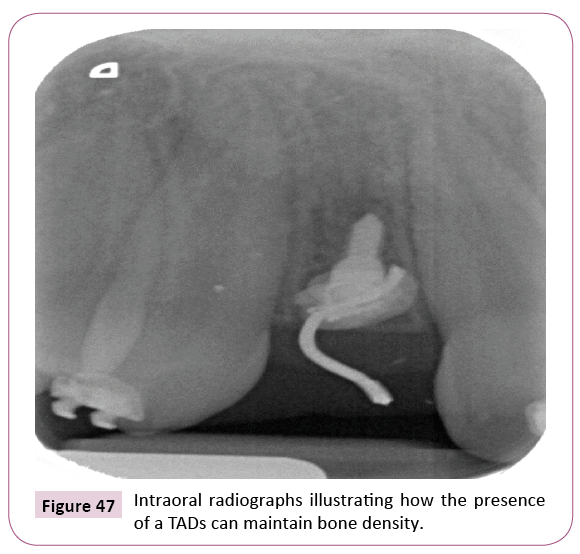
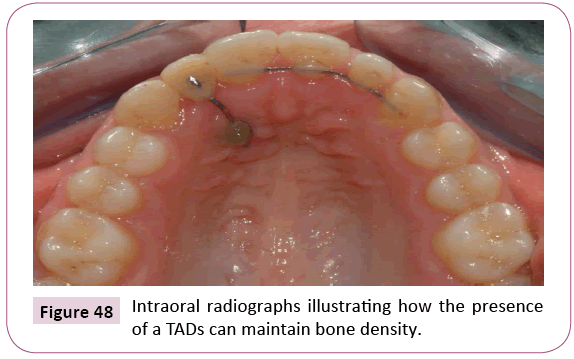
These findings were further supported by the observation of a patient with bilateral agenesis of maxillary second premolars and lateral incisors. It was decided to close the spaces for the premolars and maintain the spaces corresponding to the lateral incisors for later replacement with implants. To perform the mesial movement of the maxillary lateral segments it was necessary to apply a TADs as anchorage on the left side. A miniimplant was inserted horizontally in the alveolar process region 22. At the end of treatment, the intraoral radiographs revealed that the bone density in the region with the TADs was clearly higher that on the contralateral side (Figures 47 and 48).
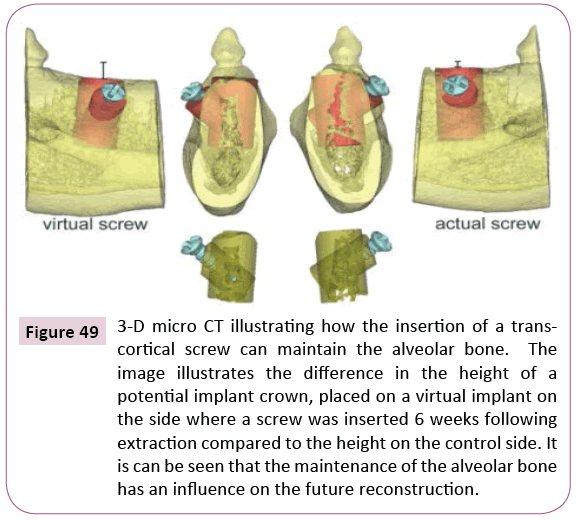
These two observations constituted the basis upon which the hypothesis tested in a dog experiment was made. The null hypothesis for this study [14] was that the presence of a miniimplant would maintain the alveolar bone in an extraction space. The study was carried out in a split-mouth design on 4 adult dogs. All dogs had 2 premolars extracted in each quadrant. After a healing period of 6 weeks self-drilling screws with a diameter of 1.5 mm were inserted horizontally bucco-lingually through each alveolus 2 to 3 mm below the alveolar crest on one side chosen at random, whereas the other side was left as control (Figure 49).
Figure 49: 3-D micro CT illustrating how the insertion of a transcortical screw can maintain the alveolar bone. The image illustrates the difference in the height of a potential implant crown, placed on a virtual implant on the side where a screw was inserted 6 weeks following extraction compared to the height on the control side. It is can be seen that the maintenance of the alveolar bone has an influence on the future reconstruction.
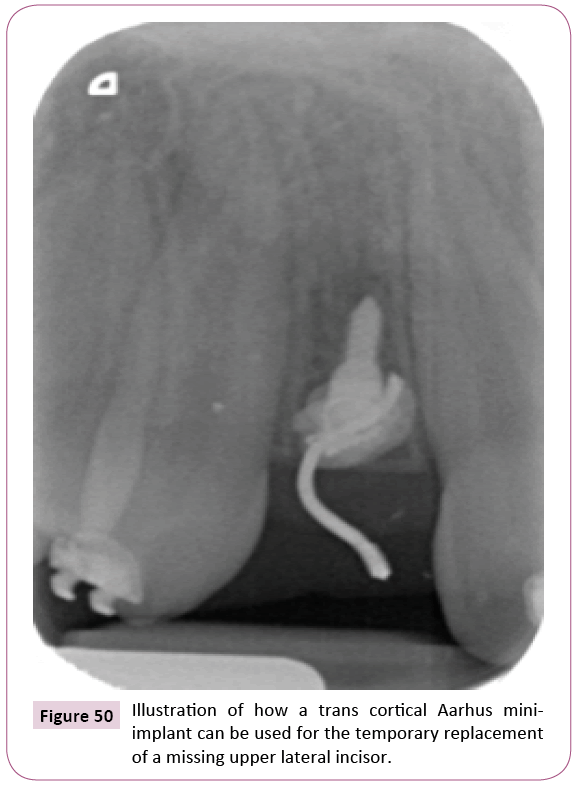
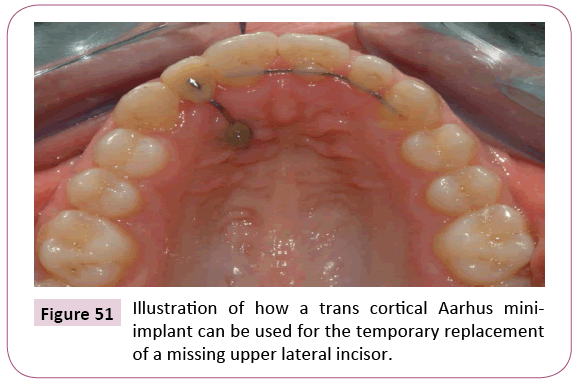
After 12 weeks, the dogs were sacrificed for excision of tissue blocks containing the alveolus with the regions of interest. Based on micro-CT scans the bone density surrounding the miniimplants were compared with bone density surrounding a virtual screw inserted in the same region on the contra-lateral side and corresponding to the extraction areas. In addition, the height of the alveolus on the side with the mini-implants was compared to that of the identical site on the contralateral side. The results confirmed the hypothesis that the existence of a screw had a positive influence on the maintenance of bone in edentulous areas. Based on these findings, it could be recommended that horizontal screws should be inserted when edentulous areas, which for various reasons e.g age or economy could not be treated with implant replacement. These findings were used by Ciarlantini, who inserted the Aarhus mini-implants in children with agenesis of lateral incisors (Figures 50 and 51). He did, however, combine the advantage of the bone preserving capacity and the fact that the mini-implants with a bracket head could support a temporary replacement of the lateral incisors and allow for the vertical development of the alveolar process [15-19].
Discussion
The introduction of the skeletal anchorage has to some degree revolutionized orthodontics and resulted in a large number of publications, of which according to a recent systematic review and meta-analysis only 14 publications fulfilled the requirement for quality research [17]. These studies confirmed that anchorage for en-masse retraction of maxillary incisors was more effective with TADs than with conventional methods. Another systematic review and meta-analysis assessed the effect of TADs on molar intrusion in patients with open bite and found that out of the 12 acceptable papers 6 reported molar intrusions while the others found no significant effect [18]. Due to the large number of confounders (patients related, user related, product related), the reviews will generally conclude that more quality research is needed. However, when the TADs are used only where other methods of anchorage cannot be applied and not as an alternative to other methods RCT’s the efficiency cannot be assessed.
The progress of orthodontics with TADs as discussed in this paper has been based on both ideas and findings during clinical practice and research. A single observation may open the way for progress and generate a foundation for research and evidence based practice. An excellent example of clinical relevant research is described in a meta-analysis comparing TADs and surgery for open bite treatments is. However, the scope of the present paper was not to assess the efficacy of TADs generally, but to illustrate how an event can widen the spectrum of orthodontics [19].
Conclusion
The temporary anchorage devices (TADs) have from the turn of the century received a wide spread interest primarily as anchorage for orthodontic tooth movements that could otherwise not be performed, but also as a mean to obtain a more compliance free appliance. The present paper has demonstrated how TADs can be used, not as an alternative to conventional anchorage, but as a mean to make it possible to perform treatments considered impossible, i.e. widen the spectrum of orthodontics. The TADs can serve as anchorage for the displacement of teeth into edentulous atrophic areas and thereby generate bone for the insertion of dental implants; they can serve as bone preservers and thus prevent atrophy of edentulous area, when the insertion of dental implants has to be postponed for various reasons and finally be used as semi-permanent replacements of missing maxillary lateral incisors.
This paper is built on a lecture presented for the CTorR with the purpose of demonstrating that it often is a clinical observation that leads to the development of a new treatment approach.
References
- Angle EH (1907) The treatment of malocclusion of the teeth. Philadelphia: White, S.S. pp. 1855-1930.
- Creekmore TD, Eklund MK (1983) The possibility of skeletal anchorage. J ClinOncol 17: 266-269.
- Melsen B, Petersen JK, Costa A (1998) Zygoma ligatures: An alternative form of maxillary anchorage. J ClinOncol 32: 154-158.
- Costa A, Raffaini M, Melsen B (1998) Miniscrews as orthodontic anchorage: A preliminary report. J ClinOncol 13: 201-209.
- Melsen B, Verna C (1999) A rational approach to orthodontic anchorage. Progress in Orthodontics 1: 10-22.
- Melsen B (2005) Mini-Implants: Where are we?J ClinOncol 39: 539-547.
- Melsen B, Verna C (2012) The adult orthodontic patient: More options than ever before! Adult Orthodontics. Chichester: Wiley-Blackwell, USA.
- Melsen B (2005) Temporary skeletal anchorage-the Aarhus anchorage system. In: Cope JB(ed) Temporary anchorage devices in orthodonticsunderdog media, LP, USA.
- Laursen MG, Melsen B (2009) Multipurpose use of a single mini-implant for anchorage in an adult patient. J ClinOrthod 43: 193-199.
- Fiorelli G, Melsen B, Modica C (2003) Two-vector mechanics. Prog Orthod 4: 62-73.
- Luzi C, Verna C, Melsen B (2009) Immediate loading of orthodontic mini-implants: Ahistomorphometric evaluation of tissue reaction. Eur J Orthod 31: 21-29.
- Pilon JJ, Kuijpers-Jagtman AM, Maltha JC (1996) Magnitude of orthodontic forces and rate of bodily tooth movement. An experimental study.Am J Orthod Dentofacial Orthop 110: 16-23.
- Wehrbein H, Diedrich P (1993) Endosseous titanium implants during and after orthodontic load--an experimental study in the dog. Clin Oral Implants Res 4: 76-82.
- Melsen B, Huja SS, Chien HH, Dalstra M (2015) Alveolar bone preservation subsequent to miniscrew implant placement in a canine model. OrthodCraniofac Res 18: 77-85.
- Ciarlantini R, Melsen B (2012) Miniscrew-retained pontics in growing patients: A biological approach. J ClinOrthod 46: 638-640.
- Ciarlantini R,Melsen B (2017) Semipermanent replacement of missing maxillary lateral incisors by mini-implant retained pontics: A follow-up study. Am J Orthod Dentofacial Orthop 151: 989-994.
- Antoszewska-Smith J, Sarul M, Lyczek J, Konopka T, Kawala B (2017) Effectiveness of orthodontic miniscrew implants in anchorage reinforcement during en-masse retraction: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 151: 440-455.
- Alsafadi AS, Alabdullah MM, Saltaji H, Abdo A, Youssef M (2016) Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: A systematic review Prog Orthod 17: 9.
- Greenlee GM, Huang GJ, Chen SS,Chen J, Koepsell T, et al. (2011) Stability of treatment for anterior open-bite malocclusion: A meta-analysis. Am J Orthod Dentofacial Orthop 139: 154-169.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences