Handwashing and Barrier Nursing to Prevent Neuro Intensive Unit Infections
Director, Nobel Institute of Neurosciences, Nobel Medical College and Teaching Hospital, Kanchanbari, Nepal
- *Corresponding Author:
- Iype Cherian, Director
Nobel Institute of Neurosciences
Nobel Medical College and Teaching Hospital
Kanchanbari, Nepal
Tel: +9779817243434
E-mail: drrajucherian@gmail.com
Received date: December 18, 2018; Accepted date: January 13, 2019; Published date: January 23, 2019
Citation: Cherian I, Burhan H (2019) Handwashing and Barrier Nursing to Prevent Neuro Intensive Unit Infections. J Health Hyg. Vol.3 No.1: 1.
Copyright: © 2019 Cherian I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: It is estimated that the highest incidence of nosocomial infections prevails in the intensive care units of hospital. Following strict nursing protocols such as proper handwashing before and after patient encounter and practicing barrier nursing can help prevent spread of infection in otherwise vulnerable patients. The aim of this study is to identify the importance of handwashing and barrier nursing protocol in prevention of nosocomial infections particularly in a neuro-intensive care unit. Methods: An observational study was conducted from May 2018 to October 2018. A total of 100 patients were observed for development of any infectious complication before (n=50) and after (n=50) implementation of handwashing and barrier nursing protocol. Results: The incidence of infectious complications in patients without handwashing measures was 26% vs 10% after handwash. The most common infection was Pneumonia (10%) followed by Bloodstream and wound site infections (7% and 6%, respectively). A clear decline in rates of infections was observed following implementation of handwashing protocol. Conclusion: Among other measures to prevent complications occurring in neuro-intensive care units, the incidence and spread of nosocomial infections can be decreased by adequate hand washing and barrier nursing protocols for the staff.
Keywords
Handwashing; Infection control; Neurointensive unit; Nosocomial infections; Nursing
Introduction
Hospital acquired infections are frequently associated with inpatient treatment and may cause a significant impact on prognosis if not treated in time. Of all the nosocomial infections, the highest incidence is seen in the intensive care units of most hospitals. The long duration of ICU days, prolonged use of catheters, drains and central lines, and mechanical intubation pose the greatest risk factors for such infections. It is estimated that on any given day, about 1 in 31 hospital patients has at least one healthcare-associated infection [1]. The consequent use of antibiotics causes unfavorable side effects and interactions, and most importantly, drug resistance for many organisms, hence it is important to prevent the incidence as well as spread of these infections for a favorable patient outcome. The implementation of infection control and disease prevention protocols aims to prevent the occurrence and spread of health-care associated infections. One of the simplest methods to practice infection control is to wash hands with soap and water before and after every patient interaction and use barriers like gloves, masks and caps to further prevent spread of disease. Nurses form the greatest proportion of health personnel worldwide, and attention is needed to play a greater role in delivering health services amidst a severe human resource for health crisis and overwhelming disease burden in low-income countries [2]. These protocols are often difficult to practise in low income countries, where patient burden is on the rise and healthcare facilities are below par. However, it is equally important to create awareness among healthcare providers regarding the efficacy of implementing handwashing and barrier nursing protocols in preventing infectious disease occurrence and spread in intensive care units.
Materials and Method
A prospective observational study was conducted at the 29- bedded Neuro-Intensive Care Unit (ICU) in Nepal. The study was conducted over a period of 6 months from May to October 2018. A total of 100 patients admitted in the Neuro-ICU were included, and divided into control and treated groups, 50 patients each. A protocol to implement infection prevention and control was established. All the healthcare staff was educated about steps of proper handwashing using soap and water before and after every patient interaction. Steps were taken to introduce the concept of “barrier nursing” by wearing gloves, face masks, head caps and ICU shoes within the restricted areas of the neuro ICU. No handwashing or barrier nursing was practised in the control group, in contrast to the treated group. Information regarding patient demographics and daily followups were used to record any infectious complication occurring in the patients. Data was analyzed using SPSS software and a chisquared test was run to assess any significant difference between the two groups.
Results
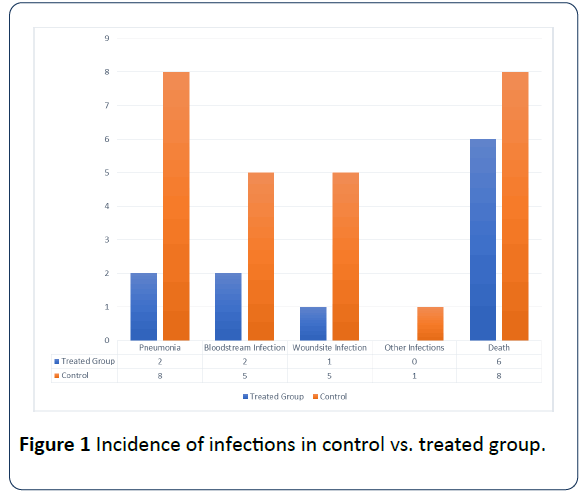
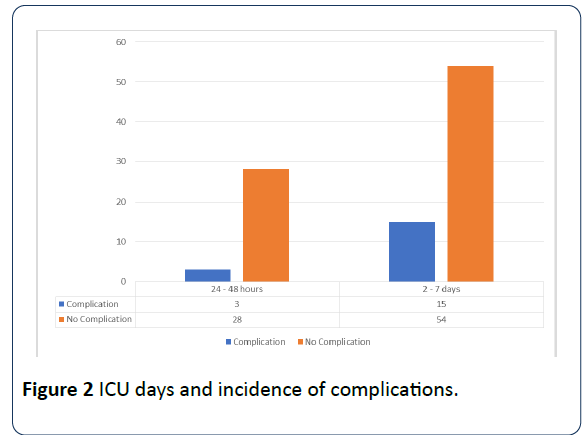
Among the patients, 48 were male and 52 females. Around 42% belonged to age group 25-40 years, followed by 15–25 years (31%), 40–60 years (20%), 0–15 years (5%) and only 2% patients aged 60 and above. Infectious complications in control group accounted for 26% (n=13) vs 10% (n=5/50) in the treated group. Among all the complications in both groups, pneumonia contributed to 10% (16% in control vs 4% in treated group), followed by bloodstream and wound infections (7% and 6%, respectively) and others (1%). The incidence of deaths in both the groups was almost same (16% control and 12% treated group) (Figure 1). A significant association was found between the duration of ICU stay and prevalence of pneumonia (p<0.005) (Figure 2).
Discussion
Health-care associated infections are a common part of hospital treatment. A recent survey by the CDC reports that about 1 in 31 hospital patients has at least one healthcareassociated infection. The close contact of a patient with his healthcare provider serves as a means of disease development and spread from one patient to another. Intensive care units are designed to strictly monitor critically ill or post-operative patients, where usually the immunity is low, providing a chance for opportunistic infections to develop in the setting. It is noteworthy that the majority of nosocomial infections are found in these intensive care units, and strict measures are needed to prevent the development and spread of such infections.
These healthcare-associated infections (HAIs) include central line-associated bloodstream infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia. Infections may also occur at surgery sites, known as surgical site infections.
Surveillance studies from multiple centers have concluded the prevalence of pneumonia to top the list of all nosocomial infections [3,4]. Another study to determine the causative agents for HAI concluded that the most common were the Entero bacteriaceae family members – 23 (32.4%), Pseudomonas aeruginosa – 14 (19.7%), Staphylococcus aureus – 11 (15.5%), including 10 (90.9%) MRSA isolates, Acinetobacter spp., mainly Acinetobacter baumannii – 11 (15.5%), Enterococcus spp. – 8 (11.3%), other gram-negative non-fermentative rods – 2 (2.8%), Streptococcus pyogenes – 1 (1.4%) and Candida parapsilosis – 1 (1.4%) [5].
The neuro-ICU population poses a specific challenge in the diagnosis of infections, because of the high incidence of fever in acutely brain-injured patients. Furthermore, susceptibility to infections is likely enhanced by brain-injury (induced immune modulation). Nosocomial meningitis and ventriculitis are a specific problem for the neuro-ICU population, largely linked to craniotomy and placement of central nervous system devices [6]. A recent large-scale surveillance study estimated the risks of HAI in neurocritical a rate of 10.9/1000 ICU days, with a majority being related to the use of devices such as catheters, ventilators, central line-associated blood stream infections and ventriculostomy. Prolonged neuro-ICU length of stay (more than 48 hours) was strongly associated with all HAIs similar to the results observed in our study.
The situation is much worse in low income countries where healthcare facilities as not well equipped to implement infection control protocols even in tertiary care hospitals. The fact that healthcare associated infections can be prevented makes it even more important to take steps for disease prevention and control. It is important to start from the basic rather than developing sophisticated methods to achieve a disease-free environment. The global initiative of the WHO on patient safety programs is based on the agenda “Clean Care is Safer Care”. With this awareness and undisputed evidences, it is time for developing countries to formulate the much-needed policies for implementation of basic infection prevention practices in health care set-ups. Hand hygiene, or hand-washing is perhaps the simplest and low-cost way to reduce the risk of crosstransmission of infections prevent the spread of infections, despite which, it is least practiced by many healthcare providers. On average, healthcare providers clean their hands less than half of the times they should. On any given day, about one in 25 hospital patients has at least one healthcare-associated infection. Several studies have demonstrated that handwashing virtually eradicates the carriage of MRSA which invariably occurs on the hands of HCPs working in ICUs [7]. The hand hygiene liaison group identified nine controlled studies, all of which showed significant reductions in infection related outcomes, even in settings with a high infection rates in critically ill patients [8]. It is important to educate the healthcare providers, particularly in the neuro-intensive units when and how to properly wash their hands.
Another method to achieve infectious disease prevention is barrier nursing to protect medical staff against infection by patients and also protect patients with highly infectious diseases from spreading their pathogens to other non-infected people. This technique provides maximal isolation care, while also preventing the disease from spreading while care is being provided. Simple barrier nursing consists of utilizing sterile: gloves, masks, gowns, head-covers and eye protection [9]. A much rigid barrier nursing in more catastrophic case involves further use of air-locking systems and wearing of personal protective equipment to ensure strict protection from any contagious infection.
Barrier nursing has been shown to be accepted by most patients in a very positive manner as they feel content with the level of care and privacy being provided to them. On the other hand, it does compromise the quality of emotional support for the patient and may aggravate the social stigma of isolation within the patient [10]. Nevertheless, it is desirable to provide optimum care for best patient outcome, which could otherwise deteriorate with the prevalence of nosocomial infections, particularly in critically-ill patients.
Conclusion
The results clearly indicate that a shorter duration of ICU stay along with the implementation of hand hygiene and barrier nursing practices can decrease the incidence of nosocomial infections in neuro-intensive care patients. Practicing hand hygiene and barrier nursing is a simple yet effective way to prevent infections.
References
- CDCP (2018) Current HAI Progress Report. Centers for Disease control and prevention website.
- Ng'ang'a N, Byrne MW (2015) Professional practice models for nurses in low-income countries: an integrative review. BMC Nurs 14: 44.
- Dettenkofer M, Ebner W, Els T, Babikir R, Lucking C, et al. (2001) Surveillance of nosocomial infections in a neurology intensive care unit. J Neurol 248: 959-964.
- Dasgupta S, Das S, Chawan NS, Hazra A (2015) Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med 19: 14-20.
- Kozlov R, Ratchina S, Mishchenko V, Sukhorukova M, Kretchikova O, et al. (2012) Spectrum of causative agents of nosocomial infections (NI) and their susceptibility to antimicrobials (AM) in multiward clinical hospital: results of one-year surveillance study. International Journal of Infectious Diseases 16: e422.
- Busl KM (2017) Nosocomial Infections in the Neurointensive Care Unit. Neurol Clin 35: 785-807.
- Peacock JE, Marsick FJ, Wenzel RP (1980) Methicillin resistant Staphylococcus aureus; introduction and spread within a hospital. Ann Intern Med 93: 526-532.
- Stone SP (2001) Hand hygiene: the case for evidence-based education. J R Soc Med 94: 278-281.
- Landers T, McWalters J, Behta M, Bufe G, Ross B, et al. (2010) Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs 66: 2309-2319.
- Barratt R, Shaban R, Moyle W (2010) Behind barriers: patients' perceptions of source isolation for Methicillin resistant Staphylococcus aureus (MRSA). Australian Journal of Advanced Nursing 28: 2.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences