Familial Aggregation of Hypospadias in South Indian Population
JN Medical College, KLE Academy of Higher Education and Research Belagavi, Karnataka, India
- Corresponding Author:
- Rajendra B Nerli
JN Medical College
KLE Academy of Higher Education and Research Belagavi
Karnataka, India
E-mail: rbnerli@gmail.com
Received Date: June 29, 2018; Accepted Date: July 20, 2018; Published Date: August 10, 2018
Citation: Rajendra BN, Shridhar CG, Shivayogi EN, Murigendra BH, Neeraj SD (2018) Familial Aggregation of Hypospadias in South Indian Population. Res J Congenit Disease Vol. 1 No. 2:2.
Copyright: © 2018 Rajendra BN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Hypospadias is one of the most common birth defects in male. However, its etiology remains largely unknown. Several authors have investigated the contribution of genetic and environmental factors to familial aggregation of hypospadias. We retrospectively analyzed our hospital data for boys who were operated for hypospadias at our center and had relatives with hypospadias.
Materials and Methods: We retrospectively reviewed the records of 234 children ( 18 yrs.) admitted for surgical correction of hypospadias at the department of pediatric urology in a single tertiary care centre of South India, from Jan 2007 to Dec 2017.
Results: During the 10 year study period a total of 234 children (≤18 yrs.) were operated for hypospadias. Twenty one (9%) children reported on additional members of the family having hypospadias.
Conclusions: Nine percent of the children operated for hypospadias reported on additional members of the family having hypospadias. These findings underline the heavy influence of genetic factors on hypospadias development. Genetic factors could be responsible for a certain percentage of cases of hypospadias.
Keywords
Hypospadias; Family; Genetics; Hypospadias; Inheritance patterns
Introduction
Hypospadias is a congenital disorder characterized by an incomplete fusion of the urethral folds, which results in the urethra opening on the ventral aspect of the penis [1]. It is a common congenital problem, affecting approximately 2-8 per 1,000 live births [2]. A number of surveillance programs have registered an increase in the prevalence of hypospadias [3,4]. In Denmark and Sweden, a temporal increase was observed after initializing registration of hypospadias in the 1970s; however, prevalence has been stable since the beginning of the 1980s [4,5]. Therefore several experts believe that this increase may be due to ascertainment bias.
The etiology of hypospadias to a large extent remains unknown. Observations from families with a monogenic inheritance of hypospadias, the presence of hypospadias in several genetic syndromes as well as an association with genetic defects in androgen biosynthesis and function, speak in favor of a genetic background [1,6]. However, less than 5 percent of all cases of hypospadias may be associated with such conditions [1]. In addition to a family history of hypospadias, only a few risk factors associated with hypospadias have been found, for example, paternal subfertility, low birth weight, and intrauterine growth retardation [7-9]. In spite of strong evidence for a genetic component being involved in the etiology of hypospadias, the exact mode of inheritance has not been well delineated.
Fredell et al. [10] analyzed 2503 boys operated for hypospadias regarding familial aggregation. Of these 7% reported 1 or more additional family members with hypospadias. There were 50% more twins than expected compared to the general population and established zygosity in 83% (67% monozygotic, 33% dizygotic). The authors concluded that finding of additional members with hypospadias in 7% of the families supported the concept that genetic factors were involved in the pathogenesis. We retrospectively analyzed our hospital data for children operated for hypospadias at our center and had relatives with hypospadias.
Methods and Materials
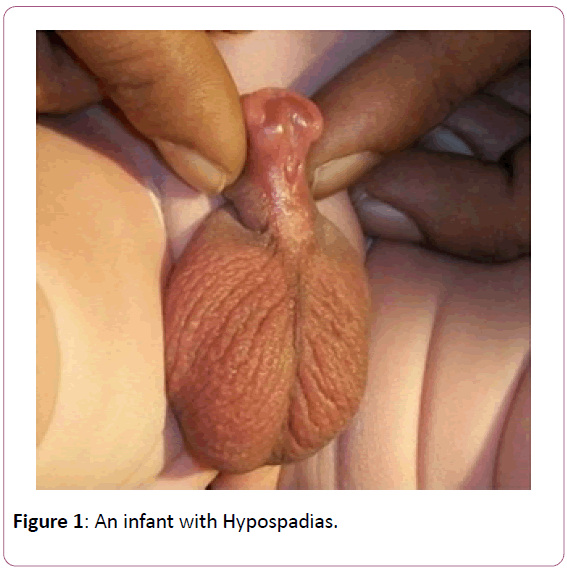
We retrospectively reviewed the records of 234 children ( 18 years) admitted for surgical correction of hypospadias at the department of pediatric urology from Jan 2007 to Dec 2017. All these index patients and their parents were questioned at admission/follow-up for additional family members with hypospadias (Figure 1). All patients who reported relatives with hypospadias were inquired in detail regarding the pedigree. In this present study familial cases were defined as patients with 1 or more first, second or third- degree relatives with hypospadias.
All the children presenting for surgery and the relatives with hypospadias were questioned and examined for other congenital malformations and previous surgeries. The severity of hypospadias was assessed in all of them.
Results
During the 10 year study period a total of 234 children ( 18 yrs.) were operated for hypospadias. Twenty one (9%) children reported one or more family members having hypospadias (Table 1). The mean age of the children at the time of surgery was 11.8 years.
| Degree of Relationship | No. of Patients (%) | Cases with more than one affected relative (%) | |
|---|---|---|---|
| 1 | First degree | 16 (76.19) | 4 (19.04) |
| 2 | Second degree | 4 (19.04) | 1 (4.76) |
| 3 | Third degree | 1 (4.76) | - |
Table 1: Incidence of hypospadias in relatives based on the degree of relation.
Of the 16 children having a first degree relative with hypospadias, ten were siblings and the remaining six were fathers of the index child. Four of these children had more than one family member with hypospadias. One child had two younger siblings (15 and 13 years old) with hypospadias. This child approached us for repair at the age of 17 years and reason for delay in treatment was poverty and ignorance. Another child (15 yrs.) was brought to us with history of not attaining menarche. On examination this child had external genitalia appearing like that of a female child and hence the child was wrongly labelled as female at the time of birth. On evaluation it was discovered that this child had a 46XY chromosomal pattern with bilateral undescended testes. This child had a younger sibling (9 yrs.) with severe hypospadias and a first cousin (11 yrs.) also with severe hypospadias. Four children had cousins (second degree) with hypospadias and one child had a cousin uncle (third degree) with hypospadias.
Seven children with hypospadias were born out of consanguineous marriage. All these children had severe form of hypospadias (proximal penile, scrotal, perineal). All the 16 children with first degree relative having hypospadias had proximal hypospadias and their relatives too had proximal hypospadias.
Discussion
Hypospadias refers to a urethral opening proximal to the normal glanular position. Hypospadias is diagnosed by physical examination. Typically preputial development is asymmetrical, with a dorsal “hood” and ventral deficiency that exposes the glans and proximal meatus [1]. Several birth registries have suggested an increasing prevalence in the 1990s, possibly linked to environmental toxins, but changes in reporting criteria and accuracy of the diagnosis potentially account for these observations. Three case-control studies of births in Denmark, France, and Italy reported prevalence of hypospadias in 0.3% to 0.45% of male births. The relative risk for recurrence in firstdegree relatives was 13 times greater, found in 9% to 17% of brothers and 1% to 3% of fathers. Risk in same-sex twins was 50%. Recurrence risk in offspring was the same as in first-degree relatives [10-12].
Schnack et al. [11] in their study documented familial aggregation of hypospadias within male twin pairs and first, second, and third-degree relatives. These findings extended previous suggestions that related to the impact of familial aggregation on the development of hypospadias and underlined the significant contribution of genetic inheritance to the development of familial hypospadias. The inheritance appeared to be transmitted equally through the paternal and maternal sides of the family. Similarly several authors have reported about familial aggregation ranging from 4 to 25% of cases of hypospadias [13]. A few families show an autosomal dominant inheritance pattern for hypospadias [13], whereas in ethnic groups with a high degree of consanguinity a recessive mode of inheritance can be observed [13].
It is well recognized that clustering of hypospadias occurs in some families and it is the male relatives of an index male child that are more likely to have this condition. In a study reported by Sorenson [14], 28% of the 103 index cases had at least one other family member with hypospadias. The more severe the hypospadias in the index case, the higher the incidence of hypospadias in a 1st degree relative. Bauer et al. [15] reported that in their series of 307 cases, 25% of the families had a second family member, in addition to the index child, with this anomaly and 7% had 3 affected members. No child with mild or distal hypospadias had a brother with hypospadias. This familial clustering of hypospadias does not suggest a Mendelian pattern of inheritance, and a multifactorial pattern seems to be most consistent explanation [16]. Allelic variants in genes involved in androgen production and metabolism may individually produce small risks that are not in themselves sufficient to produce hypospadias. When genetic susceptibility is combined with exposure to anti-androgenic agents, risk factors surpass a threshold, resulting in occurrence of this birth defect [17].
A familial aggregation speaks in favor of genetic involvement in the pathogenesis of hypospadias. Hypospadias is also a part of more than one hundred genetic syndromes [13]. Several single gene traits can cause this malformation, including the partial androgen insensitivity syndrome, testosterone 5-∝ reductase deficiency and Drash syndrome [18]. Fredell et al. [16] analyzed a large group of patients with hypospadias regarding familial aggregation, phenotype, twin rate and ethnic origin and assessed the correlation of low birth weight with hypospadias. Of the 2503 boys questioned, 7% reported 1 or more additional family members with hypospadias. The birth weight of the boys with hypospadias was significantly lower (p = 5X10-13) than the birth weight of their unaffected brothers. Phenotyping of 676 individuals revealed glandular hypospadias in 53%, penile forms in 39%, penoscrotal or perineal variants in 6% and cleaved prepuce as the only manifestation in 2%. There were 50% more twins than expected compared to the general population and established zygosity in 83% (67% monozygotic, 33% dizygotic) [16].
Our series does show that 9% of children with hypospadias have a familial etiology. Recurrence risk is approximately 13 times greater in first-degree relatives (brothers, fathers, and offspring) found in 9% to 17% of brothers and 1% to 3% of fathers [19]. Risk in same-sex twins is 50%. Recurrence risk in offspring is the same as in first-degree relatives [20-23].
Conclusion
Hypospadias is one of the most common birth defects although its etiology remains largely unknown. The authors investigated the familial aggregation of hypospadias. Nine percent of the children operated for hypospadias at our center, reported on additional members of the family having hypospadias. These findings underline the heavy influence of genetic factors on hypospadias development.
References
- Baskin LS, Ebbers MB (2006) Hypospadias: anatomy, etiology and technique. J Pediatr Surg. 41: 463-472.
- Paulozzi LJ (1999) International trends in rates of hypospadias and cryptorchidism. Environ Health Perspect 107: 297-302.
- Aho M, Koivisto AM, Tammela LJ, Auvinen A,Auvinen A (1970-1994) Is the incidence of hypospadias increasing? Analysis of Finnish hospital discharge data. Environ Health Perspect 108: 463-465.
- Toppari J, Kaleva M, Virtanen HE (2001) Trends in the incidence of cryptorchidism and hypospadias, and methodological limitations of registry-based data. Hum Reprod Update 7: 282-286.
- Kallgn B, Bertollini R, Castilla E, Czeizel A, Knudsen L, et al. (1986) A joint international study on the epidemiology of hypospadias. Acta Paediatr Scand Suppl 324: 1-52.
- Manson JM, Carr MC (2003) Molecular epidemiology of hypospadias: review of genetic and environmental risk factors. Birth Defects Res A Clin Mol Teratol 67: 825-836.
- Gatti JM, Kirsch AJ, Troyer WA, Perez-Brayfield MR, Smith EA, et al. (2001) Increased incidence of hypospadias in small-for-gestational age infants in a neonatal intensive-care unit. BJU Int 87: 548-550.
- Hussain N, Chaghtai A, Herndon CDA, Herson VC, Rosenkrantz TS, et al. (2002) Hypospadias and early gestation growth restriction in infants. Pediatrics 109: 473-578.
- Weidner IS, Moller H, Jensen TK, Skakkebaek NE (1999) Risk factors for cryptorchidism and hypospadias. J Urol 161: 1606-1609.
- Calzolari E, Contiero MR, Roncarati E, Mattiuz PL, Volpato S (1986) Aetiological factors in hypospadias. J Med Genet 23:333-347.
- Schnack TH, Zdravkovic S, Myrup C (2008) Familial aggregation of hypospadias: a cohort study. Am J Epidemiol 167: 251-256.
- Stoll C, Alembik Y, Roth MP, Dott B (1990) Genetic and environmental factors in hypospadias. J Med Genet 27: 559-563.
- Nordenskjold A (2004) Genetic and clinical studies on hypospadias. In Baskin LS ed. Hypospadias and genital development. AEMB Series, Kluwer Academic/Plenum Publishers, New York 545: 73-84.
- Sorenson HR (1953) Hypospadias with special reference to etiology. Copenhagen, Munksgaard 94.
- Bauer SB, Retik AB, Colodny AH (1981) Genetic aspects of hypospadias. Urol Clin North Am 8: 559-564.
- Fredell L, Iselius L, Collins A, Hansson E, Holmner S, et al. (2002) Complex segregation analysis of hypospadias. Hum Genet 111: 231-234.
- Hyun G, Kolon TF (2004) In Baskin LS Ed. Hypospadias and genital development. Endocrine evaluation of hypospadias. AEMB Series, Kluwer Academic/Plenum Publishers. 545: 31.
- Wilson JD, Griffin JE, Russell DW (1993) Steroid 5 alpha reductase 2 deficiency. Endocr Rev 14: 577.
- Snodgrass WT, Bush NC (2016) Hypospadias. In Wein AJ, Kavoussi LR, Partin AW and Peters CA Eds Campbell-Walsh Urology, Elsevier, Philadelphia 11: 3399-3429.
- Schnack TH, Zdravkovic S, Myrup C, Westergaard T, Christensen K (2007) Familial aggregation of hypospadias: a cohort study. Am J Epidemiol 167: 251-256.
- Nerli RB, Santhoshi P, Guntaka A (2010) Modified Koyanagi's procedure for proximal hypospadias: our experience. International J Urol 17: 294-296.
- Nerli RB, Guntaka AK, Patil RA, Patne PB (2014) Dorsal inlay inner preputial graft for primary hypospadias repair. Afr J Paediatr Surg 11: 105.
- Nerli RB, Kamat SM, Ravish IR (2006) Female-assigned genetic males with severe hypospadias: Psychosocial changes and psychosexual treatment. Indian J Urol 22: 42.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences