ISSN : 2393-8854
Global Journal of Research and Review
Factors Associated with Reproductive Health Seeking Behaviour among Women of Reproductive Age (15-49 years): A Case Study of Kangitit Sub-Location, Turkana East Sub-County, Turkana County
Gladys Arika1* and Ben O Osuga2
1Health Systems Management, Kenya Methodist University School of Medicine and Health Sciences, Kenya
2Lecturer and Independent Development Consultant, Kenya Methodist University, Kenya
- *Corresponding Author:
- Gladys Arika
Kenya Methodist University School of Medicine and Health Sciences
Health Systems Management, Koinange street Nairobi
Nairobi 020, Kenya
Tel: +254734502830
E-mail: tracytruck@hotmail.co.uk
Received date: January 10, 2017; Accepyed date: January 24, 2017; Published date: February 04, 2017
Citation: Arika G, Osuga BO. Factors Associated with Reproductive Health Seeking Behaviour among Women of Reproductive Age (15-49 years): A Case Study of Kangitit Sub-Location, Turkana East Sub-County, Turkana County. Glob J Res Rev. 2017, 4:1.
Abstract
Introduction: There is an increasing unmet need for safe and effective maternal health services. The health seeking behaviour among women of reproductive age is low in Kangitit Sub-location and yet no studies had been carried out in Turkana East sub-county to determine factors associated with health seeking behaviour among women of reproductive age. The main objective of the study was to describe factors associated with reproductive health seeking behaviour among women of reproductive age.
Methods: The study was a cross-sectional descriptive study conducted in Kangitit sub-location. Simple random sampling was used to select the sample population and a total of 228 respondents participate in the study. Data was collected using questionnaires with open and close ended questions and the data analysed using Statistical Package for Social Sciences (SPSS) software.
Results: The study found out that culture, belief systems and economic conditions are vital factors in determining factors associated with reproductive health seeking behaviour among women of reproductive age which can form the major concern of those who formulate and implement government health policies. The study revealed the distance to health centre from home was negatively associated with the use of antenatal care. Key barriers reported in contracted sites included physical distance, user charges and familial influences. Decision-making patterns for participants of both catchments were largely similar. Spouses and mother-inlaws particularly influenced the decision to utilize health facilities.
Conclusions: The study recommends that increased efforts should focus on sensitizing the general public on maternal health services and so programs should promote health seeking behaviour among women and training of health personnel. Maternal health programs should therefore be intensified for poor and illiterate women.
Keywords
Focused antenatal care (FANC); Antenatal care; Maternal health services; Post natal care; Health facility; Quality maternal care; Skilled birth attendant
Introduction
Access to health care overall is a challenge to rural residents, who have a lower proportion of the population insured, a greater difficulty in travelling to primary, preventative, prenatal, and emergency care providers, and less diversity in health care resources to choose from. Rural residents are left without these services, increasing the physical barriers to quality and timely healthcare. The geographic variances in access lead to the conclusion that different strategies to address health disparities will have to be considered for rural regions.
Kenya’s Service provision assessment of 2010 [1] establishes that all pregnancy are at risk of developing complications and as such to ensure good health outcome for both mother and baby pregnant women should have access to preventive interventions, early diagnosis and treatment and emergency care when needed. Studies have shown the benefits related to routine Ante-natal care for pregnant women including early management of dangers signs, preparation for delivery through individualized birth plans, provision of supplements and vaccination including tetanus toxoid vaccine ANC is designed to promote healthy behaviors and preparedness during pregnancy, childbirth and delivery (NCAPD, 2010; WHO 2003) [2,3].
To provide proper management of pregnant women’s health and in lieu of the cost and other barriers involved in access of health, WHO recommends at least 4 ante-natal visits during pregnancy (WHO, 2002) [3] There is a trend of decline in proportion of women who make four or more ANC visits during pregnancy in Kenya from 52% in 2003 to 47% in 2008 (KNBS, 2010) [4]. There is also discrepancy between geographical location of clients with rural (43.1%) and urban (59.9%) women attending 4th ANC (KNBS, 2010) [4].
Globally, reproductive health effects and is affected by, the broader context of people's lives, including their economic circumstances, education, employment, living conditions and family environment, social and gender relationships, and the traditional and legal structures within which they live. Sexual and reproductive behaviors are governed by complex biological, cultural and psychosocial factors. Therefore, the attainment of reproductive health is not limited to interventions by the health sector alone. Nonetheless, most reproductive health problems cannot be significantly addressed in the absence of health services and medical knowledge and skills [2,3].
Women bear by far the greatest burden of reproductive health problems. Women are at risk of complications from pregnancy and childbirth; they also face risks in preventing unwanted pregnancy, suffer the complications of unsafe abortion, bear most of the burden of contraception, and are more exposed to contracting, and suffering the complications of reproductive tract infections, particularly sexually transmitted diseases (STDs). Among women of reproductive age, 36% of all healthy years of life lost are due to reproductive health problems such as unregulated fertility, maternal mortality and morbidity and sexually transmitted diseases including HIV/AIDS. By contrast, the equivalent figure for men is 12% (UNEPA, 2013) [2,3].
Globally, research findings indicates that 535,900 women die from pregnancy related causes and child birth, in 2005 (WHO, 2004) [5]. The majority of the maternal deaths (62%) occur soon after birth with post-partum haemorrhage being a major cause of maternal death. In rural areas, the proportion rate of institutional deliveries is as low as 4% (WHO, 2004) [5].
In Sub-Saharan Africa, health services are poor in general, but they are particularly deficient for maternal health leading to adverse outcomes for both women and new-borns. Antenatal care is named as one of the four pillars of the safe motherhood initiative: although its relative contribution to maternal health care has been under debate, its importance cannot be denied. Less than one-third of pregnant women receive antenatal care, with a large urban and rural difference: 17% of pregnant women in rural areas receive antenatal care, while 71% of women in major cities are able to take advantage of service (WHO, 1992) [2].
In Kenya, maternal mortality increased from 380/100000 live births to 530/100000 live births between 1990 and 2008. Skilled assistance during childbirth is central to reducing maternal mortality yet the proportion of deliveries taking place in health facilities where such assistance can reliably be provided has remained below 50% since the early 1990s. The 2014 Kenya Demographic and Health Survey data is used to describe the factors that determine the where women deliver in Kenya and to explore reasons given for home delivery (KDHS, 2014-2015) [6]. Also the percentage of births attended by a skilled provider and the percentage occurring in health facilities each increased by a magnitude of 20% points from 2003 to 2014 (KDHS, 2014-2015) [6]. This therefore calls for a need to engage the community through studies that will unveil underlying issues contributing to maternal and perinatal morbidity and mortality. This study was undertaken to address some factors which are crucial in opening up of understanding some problematic issues in relation to antenatal care, health facility delivery and postnatal care utilization in this community.
In Kangitit, there have not been any studies done to explain the various challenges encountered by women of reproductive age in the area. If anything the various organizations that have operated here concentrated their efforts in nutritional emergency responses with none paying attention to the long standing maternal health needs of the community. There are therefore no figures available for comparative study.
The study aimed at identifying factors associated with reproductive health seeking behaviour among women of reproductive age (15-49 years) in Kangitit sub-location, Turkana East Sub-County, Turkana County hence identifying measures to facilitate the increase of health care facilities in the area and encourage utilization of the same in order to tame high maternal morbidity and mortality rates related to pregnancy and delivery (reproductive health) in the area.
Methodology
The study was a cross-sectional descriptive study conducted in Kangitit sub-location. Simple random sampling was used to select the sample population and a total of 228 respondents participate in the study. Every 2nd household in the selected village was considered for interview of the female in the household or 2nd female in the household where the family is polygamous. A simple random sampling method was used to select the respondents in a situation where the household had more than 1 female who are eligible for the study or in case of a polygamous family. The study targeted women of child bearing age between 15yrs to 49yrs of age. The study also included all women who have delivered in the last 3 months but excluded all the women who don’t reside in the village and just visiting who were around during the time of the study and any woman who is outside the age bracket of 15-49yrs of age.
The data analysis for the study was in both quantitative and qualitative methods. Qualitative and quantitative data were collection methods were employed in the study. Data was collected using questionnaires with open and close ended questions. The data collectors/assistants were selected and trained on data collection tools and a testing was done to ensure that they understand the questioner to reduce the errors. The questioner was administered in English however it was translated to the respondent in local language which is Turkana or Kiswahili in case the respondent didn’t understand English. The data from questionnaires responses were organized coded and then analyzed using Statistical Package for Social Sciences (SPSS). It was then summarized and presented using descriptive statistics including percentages and frequency distribution tables to illustrate the diverse findings of the study. The qualitatively, data was presented in a narrative way.
Ethical Considerations were sort during the study. The researcher sought permission from Jomo Kenyatta University of Agriculture and Technology College of Health Sciences (COHES) research committee and the Turkana East Sub-County administration to conduct the study. Consent was obtained from adult subjects and guardians where applicable. When interacting with the respondents, the researcher acted in accordance with the trust bestowed upon him by the client to maintain confidentiality in terms of restricting any disclosure of confidential information about clients/respondents. The data collected coded to conceal the identity of the respondents. They (respondents) were aware of the study as being voluntary and privacy is upheld. The report findings from the questionnaire were captured as completed by the respondents. No alterations of data were made in support of any particular conclusion. Lastly, the respondents were offered access to the results.
Results
The age of the respondents is relevant to the study since it is assumed that those respondents who were mature have adequate knowledge on Factors associated with reproductive health seeking behaviour among women of reproductive age and therefore were in a position to state the true picture.
The research sort to understand the age, education and marital status of the respondents as these were main factors that helps in understating the reasons for poor accessibility to maternal health services. The results from the respondents indicated that majority of the respondents (51.8%) were in the age bracket of 21-25 years, 29.4% were in the age bracket of 16-20 years, those above 30 years were 11% and only 2.7% were below 25 years. The high proportion 26- 40 years (65.5%) of the respondents could be attributed to low education among women shown in Table 1.
| Age | Frequency | Percent |
|---|---|---|
| Less than 16 years | 3 | 1.3 |
| 16-20 years | 67 | 29.4 |
| 21-25 years | 118 | 51.8 |
| 26-30 years | 15 | 6.6 |
| Above 30 years | 25 | 11.0 |
| Education level | ||
| No formal education | 46 | 20.1 |
| Primary education | 123 | 53.9 |
| Secondary education | 44 | 19.3 |
| Tertiary college and above | 15 | 6.6 |
| Marital status | ||
| Single | 63 | 17.4 |
| Cohabiting | 32 | 1.3 |
| Estranged/Divorced | 13 | 8.4 |
| Married | 120 | 72.9 |
Table 1: Demographic information of respondents.
On the findings of education level of the respondents, 53.9% had primary formal education, 19.3% of the respondent’s secondary formal educations, 20.1% had no formal education and only 6.6% had tertiary education which is very important as it enables them to be aware of the factors associated with reproductive health seeking behaviour among women of reproductive age,. Results on Marital status of the respondent was also sought and the results presented in Table 1 show that 72.9% of the respondents were married, 17.4% single, 8.4% divorced while 1.3% of the respondents were cohabiting.
Socio-cultural factors and sources of maternal health care services
On Socio-cultural factors and sources of maternal health care services, the findings shows that majority of the total respondents 167 (71.2%) delivered at home 40 (21.5%) had delivered at a health facility while 12 (5.3%), had delivered on their way to the facility. This indicates that most of the mother in Kangitit Sub- Location, Turkana East Sub-County, Turkana County delivered at home which clearly shows that they were not attending maternal health care services. Table 2 shows the places of delivery by the mothers.
| Frequency | Percentage | |
|---|---|---|
| Health facility | 49 | 21.5 |
| Home | 167 | 73.2 |
| On the way to the facility | 12 | 5.3 |
| Total | 228 | 100 |
Table 2: Delivery services.
On the findings related to ANC attendance and whose decision it was, the findings shows that most of the respondents 128 (56.1%) had attended ANC in the current pregnancy. 82 (36.0%) did not attend ANC while only 16 (7.9%) did not respond to the item maybe because they did not attend the ANC (Table 3). This clearly indicates that the respondents were attending the ANC. Further findings showed that the person who made the decisions for the respondents to attend ANC most on the respondents 81 (35.5%) did not response to the question probably because they did not attend ANC thus they did not respond, 75 (32.9%) said that it was their husband who made the decision of them attending ANC, 32 (14%) were on the opinion that they made the decision themselves, 24 (10.5%) said it was their mothers decisions, 12 (5.3%) said it was the neighbour who gave them the idea to attend ANC while only 4 (1.8 said it was the mother inlaw who made the decision for them to attend ANC. The results are indicated in Table 3. This results shows that the mothers who were not attending ANC, might have done so due to lack of knowledge on the importance of attending ANC and they were assisted in making the decisions to attend ANC by their husbands or neighbours. This also could be attributed to the fact that they were young because some of them had delivered at a younger age of even less than 20 years before even reaching the age of 20 years.
| Frequency | Percentage | |
|---|---|---|
| Yes | 128 | 56.1 |
| No | 82 | 36.0 |
| Not applicable | 12 | 7.9 |
| Decisions to attend ANC | ||
| Myself | 32 | 14.0 |
| Husband | 75 | 32.9 |
| My mother | 24 | 10.5 |
| Mother in-law | 4 | 1.8 |
| Neighbor | 12 | 5.3 |
| Not applicable | 81 | 35.5 |
Table 3: Antenatal care services.
On finding out if the respondents were seeking traditional healers during the pregnancy period. Most of the respondents 116 (50.9%) agreed that they visited the traditional healers while a close percentage of 112 (40.9%) disagreed that they did not visit the traditional healers. Further finding on the reason as to why they visited the traditional healers, 116 (50.9%) agreed that they visited the traditional healers because they were sick. This shows that most of the respondents visited traditional healers because they were sick during the pregnancy period. This result is indicated in Table 4.
| Frequency | Percentage | |
|---|---|---|
| Yes | 116 | 50.9 |
| No | 112 | 49.1 |
| Total | 228 | 100 |
| Reason for visiting Traditional healers | ||
| Not applicable | 112 | 49.0 |
| Sick | 116 | 50.9 |
| Total | 228 | 100 |
Table 4: Traditional healers.
On finding out whose decision was for her to deliver either in the health facility or at home. Results indicates that 62 (27.2%) said it was their mothers in-law, 68(29.6%) said it was their own decision to delivered at the place they decided to deliver, 48 (21.1%) said it was their husbands decision, 47 (20.6%) said it was the mother. This shows that the place of delivery is decided by the mother inlaw. Further finding concerning the previous delivery showered that 160 (70.2%) delivered at home, 37 (16.2%) delivered in a health facility while 31 (13.6%) did not response because it was not applicable to them (Table 5).
| Decisions on place of delivery | Frequency | Percentage |
|---|---|---|
| Myself | 68 | 29.8 |
| Husband | 48 | 21.1 |
| My mother | 47 | 20.6 |
| Mother in-law | 62 | 27.2 |
| Neighbor | 3 | 1.3 |
| Total | 228 | 100 |
| Previous place of delivery | ||
| Health facility | 37 | 16.2 |
| Home | 160 | 70.2 |
| Not applicable | 31 | 13.6 |
| Total | 228 | 100 |
| Reasons as to why they did not deliver at the health facility | ||
| Distance from home to the health facility | 121 | 53.1 |
| Distance from home to the health facility and limited staff | 10 | 4.4 |
| Distance from home to the health facility and fear to deliver in the health facility | 94 | 39.9 |
| Distance from home to the health facility and the health facility did not have equipment | 3 | 1.3 |
| No equipment at the health facility | 3 | 1.3 |
| Total | 228 | 100 |
Table 5: Decisions on place of delivery.
On finding out the reasons as to why they did not deliver at the health facility, majority of the total respondents 121 (53.1%) indicated distance from home to the health facility as major reason, 94 (39.9%) said it was far and they also had fear of delivering in the health facility,10 (4.4%) said it was far and had no staff, and a same percentage of 3 (1.3%) said they were far and health facility had not facility to assist in delivery and the same pointed out that the health facility had no facility (Table 5).
Further results on PNC attendance showered that most of the total respondents 217 (95.2%) attend PNC while 11 (4.8%) did not attend. The results further revealed that the majority 186 (61.6%) only visited the PNC because of the child immunization, 31 (13.6%) had complication after delivery and 11 (4.6%) did not responded to the item. This indicates that the reason as to why the mothers in Kangitit were attending PNC is only because of the child’s immunization if it were not for immunization, they would not be attending the PNC as shown in Table 6.
| Frequency | Percentage | |
|---|---|---|
| Yes | 217 | 95.2 |
| No | 11 | 4.8 |
| Total | 228 | 100 |
| Reason for attending PNC | ||
| Had complications | 31 | 13.6 |
| Because of child immunization | 186 | 81.6 |
| Not applicable | 11 | 4.8 |
| Total | 228 | 100 |
Table 6: Post natal care services.
Physical access factors/motivating factors to utilize maternal services
On the second objective which was to find out the physical access factors that limited the respondent to access the maternal health services, the results showered that majority of the respondents 217 (95.2%) walk distance of between 11-20 km from home to the facility to seek for maternal health as opposed to11 represented by 4.8% who walked a distance of between 6-10 km. This shows that most of the health facilities are at a distance of more than five kilometers which poses a challenge of them seeking for maternal service in the health facility. This implies that most of the health facilities are at a distance of more than five kilometers which poses a challenge of them seeking for ANC in the health facility. This result is indicated in Table 7.
| 0-5km | 6-10km | 11-20km | Over 20km | |||||
|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | F | % | |
| Facility from home during delivery | 0 | 0 | 11 | 4.8 | 217 | 95.2 | 0 | 0 |
| Facility from home during ANC | 0 | 0 | 8 | 3.5 | 220 | 96.5 | 0 | 0 |
| Facility from home during PNC | 0 | 0 | 8 | 3.5 | 220 | 96.5 | 0 | 0 |
| Total | 0 | 0 | 228 | 100 | 228 | 100 | 0 | 0 |
Table 7: Access to maternal health services.
The findings on the means of transport used when accessing maternal services indicated that 87 (38.2%) walked to the hospital while accessing maternal service, 85 (37.3%) used a motorcycle, 45 (19.7%) used a bicycle while 11 (4.8%) did not respond to the question. This shows that the mothers walked to the hospital/ health facility to seek for maternal health which gives us a clear picture on the distance they walked as to access the service which is tiresome to most of them as shown in Table 8.
| Frequency | Percentage | |
|---|---|---|
| Motorcycle | 85 | 37.3 |
| Bicycle | 45 | 19.7 |
| Walking | 87 | 38.2 |
| Not applicable | 11 | 4.8 |
| Total | 228 | 100 |
Table 8: Means of transport.
Socio-economic factors/motivating factors to use MCH
As part of socio-economic factor, the researchers sort to find out the monthly income for the mothers. The results show that most of the respondents 176 (77.2%) were not earning, 31 (13.6%) said they earned between Ksh3000-5000, 12 (5.3%) said over Ksh.20, 000, 5 (2.2) between Ksh. 5,000-10,000, 4 (1.6%) 10,000-20,000. This implies that most women do not have a source of income because they were not earning anything as shown in Table 9.
| Frequency | Percentage | |
|---|---|---|
| 3000-5000 | 31 | 13.6 |
| 5000-10000 | 5 | 2.2 |
| 1000-2000 | 4 | 1.8 |
| Over 20000 | 12 | 5.3 |
| Not earning | 176 | 77.2 |
| Total | 228 | 100 |
Table 9: Income.
The results also showed that most of the respondents did not pay for ANC services, 40 (17.5) paid nothing when seeking for delivery services while 21 (9.2%) pay Kshs. 1000 for delivery service. Finding shows majority of the respondents did not pay for PNC services because 217 (95.2%) paid zero shillings for the PNC service as summarized in Table 10. The payments we related to the transportation to the facility and other related services for ANC.
| Frequency | Percentage | |
|---|---|---|
| Payment of ANC | ||
| Zero | 58 | 25.4 |
| Not applicable | 170 | 74.6 |
| Payment of delivery | ||
| Zero | 40 | 17.5 |
| 1000 | 21 | 9.2 |
| Not applicable | 167 | 73.2 |
| Payment of PNC | ||
| Zero | 217 | 95.2 |
| Not applicable | 11 | 4.8 |
Table 10: Payment for maternal health services.
Sources of Information on Maternal Health Services
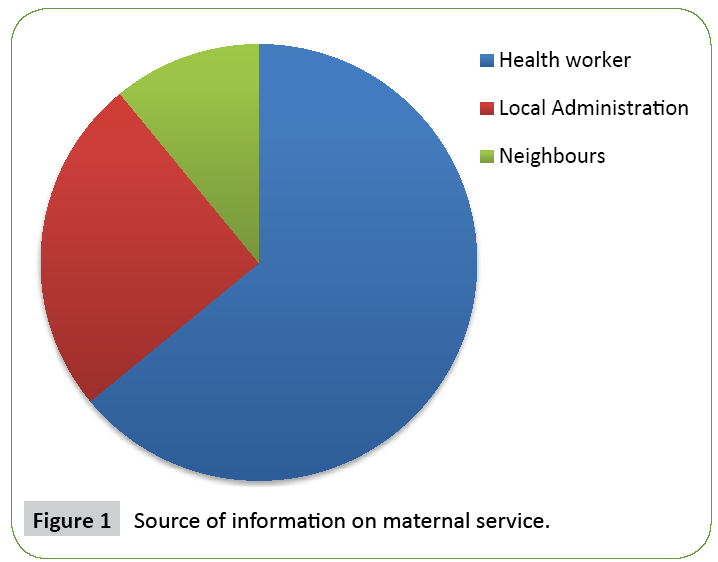
Respondents also indicated that most of them 139 (61.0%) found the information about maternal services through a health worker, 83 (36.4%) from local administration while only 6 (2.6%) received the information from the neighbours. This indicates that health workers are the main sources of information on maternal health services as indicated in the Figure 1.
Perceived quality of care/motivating factors to use care
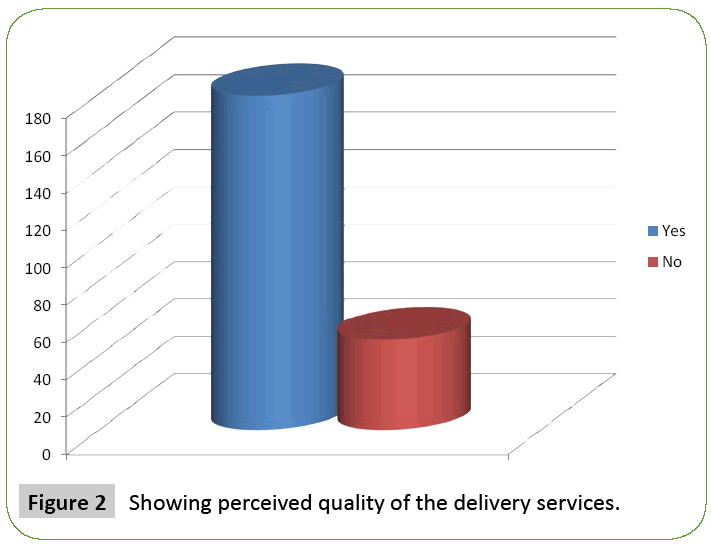
On understanding the respondents perception on quality of care in health facilities, results seeking the opinion of the respondents indicated that most of the respondents 178 (78.5%) indicated that the delivery was well conducted while 49 (21.5%) indicated that the delivery was not well conducted. This shows that the delivery is well conducted in Kangitit Location as summarized in the Figure 2.
On finding out about at the attitude of staff during the MCH services, the result showed that most of the respondents 200 (87.7%) acknowledged that the MCH staff attitude was good, 17 (7.5%) said it was fair while 11 (4.8%) said their attitude was bad. This implies that the staff have good attitude towards the patients who received MCH services as shown in Table 11.
| Frequency | Percentage | |
|---|---|---|
| Good | 200 | 87.7 |
| Fair | 17 | 7.5 |
| Bad | 11 | 4.8 |
| Total | 228 | 100 |
Table 11: Respondents perception of staff attitude in maternal health service.
Discussion
The study has identified a range of barriers, beginning from socio-cultural, physical access factors, socio-economic and perceives quality of care and cultural [7,8]. The findings indicate that financial obstacles, especially in relation to transportation, time constraints, and availability of health care staff and services influence women’s utilization of ANC and delivery services. While women who perceive prenatal and delivery care to be relevant overcome the logistical barriers with the support of family members, most notably their husbands and mothers-inlaw. Various factors facilitate women’s health seeking behaviour among women of reproductive age. As demonstrated in this study, better understanding of community and individual perceptions about prenatal care, the quality of services, and women’s health needs enable then to improve the efficacy of public health interventions and contribute to increased utilization and effectiveness of maternal and child health services.
The findings shows that most of the respondents more than half of the total respondents 128 (56.1%) had attended ANC. This clearly indicates that the respondents were attending the ANC.
Further findings out the person who made the decisions for the respondents to attend ANC most on the respondents 81 (35.5%) did not response to the question because they did not attend ANC thus they did not respond. This shows that the mother who were not attending ANC because maybe they lack the knowledge on the importance of attending ANC and they were assisted in making the decisions to attend ANC by their husbands. This also could be attributed to the fact that they were young because some of them had delivered at a younger age before even reaching the age of 20 years.
On further finding out the reasons as to why they did not deliver at the health facility majority of the total respondents 121 (53.1%) attributed distance from home to the health facility as one of the main reason why they were not able to attend the health facility because it was far. The means of transport to the health facility was also another main obstacle for the mothers to seek the services. The study revealed that most of the mothers walk to the facility to seek for the service which is tiresome and hence prefer to stay at home.
Regarding the physical factors in relation to access to maternal services distance and means of transport played key role and was a great barrier to access to the maternal services. On the distance from the facility to home during delivery majority 217 (95.2%) had to walked to cover a distance of between 11-20 km from home to the facility to seek for maternal health. This shows that most of the health facilities are at a distance of more than five kilometers which poses a challenge of them seeking for maternal service in the health facility. Finding in the table also show that the distance of the health facility to home during ANC majority 220 (96.5%) had to walked to cover a distance of between 11-20 km from home to the facility to seek for maternal health. This implies that most of the health facilities are at a distance of more than five kilometers which poses a challenge of them seeking for ANC services at the health facility. On the distance from the facility to home during PNC majority 220 (96.5%) had to walked to cover a distance of between 11-20 km from home to the facility to seek for maternal health. This shows that most of the health facilities are far for them to seek for PNC in the health facility. The findings are in line with Materia et al. who asserts that the distance to health centre from home is an important indicator of physical access to antenatal care by pregnant women. Materia et al. observed that distance of health centre was negatively associated with use of prenatal care. Okafor reported the use of prenatal care was decreased significantly with increase in distance.
On the socio-economic factors/motivating factors to use MCH, the study showered that they play a key role in the access and uptake of the MCH services. The study identified that most of the women are economically not stable and has no source of income to support and facilitate them. Most of the respondents 176 (77.2%) were not earning. This implies that most of them could not afford the payments required for delivery services. However data showed that most of the respondents did not pay for ANC services, 40 (17.5%) paid nothing when seeking for delivery services. Finding shows majority of the respondents did not pay for PNC services because 217 (95.2%) paid zero shillings for the PNC service. Respondents also indicated that most of them 139 (61.0%) found the information about maternal services through a health worker. This indicates that health workers are the main sources of information on maternal health services. The researcher’s last objective was to find out the perceived quality of care in health facilities. The researcher wanted to find the opinion regarding how the delivery process was conducted in the health facility. Results from the respondents shows that most of the 178 (78.5%) indicated that they the delivery was well conducted while 49 (21.5%) indicated that the delivery was not well conducted.
Conclusion
Culture, belief systems and economic conditions are vital factors associated with reproductive health seeking behaviour among women of reproductive age which can form the major concern of those who formulate and implement government health policies. Communities on their own part should encourage their members to appreciate health facilities, provided by the government and utilize them. The socio-cultural interpretation of threats to pregnancy affects pregnant women’s use of available healthcare services. Efforts to encourage continued use of maternity care, especially skilled birth assistance at delivery, should focus on addressing generally perceived dangers to pregnancy. Key barriers for accessing Maternal Health service included physical distance, user charges and familial influences. The study recommends increased effort on community sensitization on the maternal health services and its importance. It also recommends the training of health care professionals and increase in health facilities that offer the ANC services closer to the people to reduce distance.
Competing Interest
The authors declare no competing interest.
Authors’ Contributions
The research was done by the student as a fulfilment of the degree in Public Health. All the preparation for the research was done by the student and therefore he is the author of the article.
Acknowledgements
The author is appreciative of the support received from Sub- County health management team in Turkana East, health facility workers, community leaders and local community of Kangiti.
References
- Magadi M, Diamond I, Rodrigues RN (2000) The determinants of delivery care in Kenya. Soc Biol 47: 164-188.
- World Health Organization (2012) Trends in Maternal Mortality: 1990–2010. UNICEF, UNFPA and the World Bank, Geneva.
- World Health Organization (WHO) (2000) Maternal Mortality in 2000: Estimates Developed by WHO, UNICEF and UNFPA. Geneva.
- Kenya National Bureau of Statistics (KNBS) and ICF Macro (2010) Demographic and Health survey 2008-2009. KNBS and ICF Macro, Carlverton, Maryland.
- WHO (2004) Making Pregnancy Safer: The Critical Role of the Skilled Attendant. A joint statement by WHO, ICM and FIGO, Geneva.
- Kenya Demographic and Health Survey (2014) Key Indicators Report (PR55).
- Wagstaff A, Claeson M (2004) The Millennium Development Goals for Health: Rising to the Challenges. World Bank, Washington, USA.
- UNICEF (2009) Maternal and Newborn Health. State of the World’s Children, New York
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences