ISSN : 2576-392X
Dentistry and Craniofacial Research
Esthetic and Occlusal Considerations for Rehabilitation of Severely Worn Dentition: A Case Report
Reema Sharaf*
Dental Medicine Department, Dental Center at Prince Sultan Medical Military City, Riyadh, Saudi Arabia
- *Corresponding Author:
- Reema Sharaf Dental Medicine Department, Dental Center at Prince Sultan Medical Military City, Riyadh, Saudi Arabia, E-mail: dr.reema07@gmail.com
Received: July 07, 2021; Accepted: July 21, 2021; Published: July 28, 2021
Citation: Reema Sharaf (2021) Esthetic and Occlusal Considerations for Rehabilitation of Severely Worn Dentition: A Case Report. Dent Craniofac Res Vol.6 No.4
Abstract
Introduction: Tooth wear is a common condition affecting patients who often require advice and treatment from dentists. It is well known that the cause of tooth wear is multifactorial, making clinical diagnosis difficult. A thorough patient history is essential to help aid understanding of the causative factors. In the previous study, attrition was found to be the predominant pathological cause of tooth wear. Case description: This study describes a case of severely worn dentition in a 45 year old male who came to the dental clinic complaining of tooth discoloration and changing in their appearance. The patient’s chief complaint was difficulty in chewing and appearance problems. The patient had a history of endodontic, restorative, and prosthodontic treatment. The patient had competent lips, no asymmetry, and no signs or symptoms of temporomandibular joint disorder were detected. Initial evaluation of the patient revealed parafunctional habits of bruxism and clenching. Clinical examination revealed severe attrition of the anterior and posterior teeth. Well defined facets matching those on the opposing teeth in eccentric occlusion were also detected. The severe tooth wear was attributed to parafunctional habits. The patient had an unacceptable oral hygiene and there were generalized gingival marginal inflammation. Dental esthetics and occlusal function were restored by restoring, aligning, and replacing missing tooth structures, teeth, and/or supporting tissues. The structural stability was established by optimizing the force distribution. The functional harmony was established to improve mastication, deglutition, phonetics, and esthetics. Conclusion: This case report supports esthetic and occlusal considerations for rehabilitation of severely worn dentition in adult males.
Introduction
Tooth wear is a common condition affecting patients who often require advice and treatment from dentists. Physiological tooth wear is normal and accepted by most patients. Pathological tooth wear, by virtue of symptoms or rapid wear will prompt the need for dental care. It can range from mild sensitivity due to an abrasion lesion to gross destruction of the dentition. Similarly, treatment can range from simple operative care to full mouth reconstruction with crowns or complex dentures. Inadequate or over treatment can lead to tooth loss and patient complaints [1].
Tooth wear, or as it is also often referred to as non-carious tooth surface loss, can be described simply as ‘the pathological non-carious loss of tooth tissue’ [2]. The distinction between pathological and physiological tooth wear can be difficult to determine. Wearing of the teeth is a normal physiological process. The estimated normal vertical loss of enamel from physiological wear is considered approximately 20−38 μm per annum [3]. It is important to remember that just because a tooth has some element of wear, this does not always necessitate treatment. Tooth wear may be regarded as pathological if the rate of wear is greater than that expected for the patient’s age, the patient has concerns over the wear or the prognosis of the tooth is compromised due to wear.
Tooth wear is often multifactorial in nature and can be difficult to distinguish between, but it is often subdivided into attrition, erosion, abrasion, and abfraction. Attrition refers to the loss of tooth substance or restoration as a result of mastication or contact between occluding surfaces of approximal surfaces’ [2]. Erosion is defined as the loss of tooth tissue by chemical processes not involving bacterial actions’ [4]. Abrasion is characterized by physical wear caused by materials other than tooth contacts’ [5]. Abfraction refers to tooth wear located in the cervical area caused by flexural forces during function and parafunctions’ [6].
A survey in 2009 showed an increased incident of tooth wear between 66% and 76% since the 1998 survey [7]. Tooth wear of the dentine was found to be higher than previously, at 77% in the anterior teeth. Moderate tooth wear (extended dentine) also showed an increase from 11% in 1998 to 15% in 2009. Severe wear (exposed secondary dentine) remained at 2% [7]. Tooth wear in adults is a common clinical finding, with an increase in prevalence with advanced age. A systematic review showed 3% of 20 year olds and 17% of 70 year olds exhibited severe tooth wear [8]. Furthermore, it has been suggested that males tend to experience greater tooth wear than females, possibly due to increased tooth retention and greater occlusal forces in males [9]. It is well known that the cause of tooth wear is multifactorial, making clinical diagnosis difficult. A thorough patient history is essential to help aid understanding of the causative factors. In the previous study, attrition was found to be the predominant pathological cause of tooth wear [10]. It is important to acknowledge that the level of tooth wear is normal, physiologically increasing with age, but may become pathologically secondary to a parafunctional habit [11].
Case Presentation
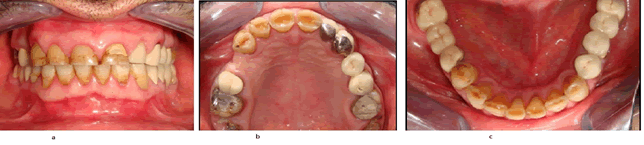
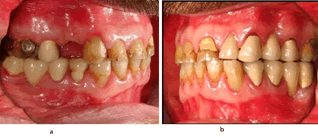
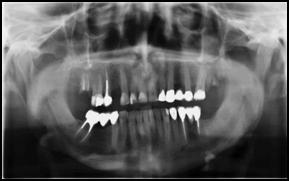
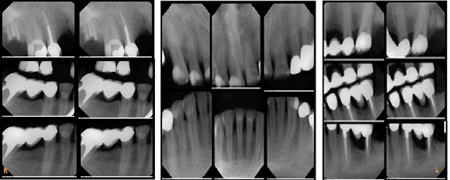
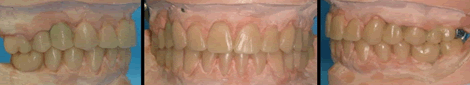
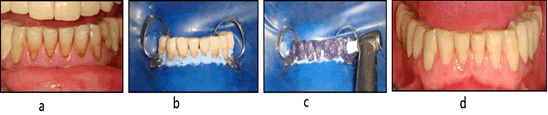
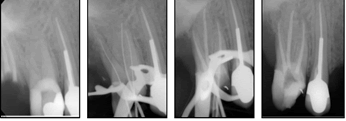
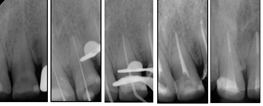
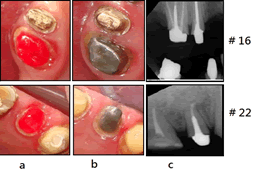
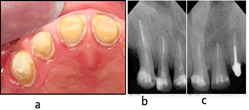
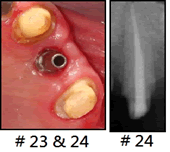
A 45 year old military male came to the department of Restorative Dentistry for the treatment of worn teeth. The patient’s chief complaint was difficulty in chewing, tooth discoloration, and appearance problems. The patient had a history of Hypothyroidism which was controlled by thyroxin tablets (100 mg) daily for the last 20 years. He also had a history of vitiligo, for which he did not take any medications. The patient had a history of endodontic, restorative, and prosthodontic treatment. The patient had competent lips, no asymmetry, and no signs or symptoms of temporomandibular joint disorder (TMD) were detected. Initial evaluation of the patient revealed parafunctional habits of bruxism and clenching. Clinical examination revealed severe attrition of the anterior and posterior teeth. Well defined facets matching those on the opposing teeth in eccentric occlusion were also detected. The severe tooth wear was attributed to parafunctional habits. The patient had an unacceptable oral hygiene and there were generalized gingival marginal inflammation (Figures 1 and 2). Radiological features are presented in (Figures 3 and 4).
Clinical and restorative protocol
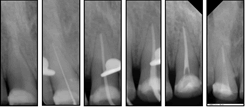
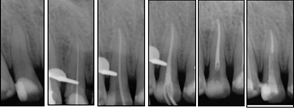
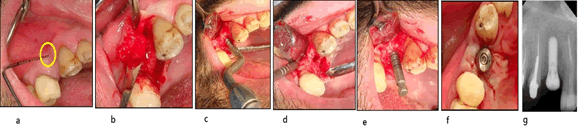
Dental esthetics and occlusal function were restored by aligning, restoring, and replacing missing tooth structures, teeth, and/or supporting tissues. The structural stability was established by optimizing the force distribution. The functional harmony was established to improve mastication, deglutition, phonetics, and esthetics. Diagnostic wax up is a preliminary step to the actual preparation of teeth as suggested by proponents of gnathological techniques that will decrease the possibility of errors in the construction of any extensive FPD prosthesis (Figures 5 and 6). The success of any procedure requires the willingness of the general dentists and specialists to “spend more time in planning than doing” [12]. The radiographs of endodontic treatment are presented in (Figures 7–11). Procedures of dental implants are shown in (Figures 12–16).
Figure 16: Dental implant procedure of # 14 (a) Vertical bone defect. b) Flap reflection. c) Bone expansion using osteotome. d) After bone expansion. e) Confirmation of the initial depth of the osteotomy using depth gauge. f) Healing cap. g) Standard Plus Implant ? 4.1 RN, SLA 12 mm).
Discussion
Dentists face a complex and complicated problem when reconstructing a badly worn dentition [13]. Excessive wear, for whatever cause, may have a negative impact on the stomatognathic system's esthetics, function, and health [14]. As a result, it is important to recover it using all available treatment options. With today's materials and procedures, a wide variety of restorative care methods are available. In this case, repairing, aligning, and replacing missing tooth structure, teeth, and/or supporting tissues, dental esthetics, and occlusal function were restored. Additionally, the structural stability was achieved by force distribution optimization. Finally, mastication, deglutition, phonetics, and esthetics were all improved as a result of the practical harmony. For patients with tooth wear, these methods of care have been recommended by a variety of clinicians [15- 17]. These methods are a relatively simple, non-invasive, and cost effective way to enhance the appearance and function of the dentition [14]. Since this patient was a known case of hypothyroidism, the restorative procedure was considered accordingly. Patients with medically stable hypothyroidism who receive dental implants may not have a greater risk of implant failure. The presence of controlled hypothyroidism does not seem to be a contraindication to endosseous implant therapy [18]. Despite the lack of evidence that bruxism induces an excess of dental implants and their suprastructures, practitioners should proceed with caution when planning implant procedures in bruxists. To minimize the risk of complications and, eventually, implant failure, some realistic guidelines are available [19]. It is recommended that more implants be placed in the presence of bruxism than would be required in the absence of this movement disorder. More precisely, one implant should be positioned for each missing element to prevent free ending situations. As the number of implants increases, the force exerted on each individual implant decreases [19]. By mechanically connecting the implants, the forces are better distributed and the stresses in the bone around the implants are reduced [19]. A night guard (hard stability splint) assists in optimally spreading and vertically redirecting the forces associated with nocturnal tooth grinding and clenching [19]. In cases where there is inadequate bone quantity, the aim of augmentation is to establish a predictable function and appearance. Various methods, such as hard tissue onlays, bone grafts, membrane techniques, bone distraction, and bone expansion, may be used to do this. Despite the fact that comprehensive research has been focusing on developing alternative materials over the last decade, autogenous bone is still known as the best material for bone augmentation [20].
Conclusion
This case study supports esthetic and occlusal considerations for the rehabilitation of adult males with badly worn dentition.
References
- Hemmings K, Truman A, Shah S, Chauhan R (2018) Tooth wear guidelines for the bsrd part 1: Aetiology, diagnosis and prevention. Dental Update 45: 483-495.
- Kelleher M, Bishop K (1999) Tooth surface loss: An overview. British Dental J 186: 61-66.
- Lambrechts P, Braem M, Vuylsteke-Wauters M, Vanherle G (1989) Quantitative in vivo wear of human enamel. J dental res 68: 1752-1754.
- Bishop K, Kelleher M, Briggs P, Joshi R (1997) Wear now? An update on the etiology of tooth wear. Quintessence International 28(5).
- Smith BGN, Robb ND (1989) Dental erosion in patients with chronic alcoholism. J Dentistry 17: 219-221.
- Lee WC, Eakle WS (1984) Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthetic Dent 52: 374-380.
- White DA, Tsakos G, Pitts NB, Fuller E, Douglas GVA, et al. (2012) Adult dental health survey 2009: common oral health conditions and their impact on the population. British dental j, 213: 567-572.
- Van’t Spijker A, Rodriguez JM, Kreulen CM, Bronkhorst EM, Bartlett DW, et al. (2009) Prevalence of tooth wear in adults. Int J Prosthodont 22: 35-42.
- Donachie MA, Walls AWG (1995) Assessment of tooth wear in an ageing population. J dentistry 23: 157-164.
- Smith BG (1984) An index for measuring the wear of teeth. Br Dent J 156: 435-438.
- Grippo JO, Simring M, Schreiner S (2004) Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J Ameri Dent Assoc, 135: 1109-1118.
- Morgan DW, Comella MC, Staffanou RS (1975) A diagnostic wax-up technique. J prosthetic dentistry, 33: 169-177.
- Hammad IA, Nassif NJ, Salameh ZA (2005) Full-mouth rehabilitation following treatment of temporomandibular disorders and teeth related signs and symptoms. CRANIO®, 23: 289-296.
- Pruthi G, Jain V, Agnihotri H (2011) Rehabilitation of a severely worn dentition using fixed and removable partial overdenture prostheses. Int J Prosthodont 1: 59-64.
- Brown KE (1980) Reconstruction considerations for severe dental attrition. J prosth dentis 44: 384-388.
- Graser GN, Rogoff GS (1990) Removable partial overdentures for special patients. Dental clinics of North America 34: 741-758.
- Watson RM (1997) The role of removable prostheses and implants in the restoration of the worn dentition. Euro J prosthodon restorative dentist 5: 181-186.
- Attard NJ, Zarb G.A (2002) A study of dental implants in medically treated hypothyroid patients. Clinical implant dentistry and related research 4: 220-231.
- Lobbezoo F, Brouwers JEIG, Cune MS, Naeije M (2006) Dental implants in patients with bruxing habits. J oral rehab 33: 152-159.
- Barman J (2014) Occlusal considerations, concepts and treatment planning for full mouth rehabilitation of mutilated dentition. Indian J Stomato 5: 102.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences