Entrapment of the Long Head of the Biceps in a Multi-Fragmentary Proximal Humeral Fracture: A Case Report
Department of Orthopedic Surgery and Traumatology, Saint Georges University Medical Center, Balamand University, Achrafieh, Beirut, Lebanon
- *Corresponding Author:
- Abdel Nour HG
Department of Orthopedic Surgery and Traumatology, Saint Georges University Medical Center, Balamand University, Achrafieh, Beirut, Lebanon
Tel: +9611575700
E-mail: hicham.abdelnour.dr@gmail.com
Received date: June 29, 2018; Accepted date: July 11, 2018; Published date: July 20, 2018
Citation: Abdel Nour HG, Joukhadar NI, Maalouly J, Ayoubi RA, Aouad DK, et al. (2018) Entrapment of the Long Head of the Biceps in a Multi- Fragmentary Proximal Humeral Fracture: A Case Report. J Physiother Res. 2:10.
Copyright: © 2018 Abdel Nour HG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Entrapment of the long head of the biceps tendon in proximal humeral fractures is an uncommon pathology described in the literature in rare cases especially in the pediatric population. Clinical presentation may be misleading, and the diagnosis of proximal humeral shoulder fractures with or without biceps tendon entrapment could be missed on plain radiographs and even on 3D reconstruction CT scan. Interposition of the long head of the biceps in complex proximal humeral fractures may be a challenge for proper anatomical percutaneous or open reduction of these fractures. The following case report describes a case of a patient involved in a ski accident falling on an outstretched arm with an atypical presentation of long head of the biceps (LHB) tendon entrapment in a multi-fragmentary depressed intra-articular proximal humeral fracture. The patient underwent prompt surgical intervention.
Keywords
Long head of the biceps; Tendon entrapment; Proximal humeral fractures; Shoulder
Introduction
Proximal humerus fractures account for 5% of all fractures and are the third most common fractures occurring in the adult population over the age of 65. Most of these fractures are relatively non-displaced and can be successfully managed non-operatively [1]. In addition to conservative treatment, many surgical interventions are at hand, including open reduction and internal fixation (ORIF) with a variety of devices, hemiarthroplasty, and percutaneous fixation [2]. Some authors discussed the concern about interposed soft tissue, such as the long head of the bicep tendon, in proximal humeral fractures in the pediatric population. These same authors have offered this fear of tissue entrapment as the main reason for recommending open reduction [3]. We discuss an atypical presentation of a case of an adult patient diagnosed with entrapment of the LHB in a complex proximal humeral fracture after a ski injury.
Case Study
This is the case of a 43 year old male patient that presented to our emergency department complaining of minimal pain and tenderness in his left shoulder after sustaining a fall during skiing. The patient noted a high speed down slope injury and falling on an outstretched hand with the shoulder abducted in 90 degrees on direct impact with the snow. The incident took place around 6 hours prior to his presentation and he continued his day skiing normally with intermittent minimal stabbing pain over the lateral aspect of the affected shoulder. He presented for assessment and management of severe shoulder pain.
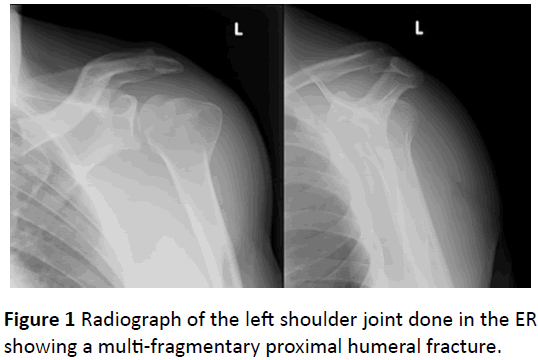
Upon inspection he had no swelling, edema, erythema or any ecchymosis over his left shoulder. Upon physical examination the patient had a full normal slightly painful range of motion of his left shoulder joint with moderate tenderness upon palpation of his left proximal humerus. No neurovascular deficits were associated with his injury. In the ED a standard Antero-Posterior and lateral radiographs of the affected shoulder joint were done and surprisingly showed a multi-fragmentary displaced humeral head fracture (Figure 1).
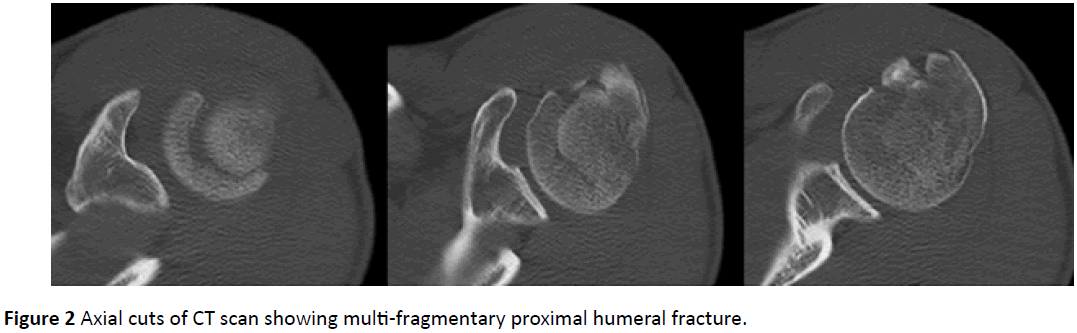
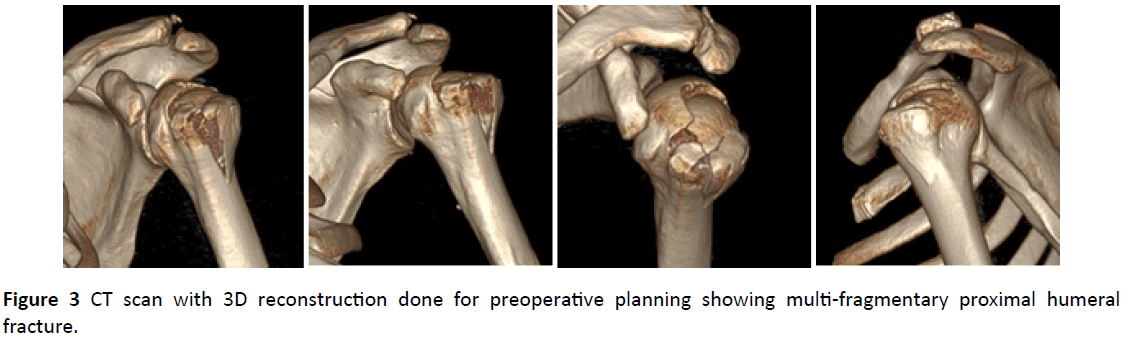
CT-Scan (Figure 2) with 3D reconstruction (Figure 3) was ordered for further evaluation and pre-operative planning. The scan showed an acute comminuted, markedly displaced, vertically oriented fracture of the proximal humerus, extending from the most superior aspect of the articular surface of the humeral head at its mid aspect and the lateral two thirds. The fracture lines also extended to involve the greater tuberosity which was laterally displaced, the proximal humerus metadiaphyseal junction at the humeral surgical neck and the floor of the bicipital tendon groove.
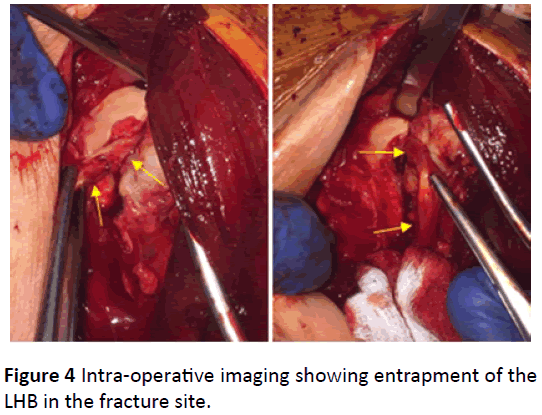
The patient was transferred to the operating room at once for planned percutaneous fixation of his left proximal humerus fracture with Kischner wires and cannulated screws. With the patient placed in the beach chair position, and after multiple failed trials of proper anatomic reduction and fixation the decision was taken to switch to an open technique. A mini deltopectoral incision approach to the proximal humerus was made. After multiple unsatisfactory extra articular attempts of reduction of the fracture and anatomical realignment of the articular surface, a decision was taken to enter the joint and reduce the fracture fragments under direct vision. Proper dissection and entry into the shouder joint was done through the rotator cuff interval with proper retraction, while taking care not to breach the integrity of the cuff insertions. Surprisingly the LHB was found to be entrapped in the longitudinal split banana shaped fracture of the superior articular surface of the humeral head, extending from the bicipital groove anteriorly all the way posteriorly at the cartilage bone interface (Figure 4).
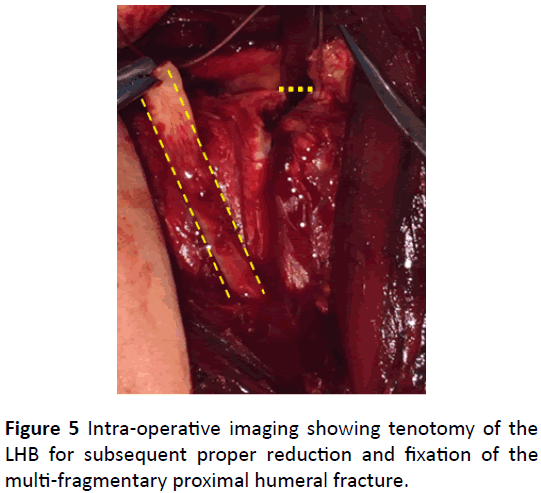
Anatomical realignment of the articular surface and freeing the entrapped LHB tendon was impossible, so the decision was taken to do a LHB tenotomy (Figure 5).
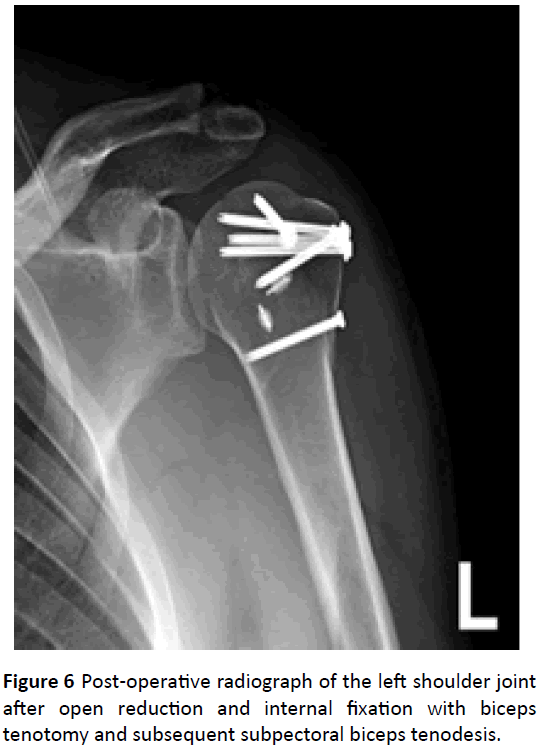
After the tenotomy was done, anatomical reduction of the fracture and the articular surface was achieved and fixed with screws (Figure 6). Subsequently subpectoral tenodesis to restore the biceps function was done.
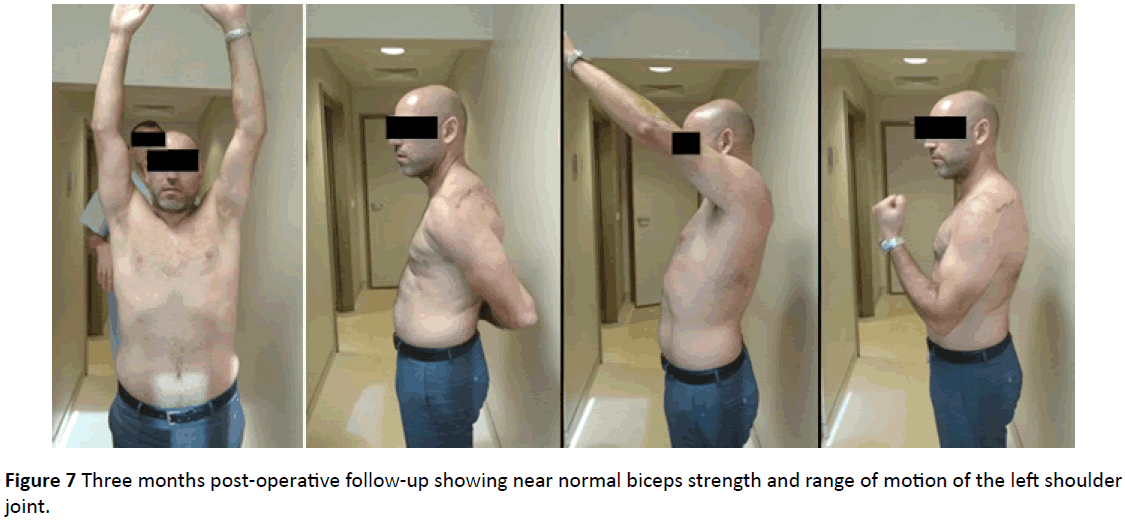
His shoulder was immobilized for the first 3 weeks post operatively with a proximal humerus shoulder immobilizer. After 3 weeks physical therapy was initiated starting with passive range of motion for 2 weeks and then progressing to active range of motion as tolerated without any biceps strengthening for the first 6 weeks. The patient presented 3 months after the surgery with full active and passive range of motion and near normal biceps muscle strength (Figure 7).
Discussion
Proximal humerus fractures typically involve the humeral head and neck. Because of the importance of the proximal humerus which serves as the insertion and origin for multiple muscles, the attachment of several ligaments, and shoulder articulation, the precision of management of these fractures is highly importance in order to decrease morbidity and optimize functional outcomes [4]. The majority of PHFs are the result of low energy falls, are minimally displaced, and may be treated with sling immobilization and physical therapy. However, in around 20% of fractures, surgery should be taken into consideration. The treating surgeon must have a wellstructured idea of the fracture itself, the patient’s bone quality, other patient-related factors, and the different reconstructive surgical options [5]. In most cases standard plain radiographs are enough to define the fracture pattern. Computed tomography (CT) can be used to evaluate for a head-splitting component, better visualize bone quality and extent of commination, and to further delineate the fracture configuration. The fracture pattern is of great importance when it comes to making the choice for treatment options and predicting the risk of osteonecrosis after proximal humeral fractures [5]. Some of these fractures are irreducible, but there are only few reports in the literature of tissue interposition into the fracture site [6,7].
The LHB tendon resides within a groove separating the greater and lesser tuberosities. The long head of the biceps tendon originates from the supraglenoid tubercle of the scapula and crosses the head of the humerus within the shoulder joint’s capsule, exiting along the intertubercular sulcus joining with the short head. The transverse humeral ligament retains the tendon in the bicipital groove [3].
Only a few reports in the literature of tissue interposition into the fracture site are reported, with the majority of cases cited being pediatric patients [3,6,7]. Smith cited a case study of a 12-year-old with a severely displaced fracture with a clinical diagnosis of biceps tendon interposition into the fracture site. The patient was followed conservatively and at 8 weeks could actively abduct his arm 160°C, externally rotate 60°C, and internally rotate 70°C. By 6 months he had regained total use of the arm and shoulder, without pain. He concluded that although the injury appears serious, full recovery of the arm and shoulder occurs and the original angular deformity remodels over time [6].
Bahrs et al. discussed 43 cases of proximal humeral fractures in children and adolescents concluding that a failed closed reduction should be interpreted as a possible soft tissue entrapment most likely because of the long head of the biceps [8].
Visser and Rietberg presented three case studies of fracture separation of the proximal humerus in children (all Salter- Harris type II) that failed efforts at closed reduction and underwent open reduction and internal fixation due to the extreme displacement of the fracture fragments, along with interposition of both the long head of the biceps and periosteum [7].
Lucas et al. reported three cases from the pediatric age group with proximal humerus fracture post fall on outstretched arm with evidence of LHB tendon or other soft tissue interposition into the fracture site. All three cases were treated non-operatively with closed reduction and immobilization and followed with progressive regain of their shoulder range of motion to normal with significant radiographic bone remodeling. They also underwent a cadaveric study to investigate the possible LHB tendon impingement by a simulated proximal humeral fracture. An osteotome and mallet were used to create a simulated fracture (transversely oriented) at the level of the surgical neck of the humerus, immediately above the insertion of the pectoral is major muscle. After manipulating the fracture in multiple directions, the LHB tendon did not become interposed into the fracture site at any point of the wide range of humeral motion abduction, flexion, internal and external rotation [3].
Henderson described a case of a thirty year old male diagnosed with interposition of the LHB after sustaining a sub coracoid fracture-dislocation of his shoulder post electroconvulsive therapy for depressive disorder [4].
In the literature, there are cases of axillary artery entrapment, associated with proximal humeral fracture but none described any entity of LHB entrapment. Palm et al. cited a case of a 38 year old woman that was diagnosed with a proximal humeral fracture post trauma. She was also diagnosed with a concomitant axillary artery entrapment in the fracture site and a brachial plexus injury [9]. Keser et al. also described a case of a 51 year old male patient diagnosed with axillary artery entrapment following a proximal humeral fracture [10].
Conclusion
Shoulder injuries can be very simple injuries to deal with in the ED but sometimes they could be challenging especially in patients presenting for regular checkup post trauma and in those with minimal pain and normal shoulder range of motion. Standard radiographs of the shoulder joint should always be done after moderate or high energy trauma in young adults because sometimes the clinical exam may be misleading and proximal humeral fractures could be easily missed. On the other hand, entrapment of the long head of the biceps should be considered in any unsuccessful attempt of reduction in proximal humeral fractures. Tenotomy and subsequent tenodesis of the LHB could be necessary in severely comminuted intra-articular humeral head fractures where anatomic reduction is primarily impossible.
References
- Grawe B, Le T, Lee T, Wyrick J (2012)Open reduction and internal fixation (ORIF) of complex 3-and 4-part fractures of the proximal humerus: does age really matter? Geriatric orthopadi surgery rehab 3: 27-32.
- Mao Z, Zhang L, Zhang L, Zeng X, Chen S, et al. (2014) Operative versus nonoperative treatment in complex proximal humeral fractures. Orthopedi 37: e410-419.
- Lucas JC, Mehlman CT, Laor T (2004) The location of the biceps tendon in completely displaced proximal humerus fractures in children: a report of four cases with magnetic resonance imaging and cadaveric correlation. J Pediatric Orthopaedi 24: 249-253.
- Henderson RS (1952) Fracture-dislocation of the shoulder with interposition of long head of biceps. J Bone Joint Surg Br 34: 240-241.
- Mauro CS (2011) Proximal humeral fractures. Current reviews musculoskeletal med 4: 214-220.
- Smith FM (1956) Fracture-separation of the proximal humeral epiphysis: a study of cases seen at the Presbyterian hospital from 1929–1953. American J Surg 91: 627-635.
- Visser JD, Rietberg M (1980) Interposition of the tendon of the long head of biceps in fracture separation of the proximal humeral epiphysis. Netherlands J surg 32: 12.
- Mehlman CT (2010) Proximal Humeral Fractures in Children and Adolescents. J Pediatri Orthopadi 30: 942-943.
- Palm DS, Parikh PP, Schoonover B, Lebamoff D, McCarthy MC (2013) Axillary arterial entrapment and brachial plexus injury due to proximal humeral fracture. Injury Extra 44: 67-69.
- Keser S, Ege A, Turhan E, Songür M, Bayar A, et al. (2011) Axillary artery entrapment following proximal humeral fracture: a case report and review of literature. European J Orthopaedic Surg Traumatolo 21: 117-22.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences