ISSN : 2347-5447
British Biomedical Bulletin
Diastasis Recti and its Non-Aesthetic Clinical Consequence: A Review
Dilainy Peña*, Mariana Añolis, Jesús Piña, Adel Al Awad and María Matera
Student Community for the Dissemination and Research of Human Anatomy (CEDIAH), University of Zulia, Maracaibo, Venezuela
- *Corresponding Author:
- Dilainy Peña
Student Community for the Dissemination and Research of Human Anatomy (CEDIAH),
University of Zulia, Maracaibo,
Venezuela,
E-mail: dilainypb@gmail.com
Received date: February 18, 2024, Manuscript No. IPBBB-24-18667; Editor assigned date: February 21, 2024, PreQC No. IPBBB-24-18667 (PQ); Reviewed date: March 06, 2024, QC No. IPBBB-24-18667; Revised date: March 13, 2024, Manuscript No. IPBBB-24-18667 (R); Published date: March 20, 2024, DOI: 10.36648/2347-5447.12.1.34
Citation: Peña D, Añolis M, Piña J, Al Awad A, Matera M (2024) Diastasis Recti and its Non-Aesthetic Clinical Consequence: A Review. Br Biomed Bull Vol.12 No.1: 34.
Abstract
Diastasis Recti (DR) is defined as the separation of the rectus muscles in the midline of the abdomen. It shows an increase in length and gradual widening of the fibers that form the linea alba. The objective of this research was to describe the incidence, clinical manifestations, complications and treatment of diastasis recti of the rectus abdominis muscles, as well as to identify its medical rather than aesthetic implication. This research was performed in a descriptive manner by reviewing literature published in various scientific journals where published articles were selected, in a period between 2017 and 2024, with no restrictions on the type of article. DR is a condition that can occur in both sexes, being asymptomatic in most cases and when it has major repercussions beyond the aesthetic, such as low back pain and pelvic floor dysfunction, are identified.
Keywords
Diastasis; Rectus abdominis; Clinical repercussions; Complications
Introduction
Diastasis Recti (DR) is defined as the separation of the rectus muscles in the midline of the abdomen, also called "interrectal distance". In this line, the increase in length and the gradual widening of the fibers that make up the linea alba are evident [1,2]. It should be noted that not every separation of the linea alba is considered pathological and there is no consensus on the choice of normal parameters, because the physiological parameters of the width of the linea alba vary according to the height of the abdominal wall and increase with age; however, it is widely accepted that a separation greater than 2 cm to 2.5 cm is considered an abnormal parameter [3,4].
An increase in the distance between the anterior borders of the rectus muscles influences the strength of the abdominal wall musculature and does not usually cause pain at rest [5]. DR is not only caused by a separation of the linea alba due to increased intra-abdominal pressure, as in heavy exercise and increased body weight, but also by a general laxity of the abdominal musculature, or by collagen alteration in special situations such as pregnancy, obesity or ascites [1-3,6].
DR has been considered in the first instance a purely aesthetic alteration because patients present personal psychological discomfort which results in difficulty in accepting their appearance [2,3,6]. However, it has been described the alteration of the biomechanical properties of the abdominal wall with diastasis generating clinical consequences [1]. On the other hand, diastasis may be associated with the presence of primary midline defects, including umbilical, epigastric and incisional hernias [2,3], so it may be erroneously considered as a primary ventral hernia, however, the absence of a true defect and hernia sac differentiates it from these [2].
It can occur in both sexes equally and in any age group, but it is frequently observed in women during pregnancy and the puerperium [2]. On the other hand, there is surgical treatment for the repair of DR by abdominoplasty or laparoscopy, although conservative treatment is also an alternative [4]. Based on the above the aim of the present investigation is to describe the incidence, clinical manifestations, complications and treatment of diastasis recti of the rectus abdominis muscles, as well as to identify its medical rather than aesthetic implication.
Review of Literature
This is a descriptive and retrospective research conducted by reviewing the literature published in various scientific journals. The articles were collected from databases such as: Elseiver, SciElo, PubMed and Google Scholar, by implementing keywords such as "diastasis recti", "rectus abdominis rectus muscles", "diastasis", "diastasis recti". The search is not limited to a specific population. The selection criteria include articles published, in a period between 2017 and 2024, with no restrictions on the type of article.
Discussion
Epidemiology and etiology
DR occurs in both sexes and in all age groups, but a higher prevalence affects women of childbearing age mainly in the second and third trimester of pregnancy and the postpartum period [2,5]. This is because, during pregnancy, the abdominal wall distends as fetal development occurs, in some cases causing excessive stretching of the linea alba connective tissue. Likewise, in the postpartum period this distension tends to reduce; however, some authors have found that up to 32.6% of women continue to have DR one year after delivery [7].
Generally speaking, the risk groups for the occurrence of DR are mainly pregnant women, in the umbilical region. On the other hand, in men, especially obese men it is usually supraumbilical and occurs between 50-60 years of age [1,2]. Similarly, it has been associated with increased risk in multiple pregnancies, fetal macrosomia and polyhydramnios in thin women, while in men DR is thought to be associated with increasing age and excessive tension in the linea alba, for example, in the presence of ascites and central obesity [2].
Other proposed risk factors also include weight gain and hormonal changes during pregnancy (increased secretion of relaxin, progesterone and estrogen), type of delivery, birth weight of the baby, benign joint hyperlaxity syndrome, bifurcated xiphoid process, heavy lifting, general physical training, lumbo-pelvic pain, urogenital dysfunctions, level of pelvic and abdominal floor muscles, history of cesarean section and ethnicity [8-12].
should be noted that, in recent years, studies have been published associating the occurrence of DR with a congenital defect in type I/III collagen synthesis, but these data are still awaiting solid scientific evidence [5,6]. DR can also occur after the patient undergoes a surgical procedure [10]. On another note, it has been described that DR may be due to a congenital defect, such as that occurring in Beckwith-Wiedemann syndrome, characterized by macroglossia, body hemihypertrophy, hypoglycemia, anterior abdominal wall defects, omphalocele and/or DR, which occurs in 0.07% of newborns [13].
DR is related to diabetes mellitus, because it can cause loss of muscle mass and function, as well as sarcopenia; this can lead to changes in the anterior rectus abdominis musculature which could be explained by two mechanisms: Diabetes could contribute to altered mitochondrial oxidative phosphorylation and hypercomplex assembly in rectus abdominis muscle fibers and it could also induce changes in muscle structure by reducing fast fibers and increasing slow fibers [12].
Anatomical aspects
The anterolateral abdominal wall is formed by muscles that can be found symmetrically on both sides of the linea alba. These are, located in the anterior midline, the rectus abdominis muscles with vertically running fibers and the lateral flat muscles: External oblique, internal oblique and transverse, with obliquely and perpendicularly running fibers respectively. The rectus muscles are polygastric muscles, made up of 4-5 units, each with its own motor innervation, which can contract synchronously, which gives them both static (they are involved in forced expiration, coughing, defecation and urination) and dynamic properties (they participate in trunk flexion and in the most important biological process for the survival of our species: Childbirth [6].
It is important to note that the connected aponeuroses of the muscles of the lateral abdominal wall form a sheath that encompasses the rectus abdominis muscle, but in its lower third, the rectus muscles lack a posterior sheath, which gives this part of the abdominal wall greater elasticity [5,6]. The aponeuroses of the opposite sides cross in the midline, fusing the medial edges of the sheaths and thus forming the Linea Alba (LA), a sheet of fibrous tissue that occupies in the midline the space between the rectus muscles; it extends from the xiphoid process of the sternum to the superior pubic ligament and plays an important role in maintaining the stability of the abdominal wall [6,9,14,15].
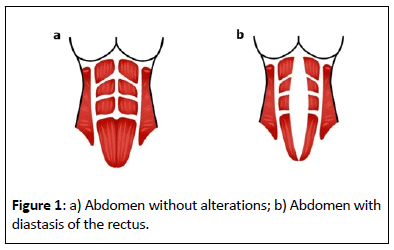
In that sense, the anatomical interactions between the rectus muscle and the lateral muscles (external oblique, internal oblique and transverse abdominal muscles) may play an important role in understanding the actual etiopathogenesis of DR (Figure 1). Cavalli et al. 2021, found in cadaveric dissections that the internal oblique aponeurosis can attach to the rectus sheath in two ways, namely by dividing its fibers into an anterior and posterior layer, as classically described, or by attaching only the posterior rectus sheath, without an anterior layer [12].
Therefore, to confirm the new crescentic line variation, they performed a retrospective review of abdominal CT images in 100 patients and found that in 89/100 (89%) of the patients the classic insertion was present, but in 11/100 (11%) only a posterior insertion was present. In patients with the classic insertion, only 23/89 (26%) of the CT images showed a diastasis recti (according to Rath et al. 1996, definition whereas in patients with only the posterior insertion, diastasis was present in all patients at 100%); therefore, it seems that only the posterior insertion could be considered a risk factor for diastasis [12,16].
Clinical implications
DR may or may not be associated with the presence of symptoms. Clinically it is characterized by an increase in volume that may be present in supraumbilical, umbilical and infraumbilical locations, being superior, middle and inferior diastasis, respectively, or encompassing the entire midline [2-4,17]. On physical examination it can be observed when the patient in dorsal decubitus elevates the head, producing an increase in intra-abdominal pressure as the muscles contract, showing the appearance of a diffuse fusiform protrusion in the midline [3].
It is usually associated with midline hernias but the absence of a true hernia defect and hernia sac differentiates it from the latter, so because there is no fascial defect there is no risk of incarceration or strangulation in diastasis [2,17]. Similarly, DR can manifest as dorsolumbalgias (68%), digestive disorders (constipation), muscular alteration of the pelvic floor with urogynecological pathology (60%), affecting the quality of life of these patients [14]. This can be evidenced in a multicenter study conducted by Juárez et al. 2019, in almost all cases the reason for consultation was abdominal pain related to the presence of hernial defects, as well as stress urinary incontinence (32.3%), low back pain (50%) and constipation (36%) [14].
Several studies have shown that the myofascial laxity associated with rectus diastasis is both vertical and horizontal and, in severe cases, can affect the entire anterior abdominal wall, including the linea alba and linea semilunaris. However, thinning and stretching of the linea alba is a major risk factor for the actual development of midline hernias (umbilical, epigastric, trocar and incisional hernias) due to connective tissue impairment and abdominal muscle tension [12,18,19].
Table 1 describes the classification of Rath et al. in which a separation at each abdominal level is determined so that it can be defined as diastasis [1,16].
| Rath y Cols | Supraumbilical | Umbilical | Infraumbilical |
|---|---|---|---|
| >45 años | >10 mm | >27 mm | >9 mm |
| Ë?45 años | Ë?15 mm | Ë?27 mm | Ë?14 mm |
Table 1: Rath classification of diastasis recti. Source: Teran et al. [1].
The abdominal wall plays an important role in posture and its control, pelvic and trunk stability, breathing, trunk movement and support of the abdominal viscera, so persistent DR can lead to a variety of symptoms and dysfunctions [20,21]. Patients with DR may present with pain in the region corresponding to the midline of the abdomen; this impacts abdominal wall functions causing associated muscle imbalance and chronic pain of the thoracoabdominal dorsal region. It can also produce aesthetic alterations of the body contour, in addition, it can generate musculoskeletal pain, urological and gynecological symptoms and low self-esteem in the patient [22].
Among the clinical consequences that may occur after RD, lumbar pain without other apparent causes (70.2%) and pelvic floor dysfunction are reported. It is necessary to know that the internal oblique and transverse abdominis muscles continue in the anterior and medial leaf of the thoracolumbar fascia. The tension generated by the oblique-anterior abdominal muscles maintains a physiological lumbar lordosis, whose main purpose is to reduce the tension exerted by the extensor muscles of the back [1]. For this reason, through this fascia a complex mechanism of counterweights between the anterolateral abdominal wall and the paravertebral muscles is achieved in order to regulate the thoracic kyphosis and lumbar lordosis of the spine that allows maintaining a correct posture during standing [6].
When the interrectal distance is very wide, the tension between both rectus muscles is lost, causing an increase in the angles of thoracic kyphosis and lumbar lordosis, generating pain due to increased pressure on the intervertebral discs, especially in the lumbar region [1,6]. The abdominal cavity has limits, which are the diaphragm superiorly, the pelvic floor inferiorly, the lumbar spine posteriorly and the anterolateral abdominal wall: Represented by the broad abdominal muscles and the anterior rectus abdominis muscles. It reflects the Valsalva maneuvers, a vector that is directed towards the posterior region of the perineum and sacrum [1], this can generate low back pain, when there is imbalance or associated decrease in the strength of the anterior and posterior muscles of the trunk, lumbopelvic instability and pelvic floor weakness [1,15,17].
Biomechanics of the abdominal wall
DR can produce pelvic floor dysfunction, the patient can acquire stress and urge incontinence, genital prolapse, as well as pelvic pain. These conditions occur because the abdominal wall suffers a decrease in tone when the rectus muscles separate, causing displacement of this vector in the Valsalva maneuver towards the anterior area of the perineum. This phenomenon favors the pelvic floor muscles to become hypotonic generating such symptoms [1].
From the psychological point of view, an observational study by Vicente-Campos et al. 2023, showed that, in terms of body image, the women openly stated that they considered their bodies to be unaesthetic, which led to a significant decrease in their self-esteem, presenting feelings of shame towards their bodies and, in particular, towards their abdomen. In this regard, the quantitative analysis showed that 75.8% changed the way they dressed and 82.7% considered their bodies unattractive. In addition, 40.6% reported that they avoid looking in the mirror because they are disappointed by the image they see and 58.2% stopped going to the beach because of embarrassment [7].
On the other hand, the patients reported gastrointestinal problems, such as flatulence (79.2%), abdominal heaviness (55.7%), difficult digestion and bloating (84.6%), slow transit (1.7%), meteorism and constipation, although this aspect has been little investigated in the literature. The possible relationship between DR and gastrointestinal symptoms may be due to the importance of the abdominal wall in digestive function, which serves as a support for the abdominal viscera, preventing their herniation and also intervenes in defecation [7]. It is convenient to highlight that in relation to sexual function, a percentage of women with DR (31.7%) manifested reduced sexual activity and this implication has also not been studied much in the literature to date [7].
An observational, comparative, non-interventional study by Zhu et al. 2024, at the Hangzhou Hospital of Traditional Chinese Medicine, involving 534 women, showed that the rates of severe pelvic girdle pain during pregnancy differed significantly between the groups with and without DR (P=0.041). Whereas, the rates of pelvic girdle pain before pregnancy and the postpartum period did not differ between the two groups (P>0.05) [23].
In turn, the frequency of low back pain did not differ between the groups with and without RD during the pre-pregnancy, pregnancy and postpartum periods (P>0.05) and pelvic floor symptoms, including urinary incontinence, frequent urination, sexual dysfunction and chronic pelvic pain, from pregnancy to the postpartum period, did not differ between the groups with and without RD (P>0.05). Likewise, they observed that, in some women, waist and hip circumferences were modified due to gravity after changing from a supine to a standing position, thus suggesting postural differences in waist and hip circumferences [23].
Diagnostic
DR is easily recognized on physical examination, so it is postulated that the diagnosis is eminently clinical and imaging studies only support the suspicion [3,17]. In clinical practice, several measurement methods are used for the width of the linea alba, such as the easy and feasible "finger-width" method, tape measure and calipers [8]. Measurements of the distance between the rectus abdominis muscles can be performed at rest and during muscle contraction at different levels along the linea alba pathway to discern in this way whether they are normal or not [17].
Palpation methods (including calipers, tape measures and finger widths) can be clinically challenging and require a standardization protocol; for example, knowing the width of the examiner's fingers in cm or mm [24]. It is important to mention that in certain individual conditions (e.g., obese patient), the use of imaging studies will be necessary to demonstrate linea alba enlargement, because the influence of subcutaneous fat thickness may be a confounding factor [17,24].
In addition, ultrasonography, computed tomography or magnetic resonance imaging to measure Donor Risk Index (DRI) is more accurate and can exclude any concurrent ventral herniation [25]. Ultrasonography is now considered a reliable and well-established method for pregnant and postpartum women due to its widespread clinical use and lack of radiation [8]. It has been named the gold standard for noninvasive and repeatable DRI evaluation in all patients, which can be used to confirm DR, as well as to exclude other causes that weaken the abdominal wall [17,24].
Abdominal Computed Tomography (CT) is an established method in the diagnosis of the abdominal wall in samples with a wider range of patients [8]. It can be used to accurately determine the rectus distance and better define the abdominal wall anatomy, although it may underestimate DR compared to intraoperative measurements [8,17]. Magnetic Resonance Imaging (MRI) can be used, however, it is not common for evaluating the anterior abdominal wall and if requested should be specified to be non-contrast and with a focus on anterior soft tissue [17].
The reported prevalence of DR or increased DRI varies and may be inaccurate due to different cut-off points for diagnosis and the use of different measurement methods. Most prevalence studies are based on palpation or calipers, which may be less reliable than ultrasonography [26]. However, despite a correct preoperative evaluation, the definitive diagnosis and the one that will command decision making is ultimately intraoperative [27].
Treatment
The treatment of DR is a multidisciplinary pathway in which surgery alone accounts for 50% and the other 50% depends on other disciplines [6]. The two main therapies used in the correction of DR are physiotherapy and surgery [1]. As initial management an alternative could be conservative treatment with the aim of strengthening the abdominal musculature [1,4], the same includes abdominal binder, electrical stimulation, manual therapy and therapeutic exercises, being exercise the most used modality by therapists to address DR, while abdominal binders can provide physical support to the abdominal wall when used in the early postpartum period [8].
In the absence of efficacy of conservative treatment, with high aesthetic and/or functional discomfort or presence of hernia, surgical intervention is usually resorted to [5]. In turn, surgical repair of the abdominal wall should be considered in patients with an interrectal distance of more than 3 cm [5]. The surgical option for repair of DR can be by abdominoplasty or laparoscopy, which restores the abdominal wall anatomy, providing good long-term results and patient satisfaction [2,4]. If DR is associated with midline hernias (umbilical and/or epigastric), due to progressive fascial laxity, concomitant surgery would be the most valid option [5,18].
Therefore, once diagnosed, it is classified according to Nahas 2001, into 4 types according to their characteristics and a different technique is proposed for each one, as shown in Table 2 [1,28].
| Nahas y Cols | Characteristic | Treatment |
|---|---|---|
| Type A | Secondary to pregnancy | Anterior rectus sheath plication |
| Type B | Lateral and infraumbilical laxity after diastasis correction | L-plication of the external oblique aponeurosis with correction of the rectus sheath |
| Type C | Congenital lateral insertion (at costal edges) of the rectus muscle | Plicatura of the posterior rectus sheath and posterior closure of anterior sheath in the midline |
| Type D | Rectus diastasis and poorly defined waistline | Rotation of the external oblique with plication of the anterior rectus sheath |
Table 2: Nahas classification for diastasis recti. Source: Teran et al. [1].
Plication of the rectus muscles reconstructs the correct vector geometry of the abdominal muscles, restoring the conditions necessary for correct intra-abdominal pressure and the right value of the previously mentioned angles; moreover, it is the most performed technique to date and the first described, usually in the context of an abdominoplasty to reduce abdominal contour [1,6].
Other surgical techniques employed include endoscopic plication of the rectus sheath Reparación Endoscópica Preaponeurótica (REPA), which is a technique that consists of insufflating gas at the supraaponeurotic level by inserting a 12 mm trocar suprapubically and two 5 mm trocars in the iliac fossa and performing a plication of the anterior rectus sheath after correcting possible hernias, if any, with eventual placement of a reinforcement mesh and even possible unloading in the aponeurosis of the external oblique in those diastasis of more than 10 cm. Laparoscopic plication of the rectus sheath and transverse plication of the rectus sheath can also be performed [1].
Brendel and Mascaró 2020, conducted a retrospective, observational and descriptive study of 10 patients with a diagnosis of ventral hernia (including supraumbilical, infraumbilical and/or umbilical hernia) associated with DR. Their study concluded that the technique presented for repairing ARD associated with midline hernia is a simple procedure, with a short learning curve, replicable and with little likelihood of morbidity. The follow-up period of the patients was 6 months, in which there were no recurrences of ventral hernias or DR, as well as reports of other complications, so the procedure is considered an effective therapeutic option, with a decrease in recurrences and without entering the abdominal cavity [2].
With regard to laparoscopic plication of the rectus sheath, pneumoperitoneum is performed through the placement of a 10 mm trocar suprapubically and two 5 mm trocars in both iliac fossae. Among the main problems of this approach are the typical complications of laparoscopic surgery, in addition to adhesion formation, intestinal perforation and postoperative neuralgia [1].
On the other hand, when longitudinal plication is performed, we only achieve a shortening of the linea alba without correcting this laxity. Furthermore, from an aesthetic point of view, longitudinal plication only achieves a concavity in the lateral contour of the waist without maintaining the original shape of the anterior aspect of the abdomen. A surgical option to achieve both objectives may be to perform a transverse shortening of the rectus sheath [1].
Another technique, such as Laparoscopic Intracorporeal Rectus Aponeuroplasty (LIRA), described by Gómez-Menchero et al. 2018 [29]. It has as an advantage that an approximation of the fascia can be performed, with repair of the hernial ring and midline, without opening the linea alba. It consists of reducing the hernial content and eliminating the preperitoneal fat adhered to the posterior fascia of the rectus. Next, the posterior fascia of the aponeurosis of the anterior rectus muscles is opened at a distance equivalent to the defect to be reinforced. Then these aponeuroses are sutured with a continuous suture and finally a double-sided mesh is placed along the entire suture with margins, since in all meshes there will be a posterior retraction [30].
There are hybrid techniques, which are those designed to correct both diastasis and concomitant hernias. The advantages of this technique are the minimal incision made, which improves esthetics, avoids the complications of laparoscopy and makes it possible to repair large defects. However, it is a highly complex technique and involves a long operative time [1]. Along the same lines, another laparoscopic option known as MILOS has also been published by Reinpold in 2013, but it involves a highly complex process and requires high learning and technology [13].
Intraoperative and postoperative complications include pain, wound infections, hematomas, seromas, mesh extrusions, recurrence, vasomotor changes, skin burns, nerve injuries, pneumonia, minor dehiscence, umbilical site infection, complex scar, skin necrosis, contour abnormalities and visceral injury, numbness or paresthetic sensations in the abdominal skin; these differ with each patient's operation and with the different techniques used, according to the literature [10,18]. Persistent loss of sensation due to nerve injury has been reported after procedures involving abdominoplasty [26].
It is important to emphasize that both conservative and surgical treatments are aimed at improving the morphological, functional and quality of life of patients [10]. In the approach to diastasis by health professionals, attention should be paid not only to the purely anatomical measurement of the interrectal distance, but also to the psychological and social consequences of diastasis [7].
The repair of rectus diastasis recti has evolved over the last few years and minimally invasive approaches now represent the first choice to treat it, even when associated with midline hernias. Most of these techniques involve plication of the anterior or posterior rectus fascia to approximate the midline muscles or (more recently) the use of a linear endoscopic stapler to divide the anterior and posterior fascia and join the left and right fascia, such as a rives replication, stoppa technique. Likewise, studies have demonstrated advantages of the minimally invasive approach to abdominal wall repair, in terms of recurrence rates, complications and outcomes, hospital stay, cosmetic results and even pain relief [31].
Conclusion
Diastasis recti is a condition that can occur in both men and women, usually occurs asymptomatically and have great repercussions beyond the aesthetic as low back pain, pelvic floor dysfunction, musculoskeletal pain, urological symptoms, gynecological and gastrointestinal symptoms and even related to sexual function, so the preventive diagnosis is a guarantee that it is considered and treated in a timely manner, since a strangulation by hernia of the linea alba is catastrophic and can compromise life.
Acknowledgement
We thank our Student Community for the Dissemination and Research of Human Anatomy (CEDIAH), University of Zulia, Maracaibo, Venezuela.
References
- Teran JIU, González AZ, Pérez-de-Villarreal Amilburu P, Ferreras AIG, Salgado LHO, et al. (2020) Consequences and treatment options in rectum diastasis. A treatment algorithm suggestion. Revi Hispanoa Herni 8: 65-71.
- Brendel SR, Mascaró J (2020) Ventral hernia repair associated to diastasis of rectus abdominis muscles by endoscopic approach. Preliminary results. Rev Hispanoam Hernia 8: 115-121.
- Cuenca O, Rodríguez A, Segovia A (2017) Endoscopic approach of rectus diastasis and abdominal midline defects. Rev Cir Parag 41: 37-40.
[Crossref], [Google Scholar]
- Cañamero de León S, Da Cuña Carrera I, De la Hoz González C, González MS (2020) Comparación de los efectos de un programa de ejercicio sobre diastasis de rectos según el periodo postparto. Medicina Naturista 14: 53-58.
- Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K (2018) Diastasis recti abdominis a review of treatment methods. Ginekol Pol 89: 97-101.
[Crossref], [Google Scholar], [Indexed]
- Cuccomarino S (2019) Why an abdominal wall surgeon should operate a diastasis recti? Rev Hispanoam Hernia 7: 43-46.
- Vicente-Campos V, Fuentes-Aparicio L, Rejano-Campo M (2023) Evaluation of the physical and psychosocial consequences of the diastasis of the rectus abdominis and its interference in health: A mixed study. Rehabilitación 57: 100744.
[Crossref], [Google Scholar]
- Kaufmann RL, Reiner CS, Dietz UA, Clavie PA, Vonlanthen R, et al. (2022) Normal width of the linea alba, prevalence, and risk factors for diastasis recti abdominis in adults, a crossâ??sectional study. Hernia 26: 609-618.
[Crossref], [Google Scholar], [Indexed]
- Çintesun E, Çintesun FNI, AydoÄ?du M, BayramoÄ?lu D, Çelik C (2021) Effect of re-approximation of the rectus muscles on diastasis recti abdominis at cesarean section-a prospective cross-sectional study. Ginekol Pol 92: 132-136.
[Crossref], [Google Scholar], [Indexed]
- Radhakrishnan M, Ramamurthy K (2022) Efficacy and challenges in the treatment of diastasis recti abdominis-a scoping review on the current trends and future perspectives. Diagnostics (Basel) 12: 2044.
[Crossref], [Google Scholar], [Indexed]
- Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O (2019) Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open 3: 750-758.
[Crossref], [Google Scholar], [Indexed]
- Cavalli M, Aiolfi A, Bruni PG, Manfredini L, Lombardo F, et al. (2021) Prevalence and risk factors for diastasis recti abdominis: A review and proposal of a new anatomical variation. Hernia 25: 883-890.
[Crossref], [Google Scholar], [Indexed]
- Murray JAB (2017) Surgical technique to repair diastasis recti associated with umbilical hernia. Ten years of experience. Rev Hispanoam Hernia 5: 52-56.
[Crossref], [Google Scholar]
- Muas DMJ, Palmisano E, Santoja GP, Cuccomarino S, Higuera GG, et al. (2019) Preaponeurotic endoscopic repair (REPA) as treatment of the diastasis of the recti associated or not to hernias of the middle line. Multicenter study. Rev Hispanoam Hernia 7: 59-65.
- Scarafoni EE, Pomerane AL, Sereday CE (2020) State-of-art of rectus shealth plication. Rev Argent Cir Plást 26: 23-30.
- Rath AM, Attali P, Dumas JL, Goldlust D, Zhang J, et al. (1996) The abdominal linea alba: An anatomo-radiologic and biomechanical study. Surg Radiol Anat 18: 281-288.
[Crossref], [Google Scholar], [Indexed].
- Bolívar-Rodríguez MA, Gaxiola-López CI, Servín-Uribe SD, Cázarez-Aguilar MA, Morgan-Ortiz F (2023) Diastasis of rectus abdominis muscles. Literature review diastasis of rectus abdominis muscles. Literature review. Rev Med UAS 13: 74-89.
- Nahabedian MY (2018) Management strategies for diastasis recti. Semin Plast Surg 32: 147-154.
[Crossref], [Google Scholar], [Indexed]
- Ferrerosa de la Rosa GA, Ibarra CEH, Mosquera SA (2022) Effectiveness of the use of absorbable suture in the plication of diastasis recti abdominis in abdominoplasty for post-bariatric patients. Rev Col Cirugía Plástica y Reconstructiva 28: 7-14.
- Weinger I, Kozinc Z, Šarabon N (2023) The efects of conservative interventions for treating diastasis recti abdominis in postpartum women: A review with metaâ??analysis. SN Compr Clin Med 5: 10.
[Crossref], [Google Scholar], [Indexed]
- Medina JP, Busnelli G, Cerutti RR, Pirchi DE (2019) Subcutaneous endoscopic repair of diastasis recti and other midline defects. Rev Argent Cir 111: 20-26.
[Crossref], [Google Scholar]
- Fernandes da Mota PG, Pascoal AGBA, Carita AIAD, Bø K (2015) Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther 20: 200-205.
[Crossref], [Google Scholar], [Indexed]
- Zhu Y, Jiang L, Ye T, Liu Y, Sun L, et al. (2024) Risk factors and patient-reported outcomes in Chinese women with postpartum diastasis recti abdominis: An observational study. Int J Womens Health 16: 179-192.
[Crossref], [Google Scholar], [Indexed]
- Werner LA, Dayan M (2019) Diastasis recti abdominis-diagnosis, risk factors, effect on musculoskeletal function, framework for treatment and implications for the pelvic floor. Current Women’s Health Reviews 15: 86-101.
[Crossref], [Google Scholar]
- SuÅ?kowski L, Matyja A, Osuch C, Matyja M (2022) Diastasis Recti Abdominis (DRA): Review of risk factors, diagnostic methods, conservative and surgical treatment. Clin Exp Obstet Gynecol 49: 111.
[Crossref], [Google Scholar]
- Carlstedt A, Bringman S, Egberth M, Emanuelsson P, Olsson A, et al. (2021) Management of diastasis of the rectus abdominis muscles: Recommendations for Swedish national guidelines. Scand J Surg 110: 452-459.
[Crossref], [Google Scholar], [Indexed]
- Macchiavello M, Arriagada C, Hurtado M, Wosiack A, Flores N, et al. (2023) Presentation of a new classification of plications in abdominoplasty. Cir Plást Iberolatinoam 49: 117-128.
- Nahas FX (2001) An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg 108: 1787-1795.
[Crossref], [Google Scholar], [Indexed]
- Gómez-Menchero J, Guadalajara JJF, Suárez Grau JM, Bellido Luque JA, García Moreno JL, et al. (2018) Laparoscopic Intracorporeal Rectus Aponeuroplasty (LIRA technique): A step forward in minimally invasive abdominal wall reconstruction for Ventral Hernia Repair (LVHR). Surg Endosc 32: 3502-3508.
[Crossref], [Google Scholar], [Indexed]
- Maillo C, Serralheiro, Piçarra G, Oliveira M, Abreu RC, et al. (2023). Laproscopic repair of umbilical hernia and diastasis recti by LIRA technique. Revista Portuguesa de Cirurgia 56: 991.
[Crossref]
- Cavallaro G, Gazzanelli S, Iorio O, Iossa A, Giordano L, et al. (2023) Laparoscopic transversus abdominis plane block is useful in pain relief after laparoscopic stapled repair of diastasis recti and ventral hernia. J Minim Access Surg 19: 207-211.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences