Dialysis Technology and the Quality of Treatment
Thomas Ryzlewicz*
Sonnering 31, D – 83129 Hoeslwang, Germany
- *Corresponding Author:
- Thomas Ryzlewicz
Senior Consultant, Nephrologist, Sonnering
31, D – 83129 Hoeslwang, Germany
Tel: +49 172 836 66 25
E-mail:thomas.ryzlewicz@web.de
Received: June 21, 2018; Accepted: July 24, 2018; Published: July 30, 2018
Citation: Ryzlewicz T (2018) Dialysis Technology and the Quality of Treatment. J Nephrol Transplant. Vol.2 No.1:3
Abstract
Different developments had appeared in the long-term of decades of dialysis treatment. Their contribution to an improvement of the therapeutic treatment will assess. The purpose of this review is, to show the shortcoming of the applications of these different parts of dialysis equipment. Concerning the under mentioned themes, there appeared shortcoming of understanding as an important problem. An improvement of the treatment’s efficacy seems conceivable, when these themes will think-over by the leadership of a dialysis centre. This also will include the level of providers, as some themes have not well understood by the majority of medical doctors (e.g. economics, chemical solubility of the dialysis fluid). A provider can seek advice by an independent specialist. By this, a better use of the technical facilities must not be more expensive.
Keywords
Dialysis; Transplantation; Anti-fibrinolytic drug; High-flux membrane; Ultrafiltration
Introduction
Vascular access
Cimino published his experience 1962 to perform haemodialysis, using two veins. Later on, the AV-fistula at the forearm was his idea [1]. The very first Cimino fistula had realised by Appel, as he had the outstanding skill to stitch these small vessels together to create an anastomosis with a diameter of 3 mm (side-toside anastomosis). This had published 1966 in the New England Journal of Medicine [2]. M. Brescia was the senior consultant, so his name appeared also in this paper. In 1967, the end-toside anastomosis had created by the both. This vascular access was decisive for the spreading of the dialysis in many countries, beginning as home-haemodialysis. Later-on, vascular grafts (PTFE) had used, when the patient had no qualified own vessels. The superior quality of the AV-fistula had shown the DOPPS report concerning long-term treatment with dialysis and the avoidance of a sepsis (as there is no synthetic material inside a classical AVFistula). 35 years later, a bigger part of the dialysis in the US had used synthetic material with the results of the shorter durability, the risk of a sepsis in case of an infection. That’s why K. Konner had re-introduced Cimino’s AV-fistula in the US at the ASN kidney week in 2003 [3,4].
Tunneled catheters as vascular access for dialysis
Francis of Royal Free, London in 1982 had introduced this. His first patient had provided for living-donor transplantation [5]. In order to reach the best possible state of his condition, this new catheter (combination of Shaldon’s catheter with the top of the Tenckhoff) had used for about five month, a limited time. There was no use-up of vessels, as this was a younger patient. There was complete sterile handling, two nurses, one sterile and the other had handed the sterile material. Today, the non-touchtechnique had introduced as a qualified way of sterile handling.
The problem of today is that a bigger part of patients will never introduce to the vascular surgeon (e.g. Narender Goel, Montefiore Medical Centre, New York, and lecture in Baltimore September 14th, 2015). Results of DOPPS report had clearly shown, that the infective problems of atrial catheters will reach even patients with limited perspective of health (> patients with tumour or very high age). Another difficult point is the qualified installation of an atrial catheter. A sufficient blood flow of the atrial catheters is an essential problem, due to the way of installation (!). Worst case is than a treatment with an antifibrinolytic drug in order to overcome a bad placed tip of the atrial catheter.
A last point: To times of Scribner’s shunt, an inserted lengthening of the line had used, in order to handle not direct at the implanted part of the patient. This inserted lengthening was also successfully used in the peritoneal dialysis up today, introduced by Twardowski. In catheter haemodialysis, it seems that everything will be allowed [6]. Single lumen catheters will use a Y-part. This does work as inserted lengthening for working with a distance to the implanted catheter. Very often, an AV-fistula is the best option for the CKD-5 patients. If there is the state of poor vessels, than a qualified shunt surgeon will required, working in a shuntcentre. This is no serious questions of costs. It only will cost to overcome elevated miles.
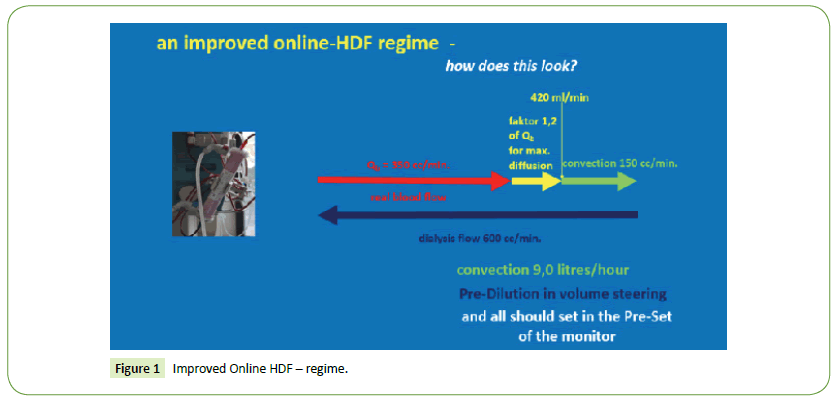
High-Flux: Low-Flux
No doubt, high-flux membranes have superior qualities concerning biocompatibility. This derives from the synthetic structure instead of the old dialyzers of regenerated cellulose/ Cuprophan. Due to the high ultrafiltration coefficient, highflux disposables had constructed for convective therapy (>hemofiltration, later-on haemo-diafiltration). In 1978, the first monitor with volume steering had appeared. This was a necessary requirement but no sufficient condition for the hygienic condition with unsterile dialysis fluid (>the internal filtration). There was no bigger consideration to the synthetic low-flow, whenever two big studies (HEMO and MPO, both prospective randomised, each of them with 5000 patients) had shown no better survival for the high-flux group. With high-flux dialyzer, the internal filtration will reach 12-14 litres within a treatment time of 4:00 hours. Even 17 litres convection (results of the Turkish online-HDF study) (Figure 1) failed concerning an improved survival! This context will be neglected continuously! But the high-flux had promoted by the industries! There was hope and belief to the absorption facilities of the synthetic high-flux membrane. This had clarified by the ISO norm 11663 from 2009: One ultrafilter is necessary for high-flux dialysis [7,8].
The Luer-Lock
The clinical dialysis had come from the US (Seattle, Scribner) after 1960. In the late 1960-ies, plate dialyzers (regenerated cellulose) had appeared. With this set-up, there was no de-airing problem, as the total air had collected in the venous expansion chamber (without air-trapping). In 1978, the first capillary high-flux disposables appeared (at first for Hemofiltration). The Luer-Lock’s of the arterial suction side of the bloodline is not tight concerning the entry of air at the usual -150 mm Hg, an arterial expansion chamber had required, as capillary disposables will blocked by air bubbles ( important reduction of the surface  loss of efficacy). This had successful worked for many decades. The problem today is there are set-up’s on the market for capillary dialyzers without arterial expansion chamber. Or this arterial expansion chamber had placed at the wrong side (in front of the blood pump). Real de-air is only possible with an arterial expansion chamber after the blood pump. The fitting of the Luer-Lock never had improved. It appears that there had been a bigger loss of knowledge in some R&D departments (>renunciation or wrong placement of the arterial expansion chamber for dialysis with capillary kidneys) [8].
loss of efficacy). This had successful worked for many decades. The problem today is there are set-up’s on the market for capillary dialyzers without arterial expansion chamber. Or this arterial expansion chamber had placed at the wrong side (in front of the blood pump). Real de-air is only possible with an arterial expansion chamber after the blood pump. The fitting of the Luer-Lock never had improved. It appears that there had been a bigger loss of knowledge in some R&D departments (>renunciation or wrong placement of the arterial expansion chamber for dialysis with capillary kidneys) [8].
Back-armament of single-needle-technique
In 1977, K.F. Kopp had developed the SN-Technique. 10 years later, the first double pumps for SN had appeared. This had been a qualified answer concerning the efficacy of the dialysis treatment. In the long-run of this development, the intermediate store for the blood had been the plate dialyzer with its compliance of more than 100% of the dialyzer volume. With the later capillary dialyzers, two big expansion chambers had used to realize a stroke volume of 60 cc. With this set-up, real blood flow of 250 cc/min. will realize. - Another intelligent SN system is the Cross-Over too, also introduced by Kopp. The Cross-Over uses also double pumps but with a very intelligent steering of the two clamps. With the Cross-Over-SN, real blood flow of 270 cc/min will be available (> also developed by Kopp in 1984) [9]. Today, there are some monitors in the market with SN-click-clack (one blood pump only) without any intermediate Store for the blood and with the compliance of the capillary dialyzer of 0 ml! This set-up never will reach by far never a sufficient processed blood volume! - What is the advantage of a double pump SN system? Clearly spoken, in case of either limited puncture facilities or only poor possibilities of puncture, a third puncture will not force. This remains a clear advantage for the patient. The reasons? Loss of knowledge and the economics. The operation of double pump SN seems not to be the reason (> the last edition of cross-over-SN has automatic handling).
Literature Review
Citrate-acidification
Body fluid with bicarbonate in mammals and men needs an acidification of 4% of total CO2 , in order to prevent the calcification with the cations Ca++ and Mg++. These 4% of the total CO2 correspond with pCO2 of 40 mm Hg resp. 1.2 mmol/l physically solved CO2 by Homer W. Smith, “From Fish to Philosopher” in 1953 [10]. Scribner had set the prescription of bicarbonate dialysis fluid to 32 mmol/l in 1960, because of the short treatment time of dialysis in relation to one week living (= 168 hours per week). The prescription of bicarbonate dialysis fluid of today had done since 1978 with 3 mmol/l acetate for the far most treatments. This is formal a correct calculation. The problem is that this dialysis fluid does calcify. To reduce this calcification even of the prescription, an elevation of Acetate will used (4, 5 or even more mmol/l). The problem of these concentrates with elevated Acetate is the very high pCO2 (far more than 100 mm Hg). The dialyzer is an excellent disposable for gas exchange. So this will burden the patient with limited pulmonary functions (e.g. COLD or just weaned from respirator). The monitors have to descale after every dialysis, in the most cases with 30 g Sodium-Citrate. Only the patients will not descaled! 20 years later, strong problems of calcification of coronary vessels and heart valves had recognised. Naturally, CKD-5 patients have real and strong different reasons for the calcification. This calcifying dialysis fluid (bicarbonate with 3 mmol/l acetate acidification) seems to be one additional reason that had not recognized. In 1997, Laurent reported his experience with long-term dialysis: “The Secret of Tassin” by NDT [11]. With Acetate as buffer precursor (> no bicarbonate and no acidification as all solids have a very good solubility), he had a big group of patients of 80 years with 30 years of RRT and a second group, a little smaller, aged 90 years with 40 years of dialysis. The treatment time was 24 hours of dialysis per week. What was the real secret of Tassin? Additional to the Na+ 135 in the dialysis fluid this was acetate as buffer precursor with no calcification in the prescription. For Charras and Larent, this was obvious, as this had been the every-day dialysis in Tassin. But this had not pronounced.
Using the acetate dialysis of Shaldon, Square-Metre-Hour- Hypothesis by Scribner in 1971, had introduced the shortening of treatment times. By this, blood flow of dialysis and square-metres of dialyzers had enlarged, in order to keep the Kt/V constant. With this time shortening, there had introduced a bigger Metabolic Overload of Acetate. The consequence had been the well-known side effects of discomfort of Acetate dialysis (blood pressure problems and vomiting). These side effects did not appear with normal or moderate clearance using the Acetate dialysis, as used continuously by Shaldon and in Tassin. For the majority of nephrologists there was the Cry for Bicarbonate dialysis.
There are newer studies with treatment times of eight hours per dialysis, prospective randomized. They all have a very good Kt/V. Some of them had reached an important risk reduction. The difference to Tassin is that these newer studies had done with bicarbonate dialysis with acetate acidification. By this, there is the calcification even in the prescription! When Laurent had reached happy retirement, modern dialysis monitors with bicarbonate dialysis had appeared. So the calcification had introduced, even in Tassin.
Since 2007, there are Citrate-based concentrates for bicarbonate dialysis in the market as regular and approved Medical Products (0.85 mmol/l plus 0.3 mmol/l or 1.0 mmol/l Citrate). The amount of acidification is totally the same to 3 mmol/l acetate, as Citrate is a threefold base. This means that the produced amount of soluble CO2 with Citrate-based concentrates will be equal the same as with 3 mmol/l Acetate. The advantage of citrate-based concentrate? There is a second principle of working inside, the Chelate binding. This Chelate binding disguises the cations Ca++ and Mg++. By this, these two ions are present in the dialysis fluid, but the contribution to a calcification of both to carbonate will completely impede. With the T50 in-vitro test, developed by Parsch and Meier, Lorenz and Schmaderer had actually shown the favourable reduction of calcification in the blood of dialysis patients treated with acetate-free, citrate-acidified bicarbonate dialysis after three months. When putting back these patients to the classical acetate-acidified dialysis, the T50 test had shown the inclination of calcification [12].
The assessment of the both bicarbonate dialysis prescriptions needs further chemical knowledge. Medical doctors will not understand this chelate effect of the citrate-based concentrate. The problem is that Medical Societies and Medical Authorities had casted with Medical Doctors. For Medical Products, there does not exist any vigilance. This will result in the continuation of this calcifying dialysis fluid [13]. The mourning concerning the clinical calcification problems will also continue [14]. The smaller advantages of Citrate-based concentrate will here not discuss.
To state, that these calcification problems are by far not only a theoretical problem, there is an X-Ray of a long-term CKD-5 patient (age of 47 years, 33 years with RRT, over all good condition). A secondary HPT will treated with low dosage of Paricalcitol and Cinacalcet. Never an elevation of Ca++. Long-term treatment with Sevelamer as the one and only phosphate binder. The three X-Rays show the course of the arteries without any radiopaque material. These X-Rays had done for the announcement for the third kidney transplant. No problems of reduced perfusion at hands and legs. The patient had accepted or the waiting list – without coronary arteriography. No coronary symptoms. We only can guess, how the coronary arteries may look . . . (Figure 2).
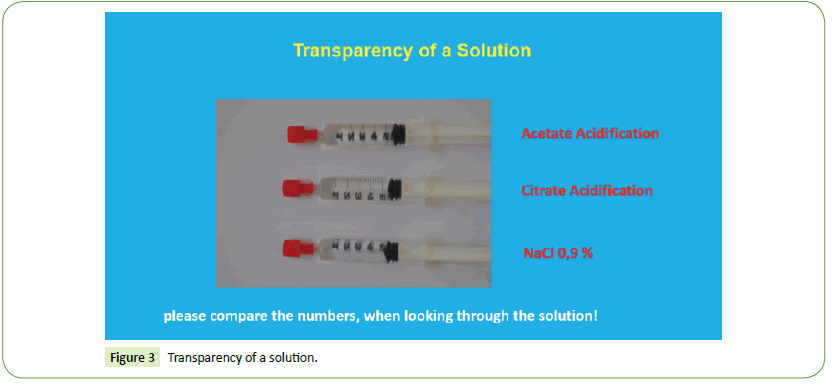
According to the approved rules of pharmacopoeia, a solution for infusion should be transparent. There are only few exceptions (>lipids, iron-infusion e.g.). For online-therapy is the dialysis fluid indeed an infusion. For the assessment of transparency, here are three syringes with different fluids. The scales of these syringes had turned back, so that you will look through the different fluid for your own assessment. You will recognise the cloudy fluid (Figure 3).
Online-HDF and the potential improved survival
In 2004, Canaud published, that there may be a longer survival, when CKD-5 patients will treat with online-HDF by Canaud, Blood Purif. in 2004, own retrospective results [15]. In 2012/2013, three well-known prospective randomised studies appeared ESHOL by Maduell in 2012, CONTRAST by Blankestijn in 2012 and Turkish Study in 2013) [16,17].
The problem: The treatment time was too short in all three studies. All of them had used online-HDF in Post-Dilution mode [18]. The poor results of the Turkish Study resulted from volume driven mode. The two other studies had used pressure driven mode (auto-processing) and an elevation of the dialysis flow due to the blood flow with far better.
ESHOL reached the improved survival, while CONTRAST failed with only small distance. The points of critics is that the predilution had not used (!). When using the litres of convection, then the Pre-Dilution will have the higher Kt/V (own results, Urea Monitor and blood sampling). At the venous half of the high-flux in Post-Dilution mode (during online-HDF), the blood will look nearly black, as it is completely exhausted. There is packed cell volume of Red Blood Cells. The small molecules (urea, creatinine) will cover longer distances for diffusion around the red blood cells as packed cell volume. Because of the higher TMP in the Post-Dilution mode, there will be a thicker secondary protein membrane as an additional diffusion handicap. The Pre-Dilution has the disadvantage of the reduction of the concentration as a principle. But this effect is smaller as the two named disadvantages of the Post-Dilution (lengthening of the way of diffusion and secondary protein membrane). Indeed, one will reach by far better results using post-dilution and auto-processing with strong elevated blood flow. But this had not done in these three studies. Naturally, not every patient has a vascular access that will allow this. The requirement for a high blood flow in Pre-Dilution will be by far not so important.
An additional point: The KUF had elevated by the industry in a large extend (> in order to improve the internal filtration at high-flux haemodialysis) [19]. The problem of today with these high-flux dialyzers is that the real convection at online-HDF had reduced by the very high KUF.
In numbers: With a surface of 2 m2, you have got a convection 20 years ago of 6.0 litres per hour resp. 100 cc/min. Today, a 2 m² high-flux will reach in online-HDF (Post-Dilution) only 5.0 litres per hour resp. 80 cc/min. The possible convection rate had reduced in Post-Dilution with auto-processing (>because of the not reasonable big elevation of the KUF in high-flux, while in Pre- Dilution (volume steering) you can easily enlarge the convection rate to 125 or 150 cc/min. (resp. 7 or 9 litres/hour)). The noncritical elevation of the KUF’s is a clear disadvantage of the highflux of today, developed by the R & D departments of the industry! Critics are one important point. It will be more successful, to show the better way of an improved online-HDF regime:
1. Treatment time 4:30 h as minimum, due to the body weight.
2. Real blood flow 350 cc/min.
3. Elevation of total dialysis flow to 600 cc/min. (> for 1.2 fold for max. diffusion and for 150 cc/min. for convection (9.0 litres/hour).
4. Mode pre-dilution (volume steering), convection rate 9.0 litres/hour (= 150 cc/min.)
5. The mode should install in the pre-set of the monitor (Figure 1).
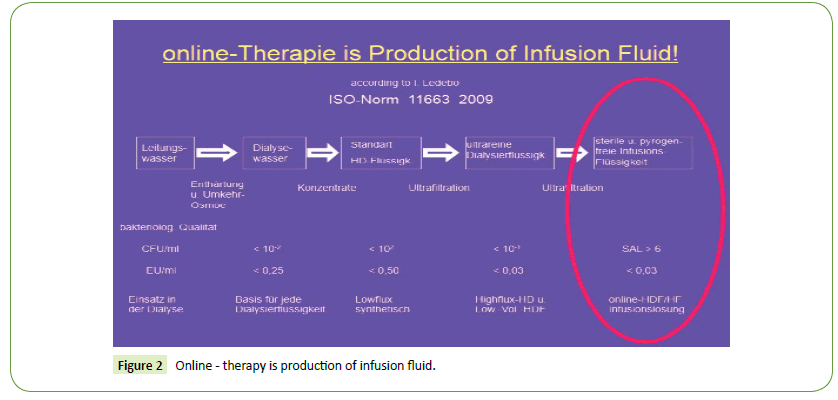
ISO Norm 11663
According to I. Ledebo and Blankestijn, NDT plus in 2009, when online-therapy had introduced, there was the big question of correct handling of the online produced infusion fluid [7,20]. This had developed to two ultra-filters in serial position. This means a sterile and pyrogen-free infusion fluid. In the flow chart of dialysis water, there appears the AMI standard (filtrate of RO water with dialysis concentrate, mixed in the monitor). AMI standard means 102 CFU/ml. With 2-step ultrafiltration, there will be a CFU reduction to 10-6 per ml (eight ten potencies). This will named sterile infusion fluid. The monitors had filled up with low percentage of Per-Acetate. At next day, this disinfection had to rinse out. The dialysis fluid had to test for potential rests of the disinfection solution.
My own critics: By the industry, the disinfection of hot citric acid over-night had “allowed”. This means that the monitor will be emptied at the end.
The problem is that both ultra-filters remained filled-up. This is standing fluid, a preferred condition for CFU growth! By this way of disinfection (> hot-citrate) the constructive facilities for onlinetherapy had weakened to the exit condition of the AMI standard (CFU 102 instead of 10-6 resp. SAL 6, Sterility Assurance Level, reduction of eight ten potencies). Because of this, the bacteriology of dialysis fluid of online monitors will no longer necessary. So we had arrived at the state of belief and hope, concerning the adsorption facilities of the high-flux, while the ISO norm 11663 (2009, and up-dated in 2013) requires sterile dialysis fluid, in terms of Ledebo CFU reduction of eight ten potencies to 10-6 [20]. Clearly spoken, The ISO norm 11663 does require the chemical disinfection. The doctor with his team remains responsible for the quality of the fluid of online monitors. What for we have the ISO norm 11663, when the way of disinfection does not fulfil the correct constructive requirements? (Figures 2 and 3).
Results
Vascular Access Monitor (VAM)
Fatal exit during dialysis happens in a smaller but continuous number over the decades. Surely, this number does not intake the supposed much bigger dark-number. The problem is the case of disconnection, when for example the needle does loose its position in the vein. There will be a reduction of hydraulic resistance. In worst case, this may not reach the lower alarm limit of the venous pressure window. In worst case scenario, there will follow a bleeding - off - without any further alarm. In one premium monitor, there had an intelligent set-up installed, that protects the patient from this potential fatal exit, the VAM.
The principle: With the arterial suction pressure-line, the quality of the vascular access will monitored continuously [21]. The patient’s arterial pressure (systolic and diastolic), the heart-rate will be analysed with a calculator. In case of a severe bleeding-off, the heart rate does definitely raise, even in case of beta-blocker medication. By this, the blood pump will stopped immediately. In my view, the manufacturer should come together to transact, that every new monitor should equipped with this VAM. The economists should find the way.
Arterial Catheters as dialysis access are a poor access. Even in high aged patients or in tumour patients they will go through infection problems. Later-on the danger to develop central venous stenosis of the big central veins. It is never a problem of costs, as the surgery of a sufficient av-shunt is a question of the quality of the vascular surgeon. And this can made some miles more. In the end, it is a question of engagement of the nephrologist, to present a CKD-4 b patient in time to a qualified vascular surgeon.
High-Flux: Low-Flux: Today, all dialyzer are synthetic. This is very good because of biocompatibility. With the internal filtration, there will be no benefit for the patients, as the total amount of this, remains poor. This is not so important, as today every monitor is equipped with one ultrafilter. The high-flux dialyzers will surely continue.
Single needle: Best option is to approach to the condition of the patient. If there is a new shunt or a nurse with limited puncture facilities, then SN equipment will make it sure, that even in a failure of puncture, two needles will satisfy. A lack of equipment for me was never a condition. If there will be only one blood pump, there will be the force to install definitely two correct placed needles. The combination of SN-click-clack with capillary dialyzer will be only a fictitious dialysis.
Discussion and Conclusion
Citrate acidification
A big theme: This may from medical doctors often not well understood! It remains essential. Medical Societies and Medical Authorities also do not understand this. There is no vigilance for Medical Products. What will remain? There will only remain the smaller number of interested doctors and the dialysis providers. If the patients will better treat, then they have a better survival. The Medical Societies may continue their mourning concerning morbidity and mortality of cardiac calcification [22]. The pilot of Lorenz and Schmaderer, using the T50 test of Parsch and Meier, will show the reduced calcification in the blood compartment of dialysis patients, when they had treated with citrate acidification [14]. This pilot had done in crossover for 2 × 3 months. This is the first time that the calcification problem of the classical bicarbonate dialysis had made evident. Further studies will be necessary.
Online-HDF: Also a big theme, many details can be handled wrong! Treatment time remains very important. The facilities of pre-dilution (volume steering) had also not well understood. For long-term patients, this is the best option. Naturally, this should be proven. A new online-HDF trail will run. The future will show these results.
ISO norm 11663
There is a remaining contradiction between this ISO norm and the handling of online-monitors (> concerning the disinfection)! There is the demand of sterility of the dialysis fluid of online monitors that cannot be reached with hot-citric disinfection overnight. The belief and hope of adsorption facilities of the ultrafilters will never be sufficient.
Vascular Access Monitor (VAM)
The VAM will prevent the potential fatale bleeding-off in case of a disconnection. The manufacturers should come together for a transaction. Every new monitor should be equipped with this.
References
- Cimino J, Brescia M (1962) Simple venipunture for hemodialysis. New Engl J Med 267: 608-609.
- Brescia M, Cimino J, Appel K, Hurwich B (1966) Chronic hemodialysis using venepuncture and surgically created arteriovenous fistula. New Engl J Med 275: 1089-1092.
- Konner K, Nonnast-Daniel B, Ritz E (2003) The arteriovenous fistula. JASN 14: 1669-1680.
- Callen R (2003) Advanced Renal Technologies (USA). Citrasate-registrated as US patent 5.252.213 and EU patent 1124567.
- Francis D, Ward MK (1982) Right arterial catheters for long term vascular access in hemodialysis patients. Lancet 2: 301-302.
- Kopp KF (1974) Die Technik der Unipunktur bei der extrakorporalem Haemodialysis. Biomed Eng 5: 187-192.
- Locatelli F, Martin-Malo A (2009) Effect of membrane permeability on survival of hemodialysis patients. JU Am Soc Nephrol 20: 645-654.
- Rose EA (2002) Effect of dialysis dose and membrane flux in maintenance hemodialysis. The New England Journal of Medicine. 347: 2019-2020.
- Kopp KF (1984) Cross-over single needle system for dialysis monitors, developer (> 2 pumps, 2 clamps, 3 expansion chambers with continuous flow, realized by B. Braun-Avitum), USA.
- Smith HW (1953) From fish to philosopher, the story of our internal environment. CIBA Pharmaceutical Products Inc, Americana.
- Laurent G (1997) How to keep the dialysis patients normotensive? What is the secret of Tassin? NDT. 12: 1104
- Lorenz G, Schmaderer C, Heemann U (2018) Acetate-free, citrate-acidified bicarbonate dialysis improves serum calcification propensity - A preliminary study. NDT 2018
- Ryzlewicz T (2018) Dialysis fluid. Nephrol Renal Dis. 3: 2-2.
- Parsch A, Meier M (2001) T50 in-vitro test to measure the inclination of calcification in the blood of humans. Biotech Start-up CALCISCON.
- Cimino J (2004) Authentic letter to K. Konner concerning begin and realisation of Cimino’s AV-fistula.
- Grooteman MP, Blankestijn PJ, CONTRAST Investigators (2012) Effect of online hemodiafiltration on all-course mortality and c outcomes. J Am Soc Nephrol 23: 1087-1096
- Ok E (2013) Turkish Online-Haemodiafiltration Study: Martality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: results from the Turkish OL-HDF Study. NDT 1: 192-202.
- Maduell F, ESHOL Study Group (2013) High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J Am Soc Nephrol.
- Ok E, Duman S (2011) Long Dialysis Study Group: Comparison of 4 and 8 h dialysis sessions thrice weekly in-centre haemodialysis - A prospective, case controlled study. NDT 26: 1287-1296.
- Ledebo I, Blankestijn PJ (2010) Haemodiafiltration-optimal efficacy and safety. NDT Plus 3: 8-16.
- Pisoni R, Young E, Held P (2002) Vascular access use in Europe and the United States: Results from the DOPPS. Kidney International 61: 305-316.
- Rivara M, Adams S (2016) Extended-hours hemodialysis is associated with low mortality risk in patients with end-stage renal disease. Kidney Int 90: 1312-1320.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences