Development of a Pharmacy Resident-Run Transitions of Care Service in a High-Risk Cardiovascular Patient Population
Christine Gillis1*, Jillian Dempsey1, Stephanie Sibicky1,2, Lina Matta1, Danika Medina3, Calum MacRae4, James Kirshenbaum4, David Faxon4 and William Churchill1
1Department of Pharmacy, Brigham and Women’s Hospital, 75 Francis Street Boston, MA 02115
2Northeastern University, Bouvé College of Health Sciences, School of Pharmacy Northeastern University 360 Huntington Ave Boston, MA 02115
3Department of Nursing, Brigham and Women’s Hospital, 75 Francis Street Boston, MA 02115
4Department of Cardiovascular Medicine, Brigham and Women’s Hospital, 75 Francis Street Boston, MA 02115
- *Corresponding Author:
- Christine Gillis
Department of Pharmacy Brigham and Women’s Hospital 75 Francis Street Boston, MA 02115
Tel: 617-732-7153
E-mail: cgillis@bwh.harvard.edu
Received date: October 04, 2018; Accepted date: October 23, 2018; Published date: October 31, 2018
Citation: Gillis C, Dempsey J, Sibicky S, Matta L, MacRae C, Kirshenbaum J, Faxon D, Churchill W (2018) Development of a Pharmacy Resident-Run Transitions of Care Service in a High Risk Cardiovascular Patient Population. J Pharm Prac Edu Vol.1:14
Copyright: © 2018 Gillis C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To describe the development and daily operations of Project PURPOSE, a pharmacy resident-run transitions of care (TOC) pilot program, in a high risk cardiovascular (CV) patient population at a tertiary academic medical center.
Summary: As part of a newly established post-graduate year 2 (PGY-2) TOC residency program at our institution, a 6 month resident-run TOC pilot service was developed for high risk CV patients. The TOC pharmacist intervention took place either prior to a patient’s ambulatory CV appointment or during the patient’s hospital admission. In both cases, the following activities were completed: best practice medication history, distribution of adherence tools, triage and resolution of medication access issues, and recommendations for drug optimization following a full pharmacotherapy review. For admitted patients, additional services included discharge medication counseling, medication bedside delivery and post-discharge phone calls. Once the patient received the pharmacist intervention either in the ambulatory or inpatient setting, the patient was followed by a TOC resident for the duration of the pilot.
Metrics collected included number of unplanned hospital readmissions, time to healthcare utilization and change in patient activation score. Additional data included number of medication discrepancies identified, percentage of therapeutic recommendations accepted by a provider, number of medication access issues resolved, patient cost savings, patient satisfaction and average length of time spent by the pharmacist on each patient encounter.
Conclusion: Project PURPOSE demonstrates how a residentrun TOC program can be utilized to expand the role of the pharmacist at a tertiary academic medical center.
Keywords
Transitions of care; Heart failure; Acute coronary syndrome; Medication reconciliation; Medication access; Discharge planning; Hospital readmissions
Introduction
Transitions of care (TOC) encompasses a vast array of resources and services supported by multidisciplinary patient care teams designed to improve the safe and timely passage of patients between different levels of healthcare and across care settings [1]. National themes observed in the current TOC process include miscommunication among health care providers, lack of risk assessment, patient follow-up, poor patient and care giver education, and increased patient financial burden secondary in increased drug costs, culminating in a lack of patient empowerment and overall dissatisfaction with the healthcare system [2-4]. To address these pitfalls, multidisciplinary TOC initiatives and tool kits have been developed to improve the quality and safety of care as patients transition from one healthcare setting to another [4-7].
As medication experts, pharmacists play a vital role in bridging the gap between inpatient and ambulatory patient care with regards to medication management, adherence, and access. Numerous multidisciplinary studies, which have included a pharmacist intervention, have demonstrated a decrease in adverse drug events (ADEs), hospital readmissions, and time to healthcare utilization [7-9]. Despite pharmacists’ proven positive impact on the TOC continuum, the question as to how to justify expansion of funding for TOC pharmacists remains unanswered, as it is difficult to quantify a pharmacist’s intervention. As a possible solution to this challenge, additional staff including pharmacy technicians, interns and residents have been leveraged to continue to support the pharmacist’s role in this evolving and growing healthcare initiative [10,11].
The purpose of this paper is to describe the development and daily operations of Project PURPOSE (Pharmacist Utilized Resources to ImProve CardiOvaScular CarE), a pharmacy resident-run TOC pilot service, focused within a high risk cardiovascular (CV) patient population at a tertiary academic medical center. To our knowledge, there are no publications to date that describe the intricacies surrounding the development and daily operations of such a service.
Site Description
Brigham and Women’s Hospital is a 793-bed university-affiliated teaching hospital located in Boston, Massachusetts. One hundred and thirty-six of those beds are reserved for patients with a cardiac-related admission diagnosis, with 24 beds located within two intensive care units and the remainder across step down units. The hospital utilized a homegrown electronic health record (EHR) system until it transitioned to Epic© in May 2015.
The pharmacy department employs approximately 200 staff members, including 90 pharmacists. Pharmacists are decentralized during the week and participate in multidisciplinary rounds; however, due to staffing limitations and concomitant individualized responsibilities, pharmacists are limited in their capacity to participate TOC activities, including discharge counseling. The pharmacy department does not currently employ a pharmacist dedicated specifically to a TOC role. A new post-graduate year 2 (PGY-2) pharmacy resident program, specializing in TOC, was developed in 2015.
Prior to the launch of Project PURPOSE, our institution had several non-pharmacy services in place that were specifically devoted to TOC initiatives. The majority of inpatient units have dedicated nurse care coordinators who assist with discharge planning for patients assigned to the unit. Additionally, the integrated care management program (iCMP), which consists of nurse case managers, follows Medicare patients who are at high risk for hospital readmission. In conjunction with these services, our institution’s outpatient pharmacy has expanded its inpatient bedside delivery program within the past year.
Watkins Cardiovascular Clinic is our institution’s ambulatory cardiology clinic located within the main hospital campus. Approximately 150 cardiologists, nurse practitioners, and physician assistants’ practice within the clinic and rotate through inpatient cardiology services. Approximately 200 to 300 patients are scheduled for visits in the clinic on a daily basis.
Service Overview
Project PURPOSE was developed in collaboration with our institution’s cardiology department as CV patients have been historically linked to high hospital readmission rates and are at increased risk for ADEs [12]. The aim of Project PURPOSE was to identify high risk patients, in either the CV ambulatory clinic or within a cardiology inpatient unit, and to have a TOC pharmacy resident follow these patients longitudinally for 6 months. Contingent upon which phase of care the patient was identified, he/she would receive the pharmacist intervention in the form of an ambulatory care visit, inpatient visit and/or post-discharge phone call.
Resident Training and Service Hours
Two TOC PGY-2 pharmacy residents were dedicated to the pilot service. In anticipation of launching the program, residents attended the Coleman Care Transitions Program training and received their certificates as care transitions coaches4. Both residents completed their PGY-1 training at BWH and had prior exposure to both the inpatient and ambulatory care settings.
Residents were available Monday through Friday from 12:00 p.m. to 4:30 p.m., excluding holidays, conference days, and paid time off to staff the service. Residents alternated between seeing patients in the ambulatory CV clinic and inpatient setting. A pharmacy practice faculty member employed by a nearby university assisted with service coverage gaps, particularly in the ambulatory setting, and PGY-1 pharmacy practice residents were paired with the faculty member and rotated through the TOC resident clinic schedule.
Defining Targeted High Risk Patient Population
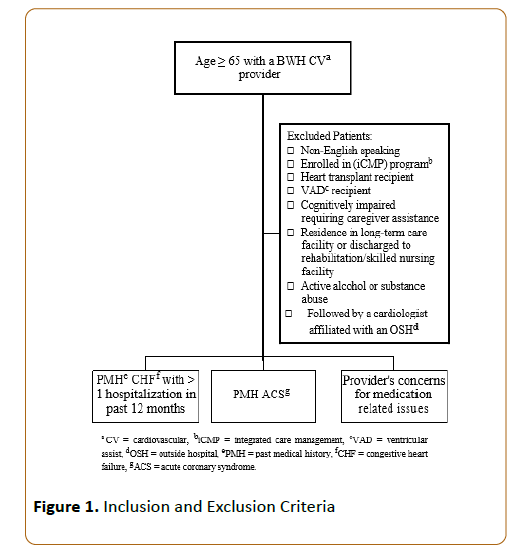
The targeted high risk patient population was defined based on previous TOC studies, CMS regulatory criteria and historical readmission rates [10,13]. However given that the pilot service was going to be run part-time by 2 residents, the expected number of patients who could be seen by a pharmacist, the service had to be focused and realistic. Following pre-pilot analysis of patient data based on CV disease states, readmission rates, and number of home and high risk medications, our target population was defined with the expectation that approximately 30 patients would be seen per week between the two residents. The targeted patient population was defined as those greater than or equal to 65 years of age with a past medical history (PMH) of heart failure (HF) and at least 1 hospital admission within the past twelve months to BWH or those greater than or equal to 65 years of age with a PMH of acute coronary syndrome (ACS) followed by a cardiologist at our institution’s cardiology clinic. Cardiologists at the institution were also able to refer patients to the service who may not have met the high risk criteria but whom the provider felt would benefit from the TOC pharmacist intervention. Refer to Figure 1 for additional information regarding service inclusion and exclusion criteria.
Patient Identification
High risk patients were identified through the EHR system. Two customized reports were built within the EHR to identify patients in both the inpatient and ambulatory care settings. Both reports screened for patient age, native language, and enrollment in the institution’s iCMP program. The reports also identified whether or not a patient met high risk criteria based on their comorbid conditions (e.g. HF, ACS). Additional manual screening via chart review had to be completed by the residents to finalize eligible patient lists for the day given that the EHR reports were not able to capture all inclusion and exclusion criteria items. Refer to Appendix A for additional details regarding the computer-generated reports.
TOC Pharmacist Intervention
As previously stated, the TOC pharmacist intervention may have been completed through an ambulatory clinic visit, inpatient visit, and/or post-discharge phone call. During the ambulatory and inpatient visits, the following activities were completed as time permitted: best practice medication history, distribution of adherence tools including pill boxes and/or medication grids, triage and resolution of medication access issues, and recommendations for therapy optimization following a full pharmacotherapy review [14]. For inpatient visits, additional services included review of discharge medication list, discharge medication counseling and education, medication bedside delivery and post-discharge phone calls. Care transitions coaching was utilized throughout the intervention and an assessment of patient activation was performed by the TOC pharmacist during each visit (cite). The Patient Activation score was developed by the Coleman group and is used to assess the patient’s ability to identify red flags, manage their medications and complete follow-up visits 4. Medicare Part D reviews were also performed for eligible patients during Medicare open enrollment (October through December). Additionally, the TOC pharmacy residents discussed prescription insurance plan options for cost savings with patients when applicable.
Operational Workflow
Ambulatory Clinic Visits: The residents alternated running the ambulatory EHR report once a week in anticipation of the following week’s clinic schedule. The resident assigned to the ambulatory clinic for the day called patients who met high risk criteria and were scheduled to see their cardiologist during the afternoon hours the following day. Residents utilized a telephone script to call patients asking them to arrive to clinic 30 to 45 minutes prior to their appointment time and to bring all of their medications. Once the patient confirmed that he/she was interested in the service and able to arrive to clinic early, the resident e-mailed the provider to inform them that their patient would be seeing a TOC pharmacy resident prior to their appointment. Once the patient was seen by the resident in clinic, the medical assistant provided the patient a survey to fill out while waiting to see their provider to assess their experience with the pharmacist.
Inpatient Visits: The inpatient report was run Monday through Friday at 7:00 a.m. by the resident assigned to the inpatient setting for the day. When the report was run on a Monday, patients who were admitted within 24 hours took priority over those who were admitted over the weekend beyond 24 hours.
Once the newly admitted patients were identified, the resident would contact the nurse to set up a time for an admission visit during the afternoon. An assessment of possible discharges for the day would also need to be completed by the resident to prioritize which patients would need discharge counseling, assistance with medication access and bedside delivery of medications.
Post-Discharge Phone Calls: The resident who saw the patient prior to discharge from the hospital would perform a postdischarge phone call 48 to 72 hours following discharge. Phone calls provided additional follow-up as needed and were made as time permitted.
Patient Tracking
Patients were tracked utilizing a shared patient list created within the EHR (Appendix B). Patients were added to the list once he or she was seen by a pharmacist for the first time, either on hospital admission or in the ambulatory clinic. The list identified patients in real time who presented either to the BWH emergency room or were admitted to the institution. The residents utilized this list as a source of communication and prioritization of work as it highlighted admitted patients who were being followed by the service. The list notified the residents of expected discharge dates and when discharge summaries were signed by providers.
Resident Communication with Care Team
Communication with patients’ care teams was completed primarily through note documentation in the EHR. Residents documented each patient encounter using a template note designed to capture the TOC pharmacist interventions and recommendations. Staff messaging within the EHR and secure emails were utilized to discuss patients.
In the inpatient setting, the TOC pharmacy resident had a face-to-face interaction with the responding clinician to notify them that the patient was being followed by the service and to discuss any outstanding issues that required follow-up. Yellow signs were placed on the patient doors to signify to the care team that the patient was being followed by a Project PURPOSE pharmacy resident. The sign provided the team with the TOC inpatient pager and instructed them to page with an anticipated discharge date and time.
In the ambulatory clinic, residents provided clinicians with a brief synopsis of the pharmacy resident’s visit with the patient prior to the provider appointment through utilization of a written provider pass-off sheet (Appendix C). The sheet highlighted key points of the pharmacist visit including identified medication discrepancies, medication adherence issues and recommendations for pharmacotherapy optimization.
Communication about the Service
As with the launch of any pilot service, communication and education regarding the role of the TOC pharmacy residents was vital to the service’s success. The residents provided various short in-services to inpatient nursing, care coordinators, cardiology clinic medical assistants and the cardiology group to educate them about the goals of the service. Business cards were distributed to staff as a reference for patients who may have benefited from referral to the service.
Metrics
Various metrics for the TOC pharmacist intervention were captured through the residents’ documentation in the EHR. Data was collected and managed using REDCap (Research Electronic Data Capture), which is an electronic data capturing tool utilized at our institution [15]. Metrics collected include unplanned 30- day hospital readmissions and time to healthcare utilization (i.e. emergency department visits). Change in patient activation score utilizing the patient activation assessment tool created by the Coleman group was utilized 4. Additional metrics included number of medication discrepancies, number of medication access issues resolved, and cost savings via medication coupon distribution, medication substitutions and Medicare Part D reviews. The number of clinical recommendations provided and accepted by providers in addition to the average time the TOC pharmacist spent on each patient encounter was recorded. Lastly, patient satisfaction was assessed in the ambulatory setting via a post-pharmacist visit survey. Refer to Appendix D for an example of the patient satisfaction survey.
Discussion
The development of Project PURPOSE highlights a few key themes in pharmacy TOC services. First, this pilot service demonstrates how ancillary support can be utilized to expand the role of pharmacy in this growing field of healthcare. Pharmacy residents are a vital resource in piloting and sustaining a program that cannot be funded through hiring additional pharmacy staff.
Additionally, the service allows the resident to foster skills such as leadership and time management by supervising the service on their own.
Second, this paper provides insight into how an EHR can be leveraged to carry out daily activities of a TOC service. Identification of high risk patients and enhanced communications are two of the barriers to sustaining TOC programs. By utilizing the EHR, identification of patient is improved and documentation lives within the patient’s health record for all of the healthcare team members to access.
Lastly, Project PURPOSE demonstrates how a TOC pharmacist can be integrated into the ambulatory and inpatient side of healthcare. The didactic nature of the intervention truly embodies the goal of a TOC service in which patients are followed through a continuum of care.
Conclusion
Project PURPOSE demonstrates how a resident-run service can be utilized to expand the role of the pharmacist in TOCrelated activities at a tertiary academic medical center. Results of the 6 month pilot have been published by Dempsey et al. in another peer review journal.
References
- Naylor M, Keating SA (2008) Transitional care. Am J Nurs 108: 58-63.
- Solet DJ, Norvell JM, Rutan GH, Frankel RM (2005) Lost in Translation: Challenges and Opportunities in Physician-to-Physician Communication During Patient Handoffs. Acad Med 80: 1094-1099.
- Snow V, Beck D, Budnitz T, Miller DC, Potter J, et al. (2009) Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J Gen Intern Med 24: 971-976.
- Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, et al. (2004) Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. J Am Geriatr Soc 52: 1817-1825.
- Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, et al. (2013) Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med 8: 421-427.
- Counsell SR, Callahan CM, Buttar AB, Clark DO, Frank KI (2006) Geriatric Resources for Assessment and Care of Elders (GRACE): a new model of primary care for low-income seniors. J Am Geriatr Soc 54: 1136-1141.
- Jack BW, Chetty VK, Anthony D, Jeffrey LG, Gail MS, et al. (2009) A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med 150: 178-187.
- Schnipper JL, Kirwin JL, Cotugno MC, Wahlstrom SA, Brown BA, et al. (2006) Role of pharmacist counseling in preventing adverse drug events after hospitalization. Archives of internal medicine 166: 565-571.
- Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, et al. (2009) Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med 4: 211-218.
- Salas CM, Miyares MA (2015) Implementing a pharmacy resident run transition of care service for heart failure patients: Effect on readmission rates. Am J Health Syst Pharm 72: 43-47.
- Kern KA, Kalus JS, Bush C, Chen D, Szandzik EG, et al. (2014) Variations in pharmacy-based transition-of-care activities in the United States: a national survey. Am J Health Syst Pharm 71: 648-656.
- Desai AS, Stevenson LW (2012) Rehospitalization for heart failure: predict or prevent? Circulation 126: 501-506.
- Services CfMaM (2012) Readmissions Reduction Program (HRRP).
- Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 10: 348-354.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377-381.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences