ISSN : 2471-299X
Medical & Clinical Reviews
Degenerative Myopia Progression: Case Report and Review
1Faculdade de Medicina da Bahia (FMB/ UFBA), Salvador, BA, Brazil.
2Escola Bahiana de Medicina e Saúde Pública, Salvador, BA, Brazil
3Clínica de Olhos Leitão Guerra, Salvador, BA, Brazil.
4Department of Ophthalmology, Universidade Federal da Bahia, Salvador, BA, Brazil.
5Department of Ophthalmology, Hospital São Rafael, Fundação Monte Tabor, Salvador, BA, Brazil.
- *Corresponding Author:
- Ricardo Luz Leitão Guerra
Clínica de Olhos Leitão Guerra, Salvador, BA, Brazil
Tel: +55-71 3525-6555
E-mail: ricardo@leitaoguerra.com.br
Citation: Guilherme MS,Cecília OS,Ricardo LLG,Roberto LM,Otacílio de OMJr, Degenerative Myopia Progression: Case Report and Review.Med Clin Rev. 2015, 1:1. doi: 10.21767/2471-299X.1000002
Copyright: © 2015 Guilherme MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Degenerative myopia or pathological myopia is a rare subtype of high myopia, which affects about 2% of the general population. It is characterized by a progressive expansion of the eyeball without stabilization of the axial length in adulthood, causing a progressive degeneration that is often associated with retinal changes that can cause severe and irreversible visual impairment. This article aims to report the evolution of the pathological findings in the fundoscopic exam in a 33-year-old woman with degenerative myopia. that has progressed within two years with decreasing visual acuity and the appearance of lacquer cracks in both eyes.
Methods and Findings: Data were collected through the analysis of a patient’s medical history at Hospital São Rafael and Hospital Professor Edgar Santos.
Conclusions: Within two years, it was observed decreased visual acuity, as well as appearance and worsening of some evidence of progression of the disease such as lacquer cracks and subretinal hemorrhage.
Introduction
The degenerative myopia is often associated with blindness and the etiology is still not clear. It is a condition characterized by the progressive expansion of the eyeball axial length which is not stabilized during the adulthood, causing a progressive degeneration [1-4]. The accelerated ocular growth is followed by scleral stretching, that will result in the formation of the characteristic findings of degenerative myopia. The etiological mechanisms are unknown, but the influence of genetic and environmental factors has been increasingly recognized [5,6].
This disease is a subtype of high myopia, which is characterized for refractive values lower than -6 diopters and axial length greater than 26,5 mm. It affects 2% of the general population. Patients with high myopia are more likely to develop degenerative conditions that range from lacquer cracks to neovascular membrane formation and retinal detachment. The progressive expansion of the eyeball leads to the formation of posterior staphyloma and degenerative changes of the sclera, choroid, Bruch's membrane, retinal pigment epithelium and neural retina. These changes result in visual impairment, changes in contrast sensibility, lower dark adaptation, visual field changes and electrophysiological changes [2,5-7].
The degenerative myopia is a medical condition of great relevance due to its large physical and socio-economic impact, as it may result in irreversible loss of bilateral central vision in workingage people [4]. The aim of this study is to report the case of a patient with degenerative myopia, highlighting the progression of pathological findings in two years.
Methods
Data were collected through the analysis of a patient’s medical history at Hospital São Rafael and Hospital Complex Professor Edgar Santos.
Results
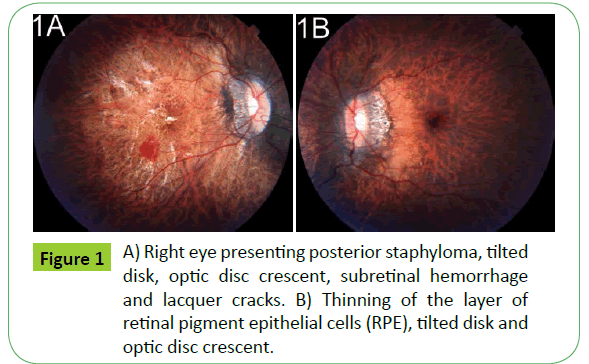
A 33-year-old female patient, from Salvador (BA)–Brazil, arrived at the Ophthalmology center of the São Rafael Hospital presenting visual impairment in 2011. The ophthalmological examination revealed best corrected visual acuity of 20/100 (-26,50 sph.-0,75 Cyl. a 150°) in the right eye, and 20/30 (18,50 sph.-1,25 cyl. a 105°) in the left eye. Fundus photography is shown below (Figures 1A and 1B).
Figure 1: A) Right eye presenting posterior staphyloma, tilted disk, optic disc crescent, subretinal hemorrhage and lacquer cracks. B) Thinning of the layer of retinal pigment epithelial cells (RPE), tilted disk and optic disc crescent.
The diagnosis of pathologic myopia was given on both eyes and the regular follow-up with expectant management was indicated.
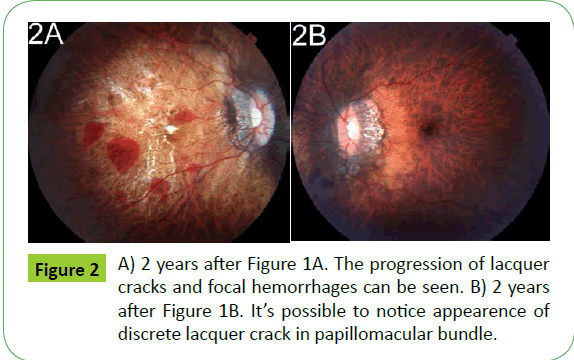
2 years later, the patient returned to São Rafael Hospital complaining about visual impairment on both eyes. The ophthalmological examination revealed best corrected visual acuity of “counting fingers” in the right eye and 20/40 in the left eye. The fundus examination can be seen in Figures 2A and 2B.
Discussion
Degenerative myopia entails diverse ocular modifications. The excessive axial growth causes a narrowing of the retina and choroid and a weakening of the sclera. This process results in the formation of posterior staphyloma, which justifies the term "degenerative". The narrowing of these structures results in a pale appearance of the fundus. The myopic maculopathy progresses in about 40% of the highly myopic eyes, and the posterior staphyloma is most frequently observed in these eyes. Some pathologic findings are tilted disk, lacquer cracks (mechanical breakages of the elastic layer of Bruch's membrane, harbinger of choroidal neovascularization), optic disc crescent (tissue traction signal), and Fuchs’ spot (last stage of choroidal neovascularization) [1,3,5,8].
The reported case presents some injuries in the fundus exam
in agreement with the literature: posterior staphyloma, tilted disk, optic disc crescent, subretinal hemorrhage, lacquer cracks and thinning of the retinal pigment epithelium. It’s possible to establish notion of progression of the condition by analyzing the evolution of such injuries in the course of two years. The presence of lacquer cracks in peripapillary region justifies the visual loss experienced by the patient. Despite the high relation described in the literature between macular choroidal neovascularization (CNV) and visual loss in patients with pathological myopia, CNV was not evidenced in this case [3,6].
Macular CNV is the main complication of high myopia and is responsible for visual impairment in many cases, especially in young and middle-aged adults, being the leading cause of vision loss in people under 50 years. Other complications include: rhegmatogenous retinal detachment, foveal retinoschisis, macular hole, cataracts, glaucoma and, less commonly, amblyopia and affections of the lens [9-11].
Although the pathophysiology is unknown, there are evidences - as the world standard for the disease distribution-indicating genetic influences. Moreover, the association of degenerative myopia and Marfan's, Ehlers-Danlos and Stickler syndrome is considered common [1,4]. In addition to the genetic influences; it is believed that there are environmental influences [2,5].
It’s also observed that the natural evolution of the condition is rather diverse. Some patients may remain stable for many years without affecting visual acuity [2].
Degenerative myopia is a challenge for the ophthalmologist because the condition requires long term medical care and comprehensive exploration during the progressive course of the pathology. Some authors suggest that high myopic patients should adopt certain measures to prevent the progression of the condition like: avoid staying in rooms with artificial lighting for long time and the importance of establishing regular medical follow-up due to their pathological condition [8].
Improvements on the understanding of the physio pathological progression/of the aspects of pathological myopia are essential. More effective and safe treatments are needed for degenerative myopia and its complications, so new treatments are being developed. Some authors believe that a genetic cure may be found. Until then, vision loss is the most common outcome of myopic macular degeneration [5,8].
References
- Yanoff M, Duker JS (2011)Oftalmologia. (4th edn), São Paulo: Editora Elsevier, pp.1552.
- Tang J, Rivers MB, Moshfeghi AA,Flynn HW, Chan CC (2010) Pathology of Macular Foveoschisis Associated with Degenerative Myopia. Journal of Ophthalmology 4: 4.
- Hayashi K, Ohno-Matsui K, Shimada N, Moriyama M, Kojima A, et al. (2010)Long-term Pattern of Progression of Myopic Maculopathy A Natural History Study. Ophthalmology117:1595-U174.
- ChooVA (2003) Look at Slowing Progression of Myopia: Solutions for this common ocular disorder might come from cellular biology. The Lancet361: 1622-1623.
- Ward B(2013)Degenerative Myopia: Myopic Macular Schisis and the Posterior Pole Buckle. Retina 33: 224-231.
- RobichaudJL, Besada E, Basler L, Frauens BJ (2011)Spectral domain optical coherence tomography of myopic traction maculopathy. Journal of the American Optometric Association82:607-613.
- Brasil OF, Brasil MV, Japiassú RM, Biancardi AL, Souza DD, et al. (2006)Fundus changes evaluation in degenerative myopia. ArqBrasOftalmol69: 2.
- Morgan IG, Matsui KO, Saw SM (2013) Myopia, Lancet 379: 1739-1748.
- Farinha CVL,Baltar A, Nunes S, Franqueira N, Henriques J, et al. (2012) Prognóstico Funcional na Miopia Patológica: História natural e resposta ao tratamento. Oftalmologia36: 1-16.
- Neves ARB (2012) Alta Miopia. Universidade Beira Interior, Covilhã-Portugal.
- Polanco SIL, Díaz REG, Rodríguez VR, Arias YG, Rodríguez WB, et al. (2012) Alteraciones del polo posterior en la miopía degenerativa. Rev. Cubana Oftalmol, Ciudad de la Habana, 25.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences