Daptomycin Induced Eosinophilic Pneumonia: A Commonly Missed Entity
Janak Adhikari1*, Priyadarshani Sharma2, Alexander Merritt2 and Saba Khokhar1
1Department of Internal Medicine, Steward Carney Hospital, Dorchester, MA, USA
2Department of Internal Medicine, Reading Hospital-Tower Health, MA, USA
- *Corresponding Author:
- Janak Adhikari
Department of Internal Medicine, Steward Carney Hospital, Dorchester, MA, USA
Tel: 8572007022
E-mail: adhikari.janak@gmail.com
Received date: March 03, 2018; Accepted date: April 18, 2018; Published date: April 27, 2018
Citation: Adhikari J, Sharma P, Merritt A, Khokhar S (2018) Daptomycin Induced Eosinophilic Pneumonia: A Commonly Missed Entity. J Clin Med Ther. 3:6.
Copyright: © 2018 Adhikari J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Eosinophilic pneumonitis is an uncommon condition characterized by fever, nonproductive cough, and progressively worsening dyspnea. Associated symptoms and signs may include malaise, myalgias, night sweats, and pleuritic chest pain. Causes include toxins, chemicals and drugs. This case highlights a case of eosinophilic pneumonitis, a rare but potential life threatening side effect of daptomycin.
Keywords
Daptomycin; Eosinophilic pneumonia
Case Presentation
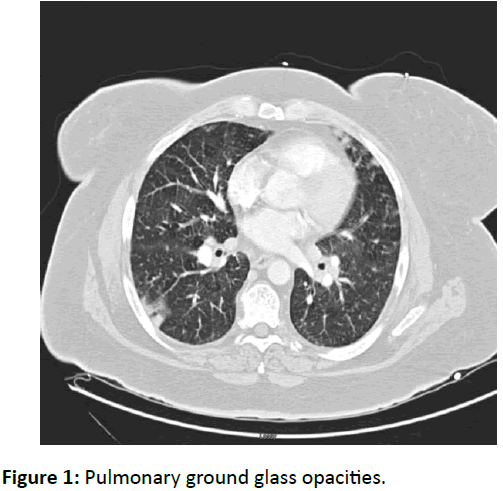
A 52 year Caucasian female with history of recurrent osteomyelitis of left great toe distal phalanx since one year presented to the emergency with shortness of breath and generalized weakness. She was being managed intermittently with debridement and vancomycin. However, 13 days back after a supratheraputic vancomycin trough level in follow up, antibiotic was changed to daptomycin for methicillin resistant Staphylococcus aureus (MRSA) coverage. Vitals on admission were remarkable for a pulse of 108/min and oxygen saturation of 88% on 2 liters. Chest auscultation revealed bi-basilar crackles, left greater than right. Left great toe was moderately tender with small ulcer and no surrounding erythema. Lab work was remarkable for white count of 18.3 (neutrophil=13.7%, eosinophil count of 7.6%). Her chest X-ray showed increased opacity within the left lower lobe consistent with left lower lobe infiltrates. CT scan demonstrated peripheral ground glass opacity with septal thickening and areas of patchy opacities within the left upper lobe, right middle lobe and bilateral lower lobes.
Daptomycin was withdrawn and she was started on vancomycin and cefepime, however she remained symptomatic for next 3 days. Repeat blood work showed white blood count of 14.8 and eosinophil of 17.7%. Work up with sputum cultures, respiratory virus panel, streptococcal/ legionella and fungal antigen testing was negative. Bronchoalveolar lavage showed eosinophil count of 2.4%. On day 4, she received intravenous methylprednisolone and later oral dexamethasone that markedly improved her symptoms over the next 12 h.
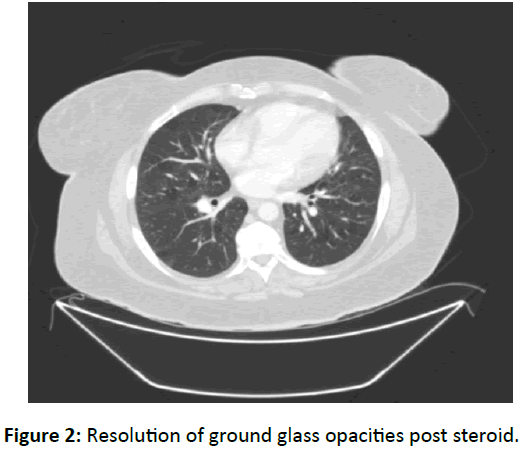
Dexamethasone was continued 2 weeks after resolution of the symptoms and then tapered. Follow up chest X-ray on day 3 after steroid initiation still showed some opacity on the left but was absent on day 7 chest X ray. Follow up CT scan in 2 weeks showed no opacities in the lungs (Figures 1 and 2).
Discussion
Daptomycin is a cyclic lipopeptide antibiotic derived from the fermentation of Streptomyces roseosporus. Daptomycin has activity against Gram-positive organisms including methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) [1]. Eosinophilic pneumonia after daptomycin is likely with the pentad of: fever, dyspnea with increased oxygen requirement, new infiltrates on chest x-ray or computed tomography (CT) scan, bronchoalveolar lavage (BAL) with>25% eosinophils and clinical improvement after daptomycin withdrawal [2]. Associated symptoms and signs may include malaise, myalgias, night sweats, and pleuritic chest pain. Clinicians should however be aware that BAL cut off value for eosinophil may be too strict on certain situations.
Conclusion
Daptomycin induced eosinophilic pneumonia is an uncommon condition characterized by fever, nonproductive cough and progressively worsening dyspnea. Prompt recognition, initiation of steroids and cessation of daptomycin will rapidly improve the symptoms and avoid unnecessary intubation and clinical decline.
References
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences