Chondromyxoid Fibroma of the Fibular Shaft: A Case Report
Alion Badar Diouf*, Dembele B, Diop M, Thiam I, Daffe M, Sarr L, Sidibe M, Diouf PA, Dione AB and Dieme CB
Orthopedics Traumatology Aristide Le Dantec Hospital, Avenue Pasteur BP 3001, West Africa
- *Corresponding Author:
- Alion Badar Diouf
Orthopedics Traumatology Aristide Le Dantec Hospital
Avenue Pasteur BP 3001, West Africa
Tel: +002214176545
E-mail: joodiouf@yahoo.fr
Received Date: August 07, 2018; Accepted Date: October 29, 2018; Published Date: November 08, 2018
Citation: Diouf AB, Dembele B, Diop M, Thiam I, Daffe M, et al. (2018) Chondromyxoid Fibroma of the Fibular Shaft: A Case Report. J trauma Orth Nurs 2:4.
Abstract
A chondromyxoid fibroma (CMF) is an extremely rare benign tumor of long bones [1]. It usually affects the metaphyseal region of long bones, particularly near the growth plate of the proximal tibia [1]. We report the case of fibular shaft localization.
Introduction
A chondromyxoid fibroma (CMF) is an extremely rare benign tumor of long bones [1]. It usually affects the metaphyseal region of long bones, particularly near the growth plate of the proximal tibia [1]. We report the case of fibular shaft localization.
Case Report
Miss D.K, a 17-year-old girl consulted for a 2-month history of sport trauma. She presented with progressive and slightly painful swelling of the lateral aspect of her left leg. She was previously healthy, and additional signs of illness could not be found.
Physical examination showed a hard, firm, tender swelling on deep palpation and adherent to the fibula of approximately 6 centimeters in length. It was located on the lateral middle third of the left leg. Neither skin lesions nor inguinal lymph nodes were found. No other abnormalities were revealed by the full systemic review.
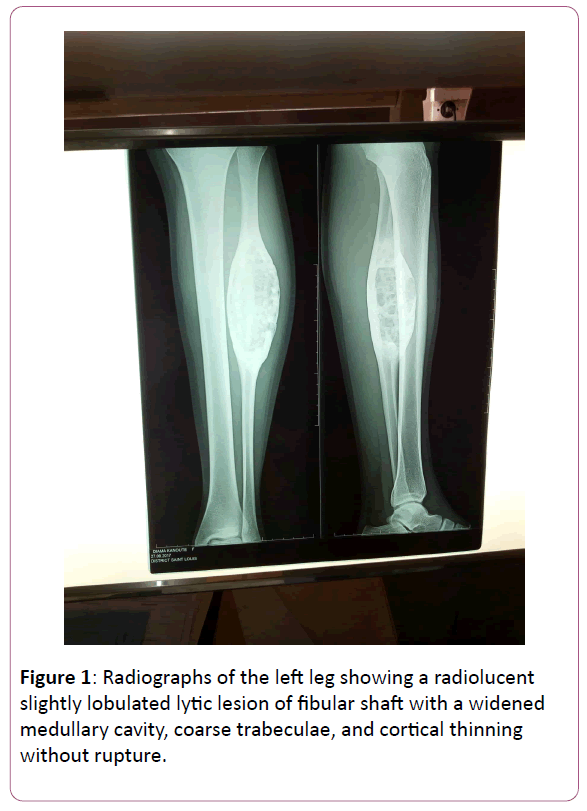
The X-ray of the leg showed the fibular shaft localization of the tumor. The radiographic appearances were those of a sharply marginated, lytic lesion in an eccentric fashion, cortical expansion and a sclerotic rim Figure 1.
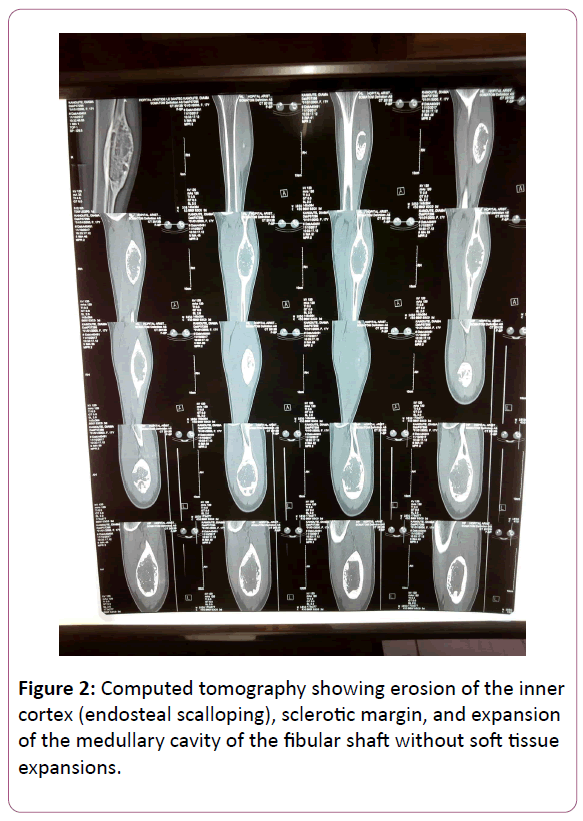
Computed Tomography scans showed a large lesion of lytic features and extended into the cortical bone, which appeared thinner and unruptured. The presumptive CT diagnosis was an enchondroma with no signs of malignancy Figure 2.
The patient was placed in supine position on operating table and fixed with three supports: pubic, sacral and thoracic. The external approach centered on the external part of one third middle of the fibula was performed. The skin incision began 3 cm below the fibular head and extended distally to the lateral retromalleolar gutter. The incision of the subcutaneous tissue led to the crural fascia which was incised in front of the lateral sural cutaneous nerve (lateral cutaneous branch of the sural nerve) suppling the skin on the posterior and lateral surfaces of the leg.
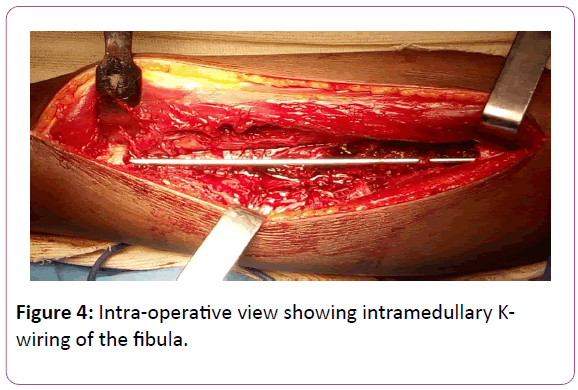
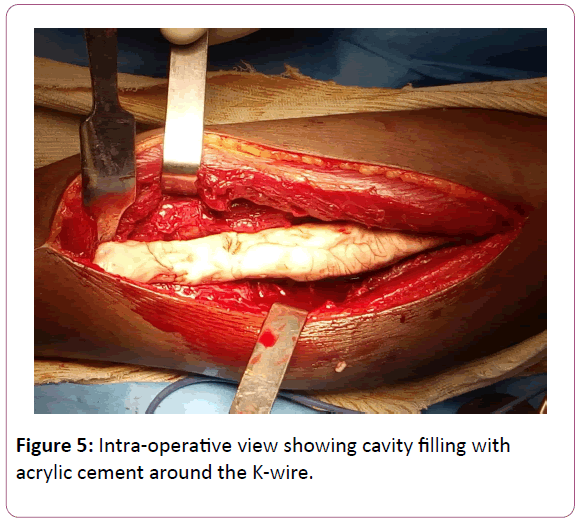
At the lower part of the incision, the attention was paid to the superficial fibular nerve which perforates the crural fascia at the lower third of the leg. The approach of the fibular shaft was between the long fibular muscle in front and the soleus muscle behind. Since the entire circumference of the fibula was needed, the long flexor muscle of the hallux was removed from the posterior part. We remained in contact with the interosseous membrane so as not to injure the posterior vascular-venous trunks. We then proceeded to the section with the tumor free margin of 1 cm on both sides of the tumor. The fibula was thereafter tunneled before being cuffed with the acrylic cement to stimulate the induced membrane.
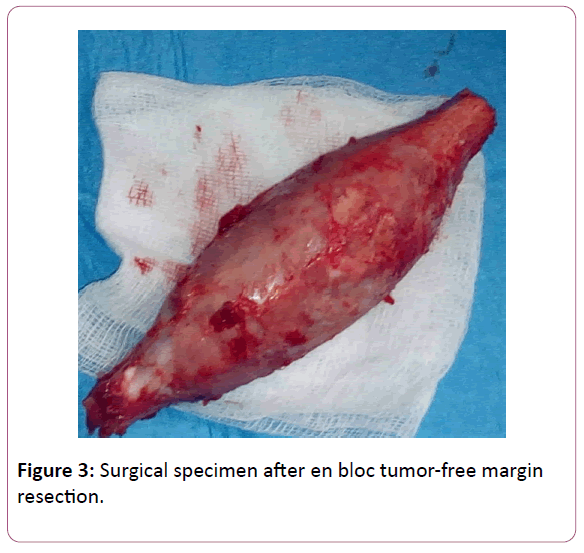
The patient underwent en bloc marginal resection of the tumor and osseous cementation with the acrylic cement as well as fixation with an intra-medullary Krischner wire of the fibula Figures 3 and 4.
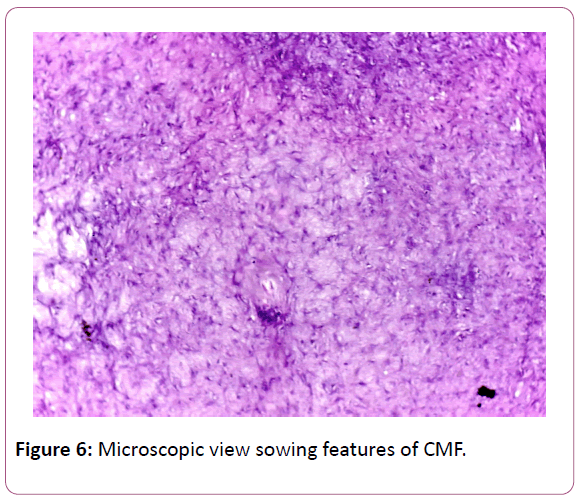
The surgical specimen was sent to the pathology. The report from the anatomopathological examination concluded that this was the chondromyxoid fibroma. No histological signs of malignancy were found Figures 5 and 6.
The patient was reviewed three months postoperatively, and the gait was normal without limping. There were no abnormalities detected at the external one third middle of the leg. The incision was with primary healing. The patient made an eventful recovery of all her daily activities.
Discussion
Chondromyxoid fibroma is the least commonly occurring bone tumor, accounting for approximately 0.5% of all biopsied primary bone tumors and 2% of benign tumors [1]. Jaffe and Lichtenstein first described the condition [2].
As reported in our study and through literature review, the symptomatology had no particularity compared to other benign bone tumors. Clinically, the main symptoms are pain, swelling or tenderness and pressure.
In our case, the age of predilection of this tumor was in the second decade of life [1]. There is a controversial sex predilection. Schajowicz and Gallardo [3] as well as Rahimi et al. [4] and Debra et al. [5] in their respective series found no significative differences between the two sexes. Hence, there is no relationship between sex and CMF.
The most common site of the tumor is the metaphysis of the long bones [6]. However, other bone sites may be involved much as proximal tibia, distal femur, pelvis, and foot [6-8]. The particularity of our case was the fibular shaft location of the tumor without involvement of the proximal and distal epiphyses. It was a form that has never been reported before. The literature reported chondromyxoid fibromas of the fibula located in the metaphyseal region and the epiphyseal line and rarely the articular surface [3,4,6].
Both plain film radiographs and CT scan were initially indicative of an enchondroma. Medical imaging patterns were an expansile ovoid lesion with a radiolucent center, well-defined sclerotic margins, septations, and a bulging, thinned, overlying cortex. However, all these aspects should suggest other tumors such as chondrosarcomas and chondroblastomas as macroscopic features may often lead to the misdiagnosis of chon-drosarcoma.
MRI would demonstrate the exact soft-tissue expansion of this well-structured lesion (vessels, nerves, muscles and the periosteum) especially in case of malignant process as it was reported in the literature. However in our patient; we did not notice neither vascular nor nervous injuries on examination.
Whatever the case may be, histological examination remains the gold standard for diagnosis [9]. It has shown us the classic anatomopathological aspects of CMF.
For the management, as it was a benign lesion without clinical and imaging features of malignant degeneration, and despite the histological diagnosis of CMF has been made; we have opted for en bloc tumor-free margin resection and osseous cementation and intra-medullary K-wiring of the fibula. We wanted to broaden the indications of the Masquelet technique of the induced membrane.
Treatment options for chondromyxoid fibroma in most of the reported cases consist of intralesional curettage alone which however have a high recurrence rate. However; curettage with or without bone grafting and polymethacrylate filling, and en bloc excision is often performed and advocated by many investigators [10]. Hence, the best technique would be one that would allow the en bloc marginal resection of the tumor and the cavity filling with acrylic cement in the short or medium term.
Conclusion
Chondromyxoid fibroma is a benign tumor usually affecting the metaphyseal region of long bones of patients in their second decade of life. Its definitive diagnosis is made by histological examination. The preferred treatment, where possible, is an en bloc excision with tumor-free margins.
References
- Daghfous M, Charfi H, Turki M, Maalla R, Baccari S, et al. (2007) Le fibrome chondromyxoïde. A propos d’une localisation phalangienne du pouce. Chirurgie de la main 26: 159–164.
- Mascard E and Guinebretière JM (2001) Fibrome chondromyxoïde. Encyclopédie médico-chirurgicale (Editions scientifiques et médicales Elsevier SAS, tous droits réservés) appareil locomoteur 14: 732-736.
- Schajowicz F and Gallardo H (1971) Chondromyxoid fibroma (fibromyxoid chondroma) of bone. A clinico-pathological study of thirty-two cases. J Bone Joint Surg Br 53: 198-216.
- Ahimim A, Beabout JW, Ivins JC, Dahlin DC (1972) Chondromyxoid fibroma: A clinicopathologic study of 76 cases. Cancer 30: 726-736.
- Zillmer DA and Dorfman HD (1989) Chondromyxoid Fibroma of Bone: Thirty-Six Cases With Clinicopathologic Correlation. Hum Pathology 20: 952-964.
- Wu CT, Inwarads CY, O’ Laughlin S, Rock MG, Beabout JW, et al. (1998) Chondromyxoid fibroma of bone: a clinicopathologic review of 278 cases. Hum Pathol 29: 438–446.
- Unni K, Inwards C (2010) Chondromyxoid fibroma. In: Dahlin’s bone tumors, Lipincott-Williams and Wilkins, Philadelphia pp. 50–59.
- Lersundi A, Mankin HJ, Mourikis A, Hornicek FJ (2005) Chondromyxoid fibroma: a rarely encountered and puzzling tumor. Clin Orthop Relat Res 439: 171–175.
- Durr HR, Lienemann A, Nerlich A, Stumpenhausen B, Refior HJ (2000) Chondromyxoid fibroma of bone. Arch Orthop Trauma Surg 120: 42-47.
- Hommadi A, Ziadi T, Rachid K, Drissi SM (2009) Fibrome chondromyxoïde de la diaphyse humérale: revue de la littérature. La Lettre du Rhumatologue 357: 30-32.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences