Botulism and its Public Health Implications
Araya Mengistu* and Belachew Worneh
Department of Veterinary Medicine and Animal Sciences, University of Gondar, Gondar, Ethiopia
- *Corresponding Author:
- Araya Mengistu
Department of Veterinary Medicine and Animal Sciences,
University of Gondar,
Gondar,
Ethiopia,
Tel: 2510911752959;
E-mail: armen.kassa@gmail.com
Received date: September 24, 2022, Manuscript No. IPJZDPH-14632; Editor assigned date: Septembre 27, 2022, PreQC No. IPJZDPH-14632 (PQ); Reviewed date: October 12, 2022, QC No. IPJZDPH-14632; Revised date: January 19, 2023, Manuscript No. IPJZDPH-14632 (R); Published date: January 27, 2023, DOI: 10.35841/IPJZDPH.7.1.001
Citation: Mengistu A, Worneh B (2023) Botulism and its Public Health Implications. J Zoonotic Dis Public Health Vol:7 No:1
Abstract
Botulism is a rare but serious neuro paralytic disease of both human and animal caused by absorption of preformed neurotoxin produced by Clostridium botulinum, which is rod-shaped, gram positive, motile, obligate anaerobic and spore forming clostridia specie. Temperature, pH, water activity, redox potential, food preservatives and competing microorganisms limit the growth of Clostridium botulinum in food. Clostridium botulinum is an alimentary bacterium that can produces heat resistant spores that able to poisoning the food. After ingestion with food spores germinate in the intestinal tract and release toxin that could result in botulism. The spores are common in the environment especially in soil, sediments and water. C. botulinum also produces eight different types of poisons neurotoxins having same therapeutic value and inactivated by heating at 85oc for five minutes. The potent botulotoxin binds to nerve endings where it blocks the release of acetylcholine to motor neurons, leading to typical progressive flaccid paralysis. Rapid treatment by antitoxin is essential, unless death is most likely to occur due to respiratory failure. Significant economic loses could occur due to sporadic occurrences as well as outbreaks. In areas where botulism is prevalent, vaccines may be used in animals. Proper boiling and heating of home canned foods before consumption and vaccination will reduce botulism intoxication. Proper disposal of contaminated materials, avoiding eating of expired and bulged canned food items and burning or burying of carcasses should be practiced as preventive measures.
Keywords
Botulism; Clostridium; Human; Toxin; Temperature
Introduction
The genus Clostridium contains several species that are found in many places in the environment, mostly on the soil. The species of clostridia are all characterized by being gram positive, spore-forming and anaerobic producing extracellular toxins [1]. Their size varies between 0.2 μm-4 μm and 2 μm-20 μm and their ability to form spores is crucial to withstand the environment. Botulism is not caused by the bacterium Clostridium botulinum, but rather by the toxins that it produces.
Botulinum toxin is produced only after the spores germinate, when the organism is actively growing and multiplying. C. botulinum also a member of family of lethal pathogens those are all capable of causing rapid, severe sickness and death, because of productions of most potent biotoxins. Tetanus, blackleg and malignant edema are other diseases caused by members of the Clostridium genus [2]. Recently the disease is investigated in Denmark and Romania (By News Desk on March 16, 2021, By News Desk on August 1, 2021), in Ukraine (by NEWS DESK, January 19, 2022), in Ethiopia (BMC Infectious Diseases volume 21, Article number: 1270 (2021) and other parts of the globe.
The nature of the causative agents
Botulism is caused by absorption of Botulinum Neurotoxin (BoNTs) produced by anaerobic, spore-forming, motile bacteria called Clostridium botulinum during vegetative growth. The most common causes of Botulism in animals are type B, C and D, but in humans usually caused by toxin types A, B and E. In rare cases by types F and G are also described [3]. Type G was identified in 1970 but has not been determined as a cause of botulism in humans or animals. The strains of C. botulinum, each distinguished by its production of a serologically distinct botulinum type.
The species Clostridium botulinum and some strains of Clostridium bara ii and Clostridium butyricum are BoNTproducing clostridia, but C. botulinum is mostly responsible for causing botulism [4]. It is classified as a single species, but it is divided into four phenotypic groups (Group I-IV), based on the ability to digest complex proteins. Group I have proteolytic characteristics and produces type A, B and F toxins, but Group II have non-proteolytic characteristics and produces type B, E and F toxins. Group III strains produces type, Cα, Cβ and D. group-IV contains only strains producing BoNT serotype G. C. botulinum strains play a vital role in the natural carbon recycling process, growing in decaying organic matter and producing high levels of BoNTs.
On the basis of their genotypic, phenotypic and biochemical characteristics, these strains are divided into 6 groups: C. botulinum (group’s I-IV), C. butyricum and C. bara ii. Groups I and II, C. butyricum and C. bara ii are mainly associated with human botulism, whereas group III organisms are mainly responsible for animal botulism [5]. Group IV organisms, also known as Clostridium argentinense, are associated with wound botulism. Group I and II organisms are capable of producing type A, B, E and F toxins; group III organisms can produce type C, D and their mosaic C/D and D/C toxins. Group IV, C. butyricum and C. baratii produce type G, E and F toxins, respectively.
C. botulinum is motile by peritrichous flagella which are arranged singly, in pairs or in small chains. It is also rod shaped with round extremities and is about 0.8 μm-1 μm wide and 4 μm-6 μm long. C. botulinum develops into ovoid spore that is highly resistant in the environment. It requires an oxygen free environment for its growth because of it is an obligate anaerobic bacterium and optimum temperature ranges between 16°C-40°C (approximately 25°C) with some exceptions between strains [6]. The optimum for toxin production ranges from 25°C-42°C and the bacteria prefer slightly alkaline environment (PH 7-7.6). Type D strains can produce toxin in carrion at a temperature as low as 9°C, whereas a type C strain failed almost completely to do it at 16°C.
C. botulinum spores can survive for almost 30 years and germinate under warm and humid conditions. The ability of C. botulinum to cause food poisoning in humans is directly related to the production of resistant spores that survive preservation methods that kill non-sporulating organisms. The heat resistance of spores varies from type to type and even from strain to strain within each type, although some strains will not survive at 80°C, spores of many strains require temperatures above boiling to ensure destruction [7]. The thermal resistance of spores also increases with higher pH and lower salt content of the medium in which the spores are suspended.
Spores can have resistance to alcohol, quaternary ammonium, phenol compounds and ultraviolet rays. But the vegetative form has low resistance to the environment. Spores are not resistant to gamma radiation, formaldehyde, ethylene, propylene and heat. Spores are found more heat resistant at low water activity and natural pH values and more sensitive at low pH values. Proteolytic spores are inactivated at 121°C for 3 minutes and non-proteolytic spores inactivated by 90°C after 10 minutes [8].
Disease occurrence
Botulism has no geographical limitations, sporadic outbreaks occurring in most countries [9]. The source of exposure to toxin and the risk for disease differ between regions because of differences in food storage, feeding and management practices. Outbreaks associated with ingestion of toxin in conserved feeds are more common in the northern states of the USA and Europe, whereas outbreaks in animals on pasture are reported primarily from South Africa, Australia and the Gulf coast area of the USA. The disease usually occurs in a number of animals at one time and has a high case fatality rate.
C. botulinum pathogens occur worldwide and are associated with soil, decaying and rotting vegetative material or cadavers. The distribution of the organism is not homogeneous, as a result of environmental factor influences. For example, the disease in southern African cattle is common because of phosphorus-poor soils. The main habitat of these clostridia is the soil but they are also found in sewage, rivers, lakes, sea water, fresh meat and fish.
The incidence rate of botulism in the US is low due to increasing education and awareness of proper storage and handling of foods. There were 121 reported cases of botulism in 2009, of which 11 were food borne, 84 infant, 23 wound and 3 of unknown or other etiology. In 2011, a total of 140 confirmed cases of botulism were reported to the CDC. Of these, 20 were food borne, 102 infant, 13 wound and 5 of unknown or other etiology. While fewer cases of food borne illness are caused by C. botulinum per year than by Salmonella, the death rate from botulism is relatively high, 17.3%, compared to 0.5 percent for Salmonella.
Since the recognition of infant botulism in 1976, cases have been identified with increasing frequency. In the United States, 1442 cases were reported to CDC from 46 states between 1976 and 1996 [10]. Type A accounted for 46.5% of these cases and type B for 51.9%. Since reporting began to stabilize in 1980, the average annual incidence of reported infant botulism in the United States has been approximately 1.9/100,000 live births. Since 1976, 47.2% of all infant botulism cases have been reported from California. Between 1976 and 1994, the incidence of infant botulism was highest in Delaware, Hawaii, Utah and California (9.0, 8.8, 6.3 and 5.7 per 100,000 live births, respectively). Affected infants are also more commonly breast-fed and breast-feeding is associated with an older age at onset in type B cases.
Literature Review
The type of toxins produced by the agents
C. botulinum produces eight different types of neurotoxins; A, B, Cα, Cβ, D, E, F and G. Botulinum neurotoxins are the most poisonous poison and colorless, odorless and presumably tasteless. The toxins are inactivated by heating higher than 85°C for five minutes.
The botulinum toxins consist of two polypeptide chains, a heavy chain and a light chain linked by disulphide bond [11]. The light chain includes zinc peptidase activity. The heavy chain has a translocation domain being responsible for the formation of a spore through which the light chains passes and a binding domain for binding to nerve cells. Although the toxin types have very similar physical and chemical properties, they differ greatly in toxicity for different animal species. All eight types of Botulinum Neurotoxins (BoNT) are zinc endopeptidases with same hydrolytic activity on docking proteins required by neurotransmitter containing vesicles to fuse with the presynaptic membrane. Blockage of the release of neurotransmitters (acetylcholine) due to hydrolysis and this is the same result for all the toxin types. What distinguishes the toxin types is that they hydrolyze different docking proteins. That means C. botulinum type A and E hydrolyze SNAP-25 (synaptosomal-associated protein 25). Toxin types B, D, F and G hydrolyze VAMP (Vesicle Associated Membrane Protein, also known as synaptobrevin). Type C hydrolyzes SNAP-25 and a protein on the target membrane, syntaxin. A hydrolyzed synapse requires weeks to months to regenerate.
Distribution of the agents and toxins
C. botulinum is found worldwide, however, its distribution is not homogeneous and cases tend to be more common in certain geographic areas. Environmental factors can also influence where botulism is seen; for instance cattle from phosphorus poor soils like southern Africa are more prone for the disease. The distribution of strains can also vary with the geographic area. In one study from the U.S., strains that produce type A toxin were detected mainly in neutral or alkaline soils in the western states, while type D producing strains were found in some alkaline soils in these states while the distribution of type B strains was more uniform, although, especially common in the eastern states and type C strains were detected in acidic soils in the Gulf Coast states. In North America, type E strains are most common along the shores of the great lakes and in the pacific Northwest. In a study from the former U.S.S.R., type E toxin producing once was accounted for 61% of the isolations [12]. Knowing the toxin types that are prevalent in an area may be helpful in selecting an antitoxin, as this must often be done before the laboratory results are complete.
Source of intoxication or toxicoinfections
Spores are found in soil worldwide, marine sediments, some agricultural products (e.g., honey), the intestinal tracts of some animals including fish, and household dust. Botulinum toxin retains much of its activity in untreated water and beverages for up to 70 days; water treatment processes inactivate the toxin [13]. Growth of C. botulinum and production of toxin is favored in canned food products with low-acid, low-salt, low-sugar and low oxygen content. Homecanned vegetables fruit and fish products are now the most common sources of botulism. Modern industrial canning was developed expressly for killing C. botulinum spores.
Most incidents of botulism are associated with the ingestion of preformed toxin (forage botulism). Toxin in feeds may result from the primary growth of C. botulinum in the feed or from the contamination of the feed with toxin containing carrion (carrionassociated botulism). Less common sources are growth with toxin production in wounds (wound botulism) or growth and toxin production in the alimentary tract (toxic infectious botulism).
Infant botulism occurs when an infant ingests spores of C. botulinum which in turn colonize the intestinal tract and produce toxin [14]. In a prototypical case, type B organisms, but no toxin, were isolated from honey fed to an infant with infant botulism whose fecal specimens contained type B organisms and toxin. Family members who eat some of the same honey did not become ill.
Spores of C. botulinum are common in marsh soil and can persist there and animals living in marsh areas ingest spores frequently. Decaying animal material provides a suitable substrate for C. botulinum growth, vertebrate carcasses being of particular importance. When an animal containing C. botulinum spores dies, putrefaction, invasion of tissues by C. botulinum from the gut and associated toxin production occurs.
The larvae of sarcophagus fly Sarcophagi species, feeding on the carcasses, are not affected by the toxins but concentrate the toxin. Ingestion of a single toxigenic maggot could be lethal and their carcasses become substrates for the generation of further toxins and more maggots, thus perpetuating the cycle [15]. Despite its microbiology being well understood, management of the disease still primarily consists of carcass collection during epizootics rather than any form of preventative management.
Transmission
Botulism usually occurs when people or animals ingest the toxins in food or water or when the spores germinate in anaerobic tissues and produce toxins as they grow. Botulinum toxin does not pass through intact skin, but it can cross mucous membranes and broken skin [16]. Laboratory accidents can cause botulism by inhalation of the aerosolized toxin or other means and bioterrorism is a possibility. Animal, as well as human botulism, the primary contamination route is the ingestion (absorption) of preformed toxins in foods or feeds. Raw material, such as grass, hay, rotting vegetation, and slaughterhouse waste, as well as decay of vertebrate carcasses, invertebrates and sewage may support BoNT producing clostridia growth and toxin production.
Animals may directly ingest decaying organic matter containing toxin or they may ingest toxins through the consumption of zooplankton or invertebrates, such as larvae, that have consumed toxic material [17]. Typically, type C and D toxins are associated with carrion of birds or small animals that have contaminated water, feed or the environment, while noncarrion associated botulism is caused by type A and B toxins.
A second form of animal botulism is associated with the absorption of BoNTs produced in vivo in the intestinal tract. This form of botulism, seen in chickens and horses, can be categorized as a toxicoinfection. Bohnel and colleagues describe a toxicoinfection in cattle, referred to as ‘visceral botulismÌ? . This form of animal botulism is hypothesized to occur when C. botulinum colonizes the lower section of the intestine. BoNT is formed and partially absorbed by mucous membrane, and the rest is excreted with the feces. Excretion of feces containing BoNTs by animals that do not show any clinical symptoms of acute paralysis may demonstrate the production of toxins in the lower sections of intestines where only a low amount is absorbed, in contrast to the proximal parts of the intestinal tract in which toxins are highly absorbed [18]. A third form of animal botulism is caused by the germination and production of BoNTs by C. botulinum spores in infected wounds. The last two forms are often referred to as toxicoinfectious form botulism.
The four transmission categories of human botulism are: food borne, infant, wound and other. Food borne botulism results from the ingestion of preformed botulinum toxin in food. The toxin can be found in food that has not been properly cooked, processed, handled or canned and is often present in canned food such as vegetables, meat and seafood products. Infant botulism occurs when infants (persons less than one year of age) ingest C. botulinum spores that then germinate and produce the botulinum toxin in the intestines. Honey is a common dietary source of C. botulinum spores; infants should never be fed honey.
Wound botulism results when C. botulinum infects a wound and produces the toxin, which is then carried throughout the rest of the body via the bloodstream. Adult intestinal toxemia/colonization (which occurs in the same way as infant botulism), and iatrogenic botulism (an accidental overdose of the toxin injection) are also included in the classification, but no secondary person to person transmission has been recorded.
Pathogensis, pathogenicity and resistance
BoNT is the etiological agent of human and animal botulism. As extensively reported elsewhere, the BoNT mechanism of action consists of the following steps: Binding of heavy chain to polysialoganglioside and probably other protein receptors on the neuronal membrane, internalization of active toxin into endosomal like compartments, membrane translocation facilitated by HN (Heavy chain N-terminal) and enzymatic cleavage of target proteins by the light chain.
In intoxication the toxin will withstand the acid environment of the stomach. As it enters the small intestine, digestive enzymes (e.g. trypsin) or bacterial protease will react on the toxin transforming it into active form. The active toxin is absorbed in the small intestine by binding to the receptors on the apical surface of gut epithelial cells. It is then released into the general circulation (blood stream) and reaching all peripheral cholinergic nerve endings (synapses), which include the neuromuscular junction and autonomic synapses. All botulinum toxin types contain 150 kd polypeptide chains; a100-kd heavy chain joined to a 50 kd light chain by a disulphide bond.
The light chain is globular protein with zinc endopeptidase activity in which it cleaves neuronal SNARE (soluble Nethylmaleimide- sensitive fusion protein attachment protein receptor) protein involved in synaptic transmission. The heavy chain has two domains; the N-terminal translocation domain and the C-terminal receptor binding domain. N-terminal consists of α-helices that facilitate the passage of the light chain into the cytosol of the nerve cell. C-terminal is important for the association of the toxin with the target cell. Variation in the receptor binding affinity may describe the differences in susceptibility to C. botulinum toxins.
After binding to nerve cell receptors the toxin light chain is internalized through receptor mediated endocytosis. Once inside the nerve terminal the light chain hydrolyzes the SNARE proteins. The SNARE proteins constitute the core of the vesicular fusion machinery enabling fusion of neurotransmitter vesicles with the neuronal plasma membrane and permits release of acetylcholine into the synaptic cleft. This causes depolarization of the muscle membrane and muscle contraction in normal physiological conditions. Cleavage of these proteins under pathological conditions prevents membrane fusion and release of acetylcholine from the nerve cell. In these sites, the toxin binds to specific receptors and is internalized into the cytosol of the nerve terminus, where it blocks the release of acetylcholine, producing the characteristic acute flaccid paralysis and the nerve impulse stops [19]. When this affects respiratory muscle death due to respiratory failure occurs.
C. botulinum is an alimentary bacterium where botulism can be caused by ingestion of preformed toxin. The toxins are the most potent accordingly one milligram contains 4800000 MLD (minimal lethal doses) for guinea pigs. The MLD (Minimal Lethal Doses) of type a toxin in mice is 1.2 ng per 1 gram of body weight intraperitoneal inoculation. The lethal dose for a person by the oral route is estimated at 30 ng, by the inhalational route 0.80 to 0.90 μg, and by the intravenous route 0.09 μg to 0.15 μg. Assuming an average weight of 70 kg each of 5.6 billion people, only 39.2 g of pure BoNT would be sufficient to eradicate humankind.
Resistance to botulism depends on circulating antitoxins. Some animals such as turkey, vultures; apparently acquire immunity through repeated sub lethal exposure. In botulism outbreaks, toxin is released in the tissue of the organism. Animals are protected against the disease if antitoxins produced by their immune system after initial exposure to the specific toxin type. It is necessary to select antitoxins of the serotypes that are present in the particular region for successful treatment or vaccination.
Clinical and pathological manifestations
Clinical signs in humans: The botulinum toxin produced by C. botulinum is a neurotoxin that causes descending, flaccid paralysis of the muscles, including respiratory system which leads to Respiratory failure. Four distinct naturally occurring forms of human botulism have been recognized and all forms are associated with an acute, a febrile, symmetric, descending flaccid paralysis. The symptoms of botulism are varying with the type of toxin produced rather than the site of its production.
The clinical syndrome of botulism, whether food-borne, infant, wound or intestinal colonization, is dominated by the neurologic symptoms and signs resulting from a toxin induced blockade of the voluntary motor and autonomic cholinergic junctions and is quite similar for each cause and toxin type. Incubation periods for food borne botulism are 6 hours to 10 days, but generally the time between toxin ingestion and onset of symptoms ranges from 18 to 36 hours. Typical clinical symptoms of all forms of botulism are a result of muscle paralysis from affected cranial nerves. These symptoms include double and blurred vision, slurred speech, difficulty swallowing and facial paralysis, dry mouth, diarrhea, nausea and muscle weakness that descends through the body. Recovery occurs with prompt administration of an antitoxin that blocks the action of the botulinum toxin in the body. In cases of severe botulism, patients may require respiratory intensive care for weeks or months until the paralysis alleviates.
Infants are not able to complain about the early effects of botulinum intoxication, the neurologic dysfunction associated with infant botulism often seems to develop suddenly. The major manifestations are poor feeding, diminished suckling and crying ability, neck and peripheral weakness (the infants are often admitted as "floppy babies"), and ventilatory failure. Constipation is also often seen in infants with botulism, before the onset of neurologic abnormalities. Loss of facial expression, extra ocular muscle paralysis, dilated pupils, and depression of deep tendon reflexes are more frequent with type B than with type A infant botulism.
Summary of types of botulism
As a general summary: There are five clinical categories of botulism: Foodborne botulism; wound botulism; infant botulism; adult infectious botulism; inadvertent, following botulinum toxin injection.
Food borne botulism: Onset generally occurs 18 to 36 hours after exposure (range, 6 hours to 8 days). Initial s ymptoms can include nausea, vomiting, abdominal cramps or diarrhea. After the onset of neurologic symptoms, constipation is typical. Dry mouth, blurred vision and diplopia are usually the earliest neurologic symptoms. They are followed by dysphonia, dysarthria, dysphagia and peripheral muscle weakness. Symmetric descending paralysis is characteristic of botulism.
Wound botulism: This can be defined as clinical evidence of botulism following lesions, with a resultant infected wound and no history suggestive of foodborne illness. Except for the gastrointestinal symptoms, the clinical manifestations are similar to those seen in foodborne botulism. However, the incubation period is much longer as time is required for the incubation of spores, growth of Clostridium and release of toxins (4 to 14 days).
Infant botulism: This is caused by the absorption of toxin produced by Clostridium botulinum that colonize the intestinal tracts of infants under one year of age. It is often associated with ingestion of honey and the first clinical sign is usually constipation. After a few weeks, progressive weakness and poor feeding are observed. The weakness is symmetrical and descending. It evolves over hours or several days. The infant is afebrile and has a weak cry, has either absent or diminished spontaneous movements, decreased sucking, floppy head and decreased motor response to stimuli. The autonomic nervous system manifestations include dry mucous membranes, urinary retention, diminished gastro-intestinal motility, fluctuation of heart rate and changes in skin colour. Duration of hospitalisation may last from a few days to six months.
Adult infectious botulism: It occurs as a result of intestinal colonization with C. botulinum and in vivo toxin production in a manner similar to that of infant botulism. These patients often have a history of abdominal surgery, achlorhydria, Crohn’s disease or recent antibiotic treatment. The disease may simulate a GuillainBarre syndrome.
Inadvertent botulism: This has been reported in patients who have been treated with intramuscular injections of botulinum toxin. Marked clinical weakness is observed as well as electrophysiologic abnormalities.
Discussion
Diagnosis and differential diagnosis
Clinical signs of animal are often strongly indicative of botulism, but lacks specificity. A presumptive diagnosis is done based on a combination of clinical signs in sick animals, history, postmortem findings and by ruling out other differential diagnoses.
In horses, weakness, decreased eyelid tone, decreased or absent tongue tone, decreased tail and anal tone, sluggish pupillary light reflex and occasional episodes of slow and uncoordinated padding used for diagnosis. Horses that feed in a group, the dominant horse eats first and is therefore usually the first one to develop clinical signs and shows most rapid progression of the neurotoxic syndrome. In cattle, clinical signs (flaccid paralysis), epidemiology of the outbreak, clinical chemistry and neutrophilia support the diagnosis.
For the mouse protection test, blood is collected from a sick or freshly dead animal and the serum fraction is inoculated into two groups of laboratory mice, one group of which has been given type-specific antitoxin. The mice receiving antitoxin will survive and those that receive no antitoxin will become sick with characteristic signs or die, if botulism toxin is present in the serum sample. The ELISA is an in vitro test that detects inactive as well as biologically active toxin. During outbreaks it is common to find healthy, sick and dead animals in the same area.
Botulism is probably substantially under diagnosed but diagnosis is not difficult when it is strongly suspected, as in the setting of a large outbreak, but since cases of botulism most often occur singularly, the diagnosis may pose a more perplexing problem. They may be diagnosed only retrospectively after death, when the subsequent clustering of cases of botulism like illness finally alerts public health personnel to an outbreak of botulism after misdiagnosis. Other cases are undoubtedly missed entirely. Entire outbreaks may even go undetected despite severe illness in patients.
Food borne botulism: Diagnosis is made by detecting botulism toxin in serum, stool or implicated food or by culturing C. botulinum from stool. Vomits or gastric aspirate can be tested for toxin if obtained within a few hours of food ingestion. Often the symptoms of food borne botulism are mistaken for symptoms associated with stroke, chemical intoxication, myasthenia gravis or Guillain-Barre syndrome. Tests such as brain scans, spinal tap exams, nerve conduction exams, Electromyography (EMG) and a tensilon exam can distinguish the above diseases from botulism.
Wound botulism: Diagnosis is made by detecting botulism toxin in serum or by culturing C. botulinum from an infected wound. Stool should be obtained in addition to rule out food borne botulism if patient history is unavailable or implicates risk foods. Infant botulism: Diagnosis is made by detecting botulism toxin in stool or by culturing C. botulinum from stool. In contrast to food borne and wound botulism, in cases of infant botulism, the toxin is rarely detected in serum and collection of serum is not recommended.
Based on clinical pathology: There are no changes in hematological values or serum biochemistry that are specific to botulism. Hypophosphatemia may be present and Muscle enzyme activities may also moderately elevate. In foals, arterial blood analysis shows acidemia, hypercapnia, hypoxemia and desaturation of hemoglobin.
Laboratory diagnosis of botulism in the live or dead animal is difficult because of the lack of sensitive confirmatory laboratory tests. Demonstration of BoNTs or spores in serum, feed material or intestinal content by the mouse bioassay and Detection of antibody in recovering or clinically normal at risk animals are important laboratory confirmation of botulism.
Based on necropsy findings; no specific changes detectable at necropsy, although the presence of suspicious feedstuffs in the fore stomachs or stomach may be suggestive. There may be nonspecific subendocardial and subepicardial hemorrhages and congestion of the intestines. Per vascular hemorrhages in the corpus striatum, cerebellum and cerebrum are nonspecific microscopic changes in the brain. The presence of toxin in the gut contents is confirmatory if found but is often absent, because the toxin may have already been absorbed. The presence of the toxin in the liver at postmortem examination is taken as evidence that the disease has occurred. In addition to mouse protection test, ELISA techniques and immuno- Polymerase Chain Reaction (PCR) assay are used for toxin detection.
Differential diagnosis
Differential diagnosis in cattle includes parturient paresis (hypocalcaemia), hypomagnesaemia, carbohydrate overload and toxicosis, including from mycotoxin, lead, nitrate, organophosphate, atropine or atropine like alkaloid, tick paralysis, tetanus and paralytic rabies. In horses, toxic plant poisoning, organophosphate intoxication, equine viral encephalitis, central nervous system trauma, equine protozoal myeloencephalitis, aberrant larval migration, tetanus, rabies and hyperammonemia. Avian botulism most often affects waterfowl in the season when they are flightless because of wing molt.
Differential diagnosis of humans
The differential diagnosis in human includes myasthenia gravis, stroke, Guillain-Barre syndrome, bacterial and chemical food poisoning, tick paralysis, chemical intoxication (e.g., from carbon monoxide, barium carbonate, methyl chloride, methyl alcohol, organic phosphorus compound or atropine), mushroom poisoning, medication reactions (e.g., from antibiotics such as neomycin, streptomycin, kanamycin or gentamicin), poliomyelitis, diphtheria and psychiatric illness. In infant botulism, sepsis (especially meningitis), electrolyte mineral imbalance, metabolic encephalopathy, Reye syndrome, congenital myopathy and Leigh disease should also be considered. Routine laboratory studies are not helpful in confirming the clinical suspicion of botulism. Serum electrolytes, renal and liver function tests, complete blood tests, urinalysis and electrocardiograms will all be normal unless secondary complications occur. A normal Cerebrospinal Fluid (CSF) examination helps differentiate botulism from Guillain- Barre syndrome, although a slightly elevated CSF protein level is occasionally seen with botulism and the protein level might be initially normal in Guillain-Barré syndrome.
Zoonotic implications
Botulism cannot be directly transmitted from diseased animal to humans who handle them. But the potential sources of contamination are faces, tissues and body fluids from animals with botulism. The meat and the milk from cattle that have botulism should not be used for human consumption.
Botulism in humans is usually the result of eating improperly home canned foods and is most often caused by type A or type B botulinum toxin. There have been several human cases of type E botulism in North America from eating improperly smoked or cooked fish or marine products. Type C botulism has not been associated with disease in humans, although several outbreaks have been reported in captive primates. Through cooking destroys botulinum toxin in food. Foodborne botulism cannot be spread from person to person. Although it is one of the least common of the foodborne diseases, anyone is susceptible to C. botulinum illness (as foodborne intoxication) even with the ingestion of only a small amount of toxin present in contaminated food. Immunocompromised individuals, young children and elderly individuals may suffer from more serious symptoms. As an impact, a report from US could be takes as granted in that an average of 110 cases of botulism is reported annually in the country, of which approximately seventy percent of these cases are infant botulism and about 25% of these cases are food borne botulism. The mean age of infected people is 46 years, with a range from 3 to 78 years and it is revealed that men and women are affected equally.
Botulism in infants
• Mean age of disease onset is 13 weeks, with a range from 1 to 63 weeks.
• Boys and girls are affected equally.
Infant botulism
• Was first recognized in 1976. Since 1980, infant botulism has been the most commonly reported form of botulism in the US.
• Is a sporadic disease. While it is a serious illness for the affected child, it does not pose a public health threat because it is extremely rare and has no epidemic potential.
• Those hospitalized with the disease tend to have higher birth weights and are more often born to mothers who are Caucasian, older and have higher education levels.
• Affected infants are more commonly breast-fed and have histories of normal gestation and delivery with no congenital abnormalities.
Treatment, prognosis, prevention and control
Botulism is life threatening condition, administration of antitoxin is the only specific therapy and it is effective only if given very early in the course of neurologic dysfunction. When botulism is suspected, the first critical therapeutic step is to give polyvalent antitoxin to affected animals. Antitoxin treatment should be initiated as soon as possible, because it is effective only against circulating toxin and not when toxin is fixed at the neuromuscular junction. Antibiotic administration is indicated only when there is a suspicion of inhalation pneumonia or wound infection. Clostridiocidal drugs may lyses vegetative cells of BoNT producing clostridia, thereby increasing the amount of free toxin in the intestinal tract. Aminoglycosides may potentiate neuromuscular weakness and a non-depolarizing type of neuromuscular block. Although antibiotic treatment is discouraged, beta-lactams have been successfully used to treat poultry affected by the toxicoinfection form of botulism. Other therapies include supportive care (oral water and electrolytes) and reduced physical activity.
For cattle, vaccination can be considered to be effective as a therapeutic treatment in an outbreak situation. Waterfowl can recover from botulism by being administered antitoxins or being provided fresh water and shade. Treated birds should be maintained in pens that provide free access to fresh water, shade, the opportunity for recovered birds to fly out and minimal disturbance. Once the diagnosis has been made, euthanasia is frequently advised to avoid problems in maintaining the animals’ welfare. Prognosis in recumbent animals is poor. Antitoxin treatment improves the prognosis, but the results are variable. Prevention is preferred for animals in risk.
The main steps of treatment of food borne and wound botulism are administration of botulinum antitoxin in an attempt to prevent neurologic progression of a moderate, slowly progressive illness or to shorten the duration of ventilatory failure in those with a severe, rapidly progressive illness; careful monitoring of respiratory vital capacity and aggressive respiratory care for those with ventilatory insufficiency (monitoring of respiratory vital capacity should be performed as soon as diagnosis of botulism is made) and meticulous and intensive care for the duration of the often prolonged paralytic illness. Food borne botulism or intestinal/colonization botulism; intravenous administration of trivalent (ABE) botulinum antitoxin as soon as possible is routine treatment. Wound botulism; penicillin or metronidazole should be given to patients with wound botulism following antitoxin administration. The wound should be debrided even if it appears to be healing well.
Infant botulism; human derived antitoxin is indicated for the treatment of infant botulism caused by type A or type B toxin. Equine-derived antitoxin is generally not recommended for infant botulism, because of the potential risk of anaphylaxis, serum sickness or the sensitization (lifelong hypersensitivity) of the infant to horse antigen. Equine antitoxin neutralizes only toxin molecules yet unbound to nerve endings.
Prevention and control
The growth of C. botulinum and toxin production depends on appropriate conditions in food including: temperature, oxygen level, water activity, pH, the presence of preservatives and competing micro flora.
Commercial canned foods are heated to a sufficient temperature and for a sufficient time to kill the spores. Unheated commercial foods in cans or jars can be made safe by acidification or other manipulations that inhibit the growth of the organism (e.g., addition of phosphoric acid to garlic in oil). Persons doing home canning and other food preservation should be advanced about the proper time, pressure and temperature required to destroying spores, the need for adequately refrigerated storage of incompletely processed foods and the effectiveness of boiling, with stirring, home canned vegetables to destroy botulinum toxins. Heating home canned foods before consumption can reduce the risk of botulism intoxication. C. botulinum may cause container lids to bulge and the contents to have “offodors.” Commercial cans or home canned products with bulging lids should not be opened and foods with off-odors should not be eaten or “taste tested.” Honey should not be fed to infants because it has been identified as a food source.
In animal the counter measures to prevent or minimize feed borne botulism are based on: providing safe and high quality feed to farm animals, properly storing animal feed, inspecting water sources for dying or dead small animals and birds, avoiding spreading poultry litter that contains birds or dead animals on pastures, avoiding using poultry litter as bedding material and vaccinating animals.
Preventing botulism can be efficiently achieved by vaccination, which generates neutralizing antibodies against BoNTs. In areas where botulism is endemic, vaccine may be used in animal including cattle, horses, sheep, goats, birds and mink. There is no cross protection against between toxin types and if an animal survives disease it is not protected from later exposure to that toxin.
In human, only high risk groups such as laboratory workers who work with botulism specimens or military personnel in risk of botulism are vaccinated when they used it as biological weapons. Botulism can be prevented if careful measures are used in canning and processing foods. Strict hygienic procedures should be followed when canning foods home. Other items such as oils with garlic or herbs have been known to contain traces of spores so keep these refrigerated. Cooking food thoroughly is highly suggested. The neurotoxin can be destroyed at 85°C after 5 minutes, so boiling of canned products for at least 10 minutes is highly recommended. Bulging cans and other abnormal smelling foods should not be tasted, but rather thrown away immediately. Honey should not be fed to babies less than 1 year of age. Wound botulism can be prevented by treating the wound immediately and avoiding injectable street drugs.
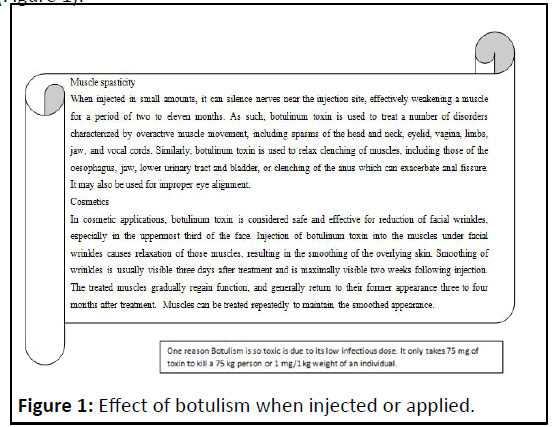
Therapeutic importance of the toxins and biological war weapon option
One of the most fascinating aspects on C. botulinum in recent years has been development of the most potent toxin into a molecule of significant therapeutic utility. Several pharmaceutical preparations of botulinum toxins for the treatment of human diseases in ophthalmology, neurology and dermatology are marketed with the trade names Botox®, Dysport® and Xeomin® (based on botulinum neurotoxin A) and Myoblock®/ Neuroblock® (based on botulinum neurotoxin B). Except Xeomin®, which is practically devoid of complexing proteins the other commercial formulations of botulinum toxins include, besides the neurotoxin, other bacterial complexing haemagglutinin and non-haemagglutinin proteins as well. Several additional substances such as albumin, sucrose, lactose are included in these preparations for drug stabilization and facilitation of administration by intramuscular injection. Botox® is Avery known cosmetic product to eliminating wrinkles and smooth out the skin. The most side effects include temporary posies, headache, flu, nausea and facial pain swelling.
The US FDA has approved use of these preparations in cervical dystopia, blepharospasm, spasmodic, torticollis and strabismus glabellas frown lines. In recent years type A botulinum toxin has been used in the treatment of spasmodic torticollis. This muscle disorder is characterized by the neck muscles contracting involuntarily causing abnormal posture of the head and neck. Controlled amounts of the toxin are injected directly in to two or more neck muscles. Due to the blockage of transmission of acetylcholine, the muscles relax. After repeated treatments, the muscle tension will eventually return to its normal level. Botulinum toxin is concluded to be the most effective available therapy for spasmodic torticollis.
Botulinum toxin is a category A biological agent and it has been extensively weaponized by governmental military programs and was deployed by a terrorist group. So, BoNTs and BoNT-producing clostridia create an additional concern because of their potential use as biological weapons and bioterrorism. Due to their absolute neurospecificity these neurotoxins do not react with any substrates in the pre-synaptic motor neurons and extremely toxic. The two most likely mechanisms for use of botulinum toxin as a terrorist weapon include deliberate contamination of food or beverages or via an aerosol release (Figure 1).
Conclusions
Generally botulism is a serious neuroparalytic disease of both humans and animals resulting from the action of potent BONTs. It is serious and economically very important due to its mass mortality during outbreaks of the disease. Rapid recognition of the clinical signs and rapid removal of the potential source of botulism toxin or C. botulinum spores is the corner stone to prevent farther spreads of the botulism and enable early administration of specific antitoxin. Without rapid treatment, death is occurring. Strict husbandry and sanitary methods as well as good feeding practices are the crucial way to prevent and control botulism in animal populations. Botulism is always transmitted by ingestion of preformed toxins. It cannot be transmitted directly from diseased animals to humans, but faces, tissues and body fluids from animals infected with botulism are the potential sources of contamination. Outbreaks of botulism in humans have been associated with contaminated canned commercial foods. Failure in one step during food processing can be disastrous, as the potentially toxic products may rapidly distribute globally. Botulism can be caused from unsuccessful heating, failure of packing or storage at temperatures allowing spore germination and neurotoxin (BONTS) production. Outbreaks of botulism are also typically the result of preparation of traditional fermented foods that are eaten without heating. Educate the population about the risk factors of botulism will contribute to efforts to strengthen the prevention and control methods.
Based on the above conclusion the following recommendations are forwarded:
• Avoid consumption of canned foods when the container is bulged, expired and damaged.
• If consuming home-canned foods of low acidity, heat to at least 80°C (176°F) for 10 minutes. Canned corn, spinach and meats should be heated for 20 minutes.
• Properly dispose contaminated material or burn or bury all carcasses, bones or rotting material and prevent stock access to animal carcasses.
• In dry months give the animals a supplement containing phosphate and calcium.
• Take care during harvesting and storage of feeds and check water sources for organic matter contamination.
• Avoid deliberate contamination of beverages or an aerosol release as a weapon.
References
- Bartram U, Singer D (2004) Infant botulism and sudden infant death syndrome. Klinische Padiatrie 216:26-30
[Crossref] [Googlescholar] [Indexed]
- Bohnel H, Schwagerick B, Gessler F (2001) Visceral botulism-a new form of bovine Clostridium botulinum toxication. J Vet Med A Physiol Pathol Clin Med 48: 373-383
[Crossref] [Googlescholar] [Indexed]
- Braun U, Feige K, Schweizer G, Pospischil A (2005) Clinical findings and treatment of 30 cattle with botulism. Vet Rec 156:438-441
[Crossref] [Googlescholar] [Indexed]
- Critchley EM (1991) A comparison of human and animal botulism: A review. J Soc Med 84:295-298
[Crossref] [Googlescholar] [Indexed]
- Lindstro M, Myllykoski J, Sivela S, Korkeala H (2010) Clostridium botulinum in cattle and dairy products. Crit Rev Food Sci Nutr 50:281-304
[Crossref] [Googlescholar] [Indexed]
- Demedici D, Anniballi F, Wyatt GM (2009) Multiplex PCR for detection of botulinum neurotoxin-producing clostridia in clinical, food and environmental samples. App Environ Microbiol 75:6457-6461
[Crossref] [Googlescholar] [Indexed]
- Dressler D, Benecke R (2007) Pharmacology of therapeutic botulinum toxin preparations. Disabil Rehabil 29:1761-768
[Crossref] [Googlescholar] [Indexed]
- Galey FD, Terra R, Walker R, Adaska J, Etchebarne MA, et al. (2000) Type C botulism in dairy cattle from feed contaminated with a dead cat. J Vet Diagn Invest 12: 204-209
[Crossref] [Googlescholar] [Indexed]
- Haagsma J (1991) Pathogenic anaerobic bacteria and the environment. Rev Sci Tech 10:749-764
[Crossref] [Googlescholar] [Indexed]
- Hogg R, Livesey C, Payne J (2008) Diagnosis and implications of botulism. In Practice 30:392-397
[Crossref] [Googlescholar] [Indexed]
- Jean D, Fecteau G, Scott D, Higgins R, Quessy S (1995) Clostridium botulinum type C intoxication in feedlot steers being fed ensiled poultry litter. Can Vet J 36:626-628
[Googlescholar] [Indexed]
- Johnson AL, Sweeney RW, McAdams SC, Whitlock RH (2012) Quantitative real-time PCR for detection of neurotoxin gene of Clostridium botulinum type B in equine and bovine samples. Vet J 194:118-120
[Crossref] [Googlescholar] [Indexed]
- Liguori V, De Luliis P, Fenicia F, Anniballi F, Aureli P (2008) A case of wound botulism in a foal affected by gastric ulcers in Italy. J Equine Vet Sci 28:476-478
[Crossref] [Googlescholar] [Indexed]
- Lindstro M, Nevas M, Kurki J (2004) Type C botulism due to toxic feed affecting 52,000 farmed foxes and minks in Finland. J Clin Microbiol 42:4718-4725
[Crossref] [Googlescholar] [Indexed]
- Lindstrom M, Korkeala H (2006) Laboratory Diagnostics of Botulism. Clin Microbiol Rev 19:298-314
[Crossref] [Googlescholar] [Indexed]
- Long SS, Gajewski JL, Brown LW (1985) Clinical, laboratory and environmental features of infant botulism in Southeastern Pennsylvania. Pediatrics 75:935-941
[Crossref] [Googlescholar] [Indexed]
- Myllykoski J, Linstro M, Keto-Timonen R (2009) Type C bovine botulism outbreak due to carcass contaminated nonacid silage. Epidemiol Infect 137:284-293
[Crossref] [Googlescholar] [Indexed]
- Nakamura K, Kohda T, Umeda K, Yamamoto H, Mukamoto M, et al. (2010) Characterization of the D/C mosaic neurotoxin produced by Clostridium botulinum associated with bovine botulism in Japan. Vet Microbiol 140:147-154
[Crossref] [Googlescholar] [Indexed]
- Neimanis A, Gavier-Wide D, Leighton F, Bollinger T, Rocke T, et al. (2007) An outbreak of type C botulism in herring gulls (Larus argentatus) in Southern Sweden. J Wildl Dis 43:327-336
[Crossref] [Googlescholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences